Abstract
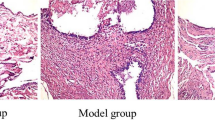
Periodontitis and rheumatoid arthritis (RA) are inflammatory diseases characterized by chronic inflammation and bone erosion. Electroacupuncture (EA) shows anti-inflammatory and anti-resorptive effects in experimental periodontitis (EP) and in RA. It is important to investigate whether EA shows these effects in periodontal tissues in the presence of these two inflammatory diseases or not. For this, Wistar rats were divided into six groups: control (C); experimental rheumatoid arthritis (RA; bovine type II collagen-induced (CII)); experimental periodontitis (EP); RA/EP (RA + EP); EP/EA (EP treated with EA); RA/EP/EA (RA + EP treated with EA). EP was induced 21 days after RA induction and EA was performed previously and during the EP induction period, every 3 days until the 36th experimental day. The rats were euthanized on day 39. RA was evaluated by edema and the withdrawal threshold of hind paws. The maxillae were removed, and alveolar bone loss (ABL) and bone radiographic density (BRD) were evaluated. Immunohistochemical analyses for interleukins (IL)-6 and -17 and nuclear factor (NF)-κB were performed. Our results showed that EA reduced only the pain intensity in arthritic rats. Histomorphometric, macroscopic, and radiographic analyses did not show differences between the control and EP/EA groups. EA caused a reduction in ABL and BRD only in the presence of EP. EA caused a reduction in IL-6 and -17 in all groups, but NF-κB was only reduced in the arthritic rats with EP. In conclusion, EA reduced the inflammation related to periodontitis in arthritic rats but did not prevent ABL.







Similar content being viewed by others
References
Huck, O., N. Buduneli, and D. Bravo. 2019. Inflammatory mediators in periodontal pathogenesis. Mediators of Inflammation 2019: 2610184. https://doi.org/10.1155/2019%2F2610184.
Caton, J.G., G. Armitage , T. Berglundh , I.L.C.Chapple, S. Jepsen, K.S. Kornman, et al. 2018 A new classification scheme for periodontal and peri-implant diseases and conditions- Introduction and key changes from the 1999 classification. Journal of Peridontology 89: S1- S8. https://doi.org/10.1111/jcpe.12935.
Arkema, E.V., E.W. Karlson, and K.H. Costenbader. 2010. A prospective study of periodontal disease and risk of rheumatoid arthritis. Journal of Rheumatology 37: 1800–1804. https://doi.org/10.3899/jrheum.091398.
Havemose-Poulsen, A., J. Westergaard, K. Stoltze, H. Skjodt, B. Danneskiold-Samsøe, H. Locht, et al. 2006. Periodontal and hematological characteristics associated with aggressive periodontitis, juvenile idiopathic arthritis, and rheumatoid arthritis. Journal of Periodontology 77: 280–288. https://doi.org/10.1902/jop.2006.050051.
Fabri, G.M.C., C. Savioli, J.T. Siqueira, L.M. Campos, E. Bonfá, and C.A. Silva. 2014. Periodontal disease in pediatric rheumatic diseases. Revista Brasileira de Reumatologia 54: 311–317. https://doi.org/10.1016/j.rbr.2013.11.004.
Sandal, I., A. Karydis, J. Luo, A. Prislovsky, K.B. Whittington, E.F. Rosloniec, C. Dong, D.V. Novack, P. Mydel, S.G. Zheng, M.Z. Radic, and D.D. Brand. 2016. Bone loss and aggravated autoimmune arthritis in HLA-DRβ1-bearing humanized mice following oral challenge with Porphyromonas gingivalis. Arthritis Research Therapy 18: 249. https://doi.org/10.1186/s13075-016-1143-6.
de Aquino, S.G., J. Talbot, F. Sônego, W.M. Turato, R. Grespan, M.J. Avila-Campos, et al. 2017. The aggravation of arthritis by periodontitis is dependent of IL-17 receptor A activation. Journal of Clinical Periodontology 44: 881–891. https://doi.org/10.1111/jcpe.12743.
S. Kurgan, Ö. Fentoğlu, C. Önder, M. Serdar, F. Eser, D.N. Tatakis, et al. 2016 The effects of periodontal therapy on gingival crevicular fluid matrix metalloproteinase-8, interleukin-6 and prostaglandin E2 levels in patients with rheumatoid arthritis. Journal of Periodontal Research 51:586–595. https://doi.org/10.1111/jre.12337.
Jung, G.U., J.Y. Han, K.G. Hwang, C.J. Park, P.G. Stathopoulou, and J.P. Fiorellini. 2018. Effects of conventional synthetic disease-modifying antirheumatic drugs on response to periodontal treatment in patients with rheumatoid arthritis. BioMed Research International 2018: 1465402.
Chi, L.Q., B. Zhou, W.Y. Gao, and Z. Liu. 2014. Research progress of drugs commonly used to anti-rheumatoid arthritis. Journal of Chinese Materia Medica 39: 2851–2858.
Nanau, R.M., and M.G. Neuman. 2014. Safety of anti-tumor necrosis factor therapies in arthritis patients. Journal of Pharmacy & Pharmaceutical Sciences 17: 324–361. https://doi.org/10.18433/j3wp4f.
Berezow, A.B., and R.P. Darveau. 2011. Microbial shift and periodontitis. Periodontology 2000 (55): 36–47. https://doi.org/10.1111/j.1600-0757.2010.00350.x.
Feres, M., L.C. Figueiredo, G.M.S. Soares and M. Faveri. 2015 Systemic antibiotics in the treatment of periodontitis. Periodontology 2000. 67: 131–186. https://doi.org/10.1111/prd.12075.
Gondim, D.V., J.C.B. Araújo, A.L.C. Cavalcante, A. Havt, J. da S. Quetz, G.A. Brito, et al. 2012. CB1 and CB2 contribute to antinociceptive and anti-inflammatory effects of electroacupuncture on experimental arthritis of the rat temporomandibular joint. Canadian Journal of Physiology and Pharmacology 90: 1479–1489. https://doi.org/10.1139/y2012-130.
Zhang, R., L. Lao, K. Ren, and B.M. Berman. 2014. Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology 120: 482–503. https://doi.org/10.1097/ALN.0000000000000101.
Lisboa, M.R.P., D.V. Gondim, E. Ervolino, M.L. Vale, N.P. Frota, N.L. Nunes, et al. 2015. Effects of electroacupuncture on experimental periodontitis in rats. Journal of Periodontology 86: 801–811. https://doi.org/10.1902/jop.2015.140630.
Alves, L.C.V., M.R.P. Lisboa, H.F. da Silveira, Luane Macêdo de Sousa, J.N.F.M. Gusmão, D.B.S. Dias, et al. 2019. Electroacupuncture increases immunoexpression of CB1 and CB2 receptors in experimental model of inflammatory bone loss. Bone 127: 59–66. https://doi.org/10.1016/j.bone.2019.05.015.
Nielsen, R.H., C. Christiansen, M. Stolina, and M.A. Karsdal. 2008. Oestrogen exhibits type II collagen protective effects and attenuates collagen-induced arthritis in rats. Clinical and Experimental Immunology 152: 21–27 10.1111%2Fj.1365-2249.2008.03594.x.
Goes, P., A.P.S. Lima, I.M. Melo, R.O.C.C. Rêgo, and V. Lima. 2010. Effect of Atorvastatin in radiographic density on alveolar bone loss in wistar rats. Brazilian Dental Journal 21: 193–198. https://doi.org/10.1590/s0103-64402010000300003.
Gondim, D.V., J.L. Costa, S.S. Rocha, Gerly Anne de Castro Brito, Ronaldo de Albuquerque Ribeiro, and M.L. Vale. 2012. Antinociceptive and anti-inflammatory effects of electroacupuncture on experimental arthritis of the rat temporomandibular joint. Canadian Journal of Physiology and Pharmacology 90: 395–405. https://doi.org/10.1139/y2012-003.
Vivancos, G.G., W.A. Verri Jr., T.M. Cunha, I.R. Schivo, C.A. Parada, F.Q. Cunha, and S.H. Ferreira. 2004. An electronic pressure-meter nociception paw test for rats. Brazilian Journal of Medical and Biological Research 37: 391–399. https://doi.org/10.1590/s0100-879x2004000300018.
Martins, C.S., R.F. Leitão, D.V. Costa, I.M. Melo, G.S. Santos, V. Lima, et al. 2016. Topical HPMC/S-nitrosoglutathione solution decreases inflammation and bone resorption in experimental periodontal disease in rats. PLoS One 11: e015371. https://doi.org/10.1371/journal.pone.0153716.
Dias, F.J., V.P.S. Fazan, D.P. Cury, S.R.Y. de Almeida, E. Borie, R., R. Fuentes, J. Coutinho-Netto, I.S. Watanabe 2019 Growth factors expression and ultrastructural morphology after application of low-level laser and natural latex protein on a sciatic nerve crush-type injury. PLoS One 14: e0210211. https://doi.org/10.1371/journal.pone.0210211.
Song, S., J. An, Y. Li, and S. Liu. 2019. Electroacupuncture at ST-36 ameliorates DSS-induced acute colitis via regulating macrophage polarization induced by suppressing NLRP3/IL-1β and promoting Nrf2/HO-1. Molecular Immunology 106: 143–152. https://doi.org/10.1016/j.molimm.2018.12.023.
Bartold, P.M., V. Marino, M. Cantley, and D.R. Haynes. 2010. Effect of Porphyromonas gingivalis-induced inflammation on the development of rheumatoid arthritis. Journal of Clinical Periodontology 37: 405–411. https://doi.org/10.1111/j.1600-051X.2010.01552.x.
Kobayashi, T., T. Yokoyama, K. Ishida, A. Abe, K. Yamamoto, and H. Yoshie. 2010. Serum cytokine and periodontal profiles in relation to disease activity of rheumatoid arthritis in japanese adults. Journal of Periodontology 81: 650–657. https://doi.org/10.1902/jop.2010.090688.
Pers, J.-O., A. Saraux, R. Pierre, and P. Youinou. 2008. Anti–TNF-α immunotherapy is associated with increased gingival inflammation without clinical attachment loss in subjects with rheumatoid arthritis. Journal of Periodontology 79: 1645–1651. https://doi.org/10.1902/jop.2008.070616.
Verzeletti, G.N., E.J. Gaio, and C.K. Rösing. 2007. Effect of methotrexate on alveolar bone loss in experimental periodontitis in Wistar rats. Acta Odontologica Scandinavica 65: 348–351. https://doi.org/10.1080/00016350701742364.
Cetinkaya, B., E. Guzeldemir, E. Ogus, and S. Bulut. 2013. Proinflammatory and anti-inflammatory cytokines in gingival crevicular fluid and serum of patients with rheumatoid arthritis and patients with chronic periodontitis. Journal of Periodontology 84: 84–93. https://doi.org/10.1902/jop.2012.110467.
Srirangan, S., and E.H. Choy. 2010. The role of interleukin 6 in the pathophysiology of rheumatoid arthritis. Therapeutic Advances in Musculoskeletal Diseases 2: 247–256. https://doi.org/10.1177/1759720X10378372.
Batool, H., A. Nadeem, M. Kashif, F. Shahzad, R. Tahir, and N. Afzal. 2018. Salivary levels of IL-6 and IL-17 could be an indicator of disease severity in patients with calculus associated chronic periodontitis. BioMed Research International 2018: 8531961–8531965. https://doi.org/10.1155/2018/8531961.
Ogura, H., M. Murakami, Y. Okuyama, M. Tsuruoka, C. Kitabayashi, M. Kanamoto, et al. 2008. Interleukin-17 promotes autoimmunity by triggering a positive-feedback loop via Interleukin-6 induction. Immunity 29: 628–636. https://doi.org/10.1016/j.immuni.2008.07.018.
Abu-Amer, Y. 2013. NF-κB signaling and bone resorption. Osteoporosis International 24: 2377–2386. https://doi.org/10.1007/s00198-013-2313-x.
Munro, S., K.L. Thomas, and M. Abu-Shaar. 1993. Molecular characterization of a peripheral receptor for cannabinoids. Nature 365: 61–65. https://doi.org/10.1038/365061a0.
Massa, F., G. Marsicano, H. Hermann, A. Cannich, K. Monory, B.F. Cravatt, et al. 2004. The endogenous cannabinoid system protects against colonic inflammation. The Journal of Clinical Investigation 113: 1202–1209. https://doi.org/10.1371/journal.pone.0153716.
Nakajima, Y., Y. Furuichi, K.K. Biswas, T. Hashiguchi, K. Kawahara, K. Yamaji, T. Uchimura, Y. Izumi, and I. Maruyama. 2006. Endocannabinoid, anandamide in gingival tissue regulates the periodontal inflammation through NF-κB pathway inhibition. FEBS Letters 580: 613–619. https://doi.org/10.1016/j.febslet.2005.12.079.
Lee, K., I. Seo, M.H. Choi and D. Jeong, 2018 Roles of mitogen-activated protein kinases in osteoclast biology. International Journal of Molecular Sciences, 19. https://doi.org/10.3390%2Fijms19103004.
Funding
This work was supported by grants from the National Council for Research and Technological Development Process (CNPQ, Brasília, DF, Brazil)—Grant (425181/2016-2).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All efforts were made to minimize the suffering of the animals, as well as the number of animals used in this study, being in accordance with the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. All procedures were performed in accordance with their Animal Care Standards.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
Experimental Protocol. The rheumatoid arthritis was induced by two immunization with CII and IFA. The EA treatment was initiated one day before the second immunization of CII and then every three days until the 36th day. EP was induced on the 28th day. The animals were euthanized on the 39th day. CII = bovine type II collagen; IFA = incomplete Freund’s adjuvant; EA = electroacupuncture treatment; EP = experimental periodontitis. (PNG 33 kb)
Rights and permissions
About this article
Cite this article
Gusmão, J.N.F.M., Fonseca, K.M., Ferreira, B.S.P. et al. Electroacupuncture Reduces Inflammation but Not Bone Loss on Periodontitis in Arthritic Rats. Inflammation 44, 116–128 (2021). https://doi.org/10.1007/s10753-020-01313-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-020-01313-x