Abstract
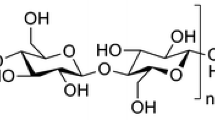
Vascular grafts prepared from synthetic polymers have serious shortcomings that can be resolved by surface modification, such as by immobilizing heparin. In this study, the mechanical properties, biocompatibility, anticoagulation property, and water contact angle of two heparin-conjugated poly(ε-caprolactone) scaffolds (PCL-hexamethylendiamine-heparin, PCL-HMD-H. PCL-lysine-heparin, PCL-LYS-H) were compared to identify a preferred heparin conjugation method. An evaluation of the subcutaneous tissue biocompatibility of the scaffolds demonstrated that PCL-HMD-H had better endothelial cell proliferation than the PCL-LYS-H and was therefore a promising scaffold candidate for use in vascular tissue-engineering.









Similar content being viewed by others
References
Smith SJ, Collins A, Ferrari R, Holmes DJ, Logstrup S, McGhie DV, et al. Our time: a call to save preventable death from cardiovascular disease (heart disease and stroke). Glob Heart. 2012;7:297–305.
Singh C, Wong CS, Wang X. Medical textiles as vascular implants and their success to mimic natural arteries. J Funct Biomater. 2015;6:500–25.
Formichi MJ, Guidoin RG, Jausseran JM, Awad JA, Johnston KW, King MW, et al. Expanded PTFE prostheses as arterial substitutes in humans: late pathological findings in 73 excised grafts. Ann Vasc Surg. 1988;2:14–27.
Avci-Adali M, Paul A, Ziemer G, Wendel HP. New strategies for in vivo tissue engineering by mimicry of homing factors for self-endothelialisation of blood contacting materials. Biomaterials. 2008;29:3936–45.
Wang X, Lin P, Yao Q, Chen C. Development of small-diameter vascular grafts. World J Surg. 2007;31:682–9.
Gui L, Muto A, Chan SA, Breuer CK, Niklason LE. Development of decellularized human umbilical arteries as small-diameter vascular grafts. Tissue Eng Part A. 2009;15:2665–76.
Zou Y, Zhang Y. Mechanical evaluation of decellularized porcine thoracic aorta. J Surg Res. 2012;175:359–68.
Tara S, Kurobe H, Maxfield MW, Rocco KA, Yi T, Naito Y, et al. Evaluation of remodeling process in small-diameter cell-free tissue-engineered arterial graft. J Vasc Surg. 2015;62:734–43.
Lee SJ, Liu J, Oh SH, Soker S, Atala A, Yoo JJ. Development of a composite vascular scaffolding system that withstands physiological vascular conditions. Biomaterials. 2008;29:2891–8.
Khosravi R, Best CA, Allen RA, Stowell C, Onwuka E, Zhuang JJ, et al. Long-term functional efficacy of a novel electrospun poly(glycerol sebacate)-based arterial graft in mice. Ann Biomed Eng. 2016;44:2402–16.
Nottelet B, Pektok E, Mandracchia D, Tille JC, Walpoth B, Gurny R, et al. Factorial design optimization and in vivo feasibility of poly(epsilon-caprolactone)—micro-and nanofiber-based small diameter vascular grafts. J Biomed Mater Res A. 2009;89:865–75.
Dehdilani N, Shamsasenjan K, Movassaghpour A, Akbarzadehlaleh P, Amoughli TB, Parsa H, et al. Improved survival and hematopoietic differentiation of murine embryonic stem cells on electrospun polycaprolactone nanofiber. Cell J. 2016;17:629.
Si J, Cui Z, Wang Q, Liu Q, Liu C. Biomimetic composite scaffolds based on mineralization of hydroxyapatite on electrospun poly(varepsilon-caprolactone)/nanocellulose fibers. Carbohydr Polym. 2016;143:270–8.
Choi WS, Joung YK, Lee Y, Bae JW, Park HK, Park YH, et al. Enhanced patency and endothelialization of small-caliber vascular grafts fabricated by coimmobilization of heparin and cell-adhesive peptides. ACS Appl Mater Interfaces. 2016;8:4336–46.
Chan-Park MB, Shen JY, Cao Y, Xiong Y, Liu Y, Rayatpisheh S, et al. Biomimetic control of vascular smooth muscle cell morphology and phenotype for functional tissue-engineered small-diameter blood vessels. J Biomed Mater Res A. 2009;88:1104–21.
Capila I, Linhardt RJ. Heparin-protein interactions. Angew Chem. 2002;41:391–412.
Castellot JJ, Wong K, Herman B, Hoover RL, Albertini DF, Wright TC, et al. Binding and internalization of heparin by vascular smooth muscle cells. J Cell Physiol. 1985;124:13–20.
Chow LW, Bitton R, Webber MJ, Carvajal D, Shull KR, Sharma AK, et al. A bioactive self-assembled membrane to promote angiogenesis. Biomaterials. 2011;32:1574–82.
Lee JS, Go DH, Bae JW, Lee SJ, Park KD. Heparin conjugated polymeric micelle for long-term delivery of basic fibroblast growth factor. J Control Release. 2007;117:204–9.
Edlund U, Danmark S, Albertsson AC. A strategy for the covalent functionalization of resorbable polymers with heparin and osteoinductive growth factor. Biomacromolecules. 2008;9:901–5.
Cao J, Geng X, Wen J, Li Q, Ye L, Zhang A, et al. The penetration and phenotype modulation of smooth muscle cells on surface heparin modified poly(varepsilon-caprolactone) vascular scaffold. J Biomed Mater Res A. 2017;105:2806–15.
Zhu GC, Gu YQ, Geng X, Feng ZG, Zhang SW, Ye L, et al. Experimental study on the construction of small three-dimensional tissue engineered grafts of electrospun poly-ε-caprolactone. J Mater Sci Mater Med. 2015;26:112.
Ingavle GC, Leach JK. Advancements in electrospinning of polymeric nanofibrous scaffolds for tissue engineering. Tissue Eng Part B Rev. 2014;20:277–93.
Xu Z, Gu Y, Li J, Feng Z, Guo L, Tong Z, et al. Vascular remodeling process of heparin-conjugated poly(epsilon-caprolactone) scaffold in a rat abdominal aorta replacement model. J Vasc Res. 2018;55:338–49.
Wagenseil JE, Mecham RP. Vascular extracellular matrix and arterial mechanics. Physiol Rev. 2009;89:957–89.
Williams C, Liao J, Joyce EM, Wang B, Leach JB, Sacks MS, et al. Altered structural and mechanical properties in decellularized rabbit carotid arteries. Acta Biomater. 2009;5:993–1005.
Pfeiffer D, Stefanitsch C, Wankhammer K, Muller M, Dreyer L, Krolitzki B, et al. Endothelialization of electrospun polycaprolactone (PCL) small caliber vascular grafts spun from different polymer blends. J Biomed Mater Res A. 2014;102:4500–9.
Domingos M, Intranuovo F, Gloria A, Gristina R, Ambrosio L, Bártolo PJ, et al. Improved osteoblast cell affinity on plasma-modified 3-D extruded PCL scaffolds. Acta Biomater. 2013;9:5997–6005.
Cipitria A. Design, fabrication and characterization of PCL electrospun scaffolds—a review. J Mater Chem. 2011;21:9419–53.
Ziyuan C, Swee-Hin T. Surface modification of ultra thin poly (epsilon-caprolactone) films using acrylic acid and collagen. Biomaterials. 2004;25:1991–2001.
Yao Y, Wang J, Cui Y, Xu R, Wang Z, Zhang J, et al. Effect of sustained heparin release from PCL/chitosan hybrid small-diameter vascular grafts on anti-thrombogenic property and endothelialization. Acta Biomater. 2014;10:2739–49.
Gong F, Cheng X, Wang S, Zhao Y, Gao Y, Cai H, et al. Heparin-immobilized polymers as non-inflammatory and non-thrombogenic coating materials for arsenic trioxide eluting stents. Acta Biomater. 2010;6:534–46.
Lu S, Zhang P, Sun X, Gong F, Yang S, Shen L, et al. Synthetic ePTFE grafts coated with an anti-CD133 antibody-functionalized heparin/collagen multilayer with rapid in vivo endothelialization properties. ACS Appl Mater Interfaces. 2013;5:7360–9.
Hoshi RA, Van Lith R, Jen MC, Allen JB, Lapidos KA, Ameer G. The blood and vascular cell compatibility of heparin-modified ePTFE vascular grafts. Biomaterials. 2013;34:30–41.
Baumann H, Kokott A. Surface modification of the polymers present in a polysulfone hollow fiber hemodialyser by covalent binding of heparin or endothelial cell surface heparan sulfate: flow characteristics and platelet adhesion. J Biomater Sci Polym Ed. 2000;11:245–72.
Cheng Q, Komvopoulos K, Li S. Plasma-assisted heparin conjugation on electrospun poly(L-lactide) fibrous scaffolds. J Biomed Mater Res A. 2014;102:1408–14.
Murugesan S, Xie J, Linhardt RJ. Immobilization of heparin: approaches and applications. Curr Top Med Chem. 2008;8.
Biran R, Pond D. Heparin coatings for improving blood compatibility of medical devices [J]. Adv Drug Deliv Rev. 2016;112:12–23.
Ye L, Wu X, Mu Q, Chen B, Duan Y, Geng X, et al. Heparin-conjugated PCL scaffolds fabricated by electrospinning and loaded with fibroblast growth factor 2. J Biomater Sci Polym Ed. 2011;22:389–406.
Jin X, Geng X, Jia L, Xu Z, Ye L, Gu Y, et al. Preparation of small-diameter tissue-engineered vascular grafts electrospun from heparin end-capped PCL and evaluation in a rabbit carotid artery replacement model. Macromol Biosci. 2019;19:e1900114.
Zhao R, Li X, Sun B, Tong Y, Jiang Z, Wang C. Nitrofurazone-loaded electrospun PLLA/sericin-based dual-layer fiber mats for wound dressing applications. RSC Adv. 2015;5:16940–9.
Li Y, Li X, Zhao R, Wang C, Qiu F, Sun B, et al. Enhanced adhesion and proliferation of human umbilical vein endothelial cells on conductive PANI-PCL fiber scaffold by electrical stimulation. Mater Sci Eng C. 2016;72:106–12.
Jiang JH, Zhu LP, Li XL, Xu YY, Zhu BK. Surface modification of PE porous membranes based on the strong adhesion of polydopamine and covalent immobilization of heparin. J Membr Sci. 2010;364:194–202.
Solouk A, Cousins BG, Mirzadeh H, Solatihashtjin M, Najarian S, Seifalian AM. Surface modification of POSS-nanocomposite biomaterials using reactive oxygen plasma treatment for cardiovascular surgical implant applications. Biotechnol Appl Biochem. 2011;58:147–61.
Beamish JA, Geyer LC, Haq-Siddiqi NA, Kottkemarchant K, Marchant RE. The effects of heparin releasing hydrogels on vascular smooth muscle cell phenotype. Biomaterials. 2009;30:6286–94.
Ku SH, Ryu J, Hong SK, Lee H, Par CB. General functionalization route for cell adhesion on non-wetting surfaces. Biomaterials. 2010;31:2535–41.
Dekker A, Reitsma K, Beugeling T, Bantjes A, Feijen J, van Aken WG. Adhesion of endothelial cells and adsorption of serum proteins on gas plasma-treated polytetrafluoroethylene. Biomaterials. 1991;12:130.
Wachem PBV, Hogt AH, Beugeling T, Feijen J, Bantjes A, Detmers JP, et al. Adhesion of cultured human endothelial cells onto methacrylate polymers with varying surface wettability and charge. Biomaterials. 1987;8:323–8.
Ye L, Wu X, Duan HY, Geng X, Chen B, Gu YQ, et al. The in vitro and in vivo biocompatibility evaluation of heparin–poly(ε-caprolactone) conjugate for vascular tissue engineering scaffolds. J Biomed Mater Res A. 2012;100A:3251–8.
Rajangam K, Behanna HA, Hui MJ, Han X, Hulvat JF, Lomasney JW, et al. Heparin binding nanostructures to promote growth of blood vessels. Nano Lett. 2006;6:2086–90.
Hannan RT, Peirce SM, Barker TH. Fibroblasts: diverse cells critical to biomaterials integration. ACS Biomater Sci Eng. 2018;4:1223–32.
Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin Immunol. 2008;20:86–100.
Pascual G, Rodriguez M, Sotomayor S, Perez-Kohler B, Bellon JM. Inflammatory reaction and neotissue maturation in the early host tissue incorporation of polypropylene prostheses. Hernia. 2012;16:697–707.
Acknowledgements
This study was supported by these grants: National Key R&D Program of China (2017YFC1104100), Beijing Clinical Translational Research of Decelluarized Artificial Blood Vessels from the Capital Health Research and Development of Special (2016-1-2012).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xu, Z., Feng, Z., Guo, L. et al. Biocompatibility evaluation of heparin-conjugated poly(ε-caprolactone) scaffolds in a rat subcutaneous implantation model. J Mater Sci: Mater Med 31, 76 (2020). https://doi.org/10.1007/s10856-020-06419-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-020-06419-0