Abstract
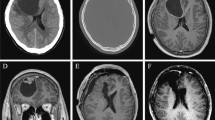
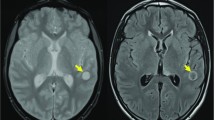
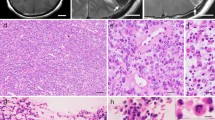
We report a case of 33-year-old Japanese male who presented with a headache and visual disturbances. Magnetic resonance imaging revealed a large tumor in the left frontal lobe, measuring 7 cm in diameter, which was diagnosed as supratentorial anaplastic ependymoma accompanied by extensive desmoplasia. The patient underwent a gross total resection. Histologically, the tumor cells had oval or short, spindle-shaped nuclei, and proliferating cells in perivascular pseudorosettes with anucleate zones and mitotic figures. Desmoplasia with abundant collagen fibers among the tumor cells was detected at numerous sites, and perinuclear dot- or ring-like immunoreactivity for epithelial membrane antigen was identified. Five years and six months after the initial procedure, a small recurrent tumor was identified at the removal site. The patient underwent a second total resection. The histology of the resected tumor showed decreased collagen production and more apparent anaplastic features as compared to those of the initial tumor. In addition to the histological findings, molecular examinations revealed ependymoma, RELA fusion positive. Although not commonly observed, this case suggests that desmoplasia could be associated with ependymomas, including RELA fusion-positive variant. Moreover, our findings indicate that high-grade ependymoma requires careful, long-term follow-up even if gross total resection is performed.



Similar content being viewed by others
References
Louis DN, Ohgaki H, Wiestler OD, et al (2016) WHO classification of tumours of the central nervous system, revised 4th eds. International Agency for Research on Cancer (IARC), Lyon, pp 106–114
Mackay RP (1935) Ependymoblastoma in the fourth ventricle, with new bone formation. Arch Neur Psych 34:844–853
Takahashi H, Goto J, Emura I et al (1998) Lipidized (foamy) tumor cells in a spinal cord ependymoma with collagenous metaplasia. Acta Neuropathol 95:421–425
Yoshida K, Sato K, Kubota T et al (2000) Supratentorial desmoplastic ependymoma with giant ependymal rosettes. Clin Neuropathol 19:186–191
Soeur M, Monseu G, Ketelbant P et al (1979) Intramedullary ependymoma producing collagen. A clinical and pathological study. Acta Neuropathol 47:159–160
Parafeynikov V, Boaz JC, Bonnin JM (2008) Clear-cell ependymoma: A report of intracortical tumor with significant desmoplasia. Neuropathology 28:165–170
Elsharkawy AE, Abuamona R, Bergmann M et al (2013) Cortical anaplastic ependymoma with significant desmoplasia: a case report and literature review. Case Rep Oncol Med 2013:354873
Parker M, Mohankumar KM, Punchihewa C et al (2014) C11orf95–RELA fusions drive oncogenic NF-kB signalling in ependymoma. Nature 506:451–455
Louis DN, Ohgaki H, Wiestler OD, et al (2007) WHO classification of tumours of the central nervous system, 4th eds. International Agency for Research on Cancer (IARC), Lyon, pp 74–80
Aydin F, Ghatak NR, Salvant J et al (1993) Desmoplastic cerebral astrocytoma of infancy. A case report with immunohistochemical, ultrastructural and proliferation studies. Acta Neuropathol 86:666–670
Bianchi F, Tamburrini G (2016) Supratentorial tumors typical of the infantile age: desmoplastic infantile ganglioglioma (DIG) and astrocytoma (DIA). A review Childs Nerv Syst 32:1577–1585
Phi JH, Koh EJ, Kim S-K et al (2011) Desmoplastic infantile astrocytoma: recurrence with malignant transformation into glioblastoma: a case report. Childs Nerv Syst 27:2177–2188
Rodriguez FJ, Scheithauer BW, Perry A et al (2008) Ependymal tumors with sarcomatous change (‘‘ependymosarcoma’’): a clinicopathologic and molecular cytogenetic study. Am J Surg Pathol 32:699–709
Reis RM, Könü-Lebleblicioglu D, Lopes JM et al (2000) Genetic profile of gliosarcomas. Am J Pathol 156:425–432
Walker C, Joyce KA, Thompson-Hehir J (2001) Characterization of molecular alterations in microdissected archival gliomas. Acta Neuropathol 101:321–333
Wang L, Liu L, Li H, Wang P et al (2019) RELA Fusion in Supratentorial extraventricular ependymomas: a morphologic, immunohistochemical, and molecular study of 43 Cases. Am J Surg Pathol 43:1674–1681
Schäfer H, Geismann C, Heneweer C et al (2012) Myofibroblast-induced tumorigenicity of pancreatic ductal epithelial cells is L1CAM dependent. Carcinogenesis 33:84–93
Figarella-Branger D, Lechapt-Zalcman E, Tabouret E et al (2016) Supratentorial clear cell ependymomas with branching capillaries demonstrate characteristic clinicopathological features and pathological activation of nuclear factor-kappaB signaling. Neuro Oncol 18:919–927
Hamilton KR, Lee SS, Urquhart JC et al (2019) A systematic review of outcome in intramedullary ependymoma and astrocytoma. J Clin Neurosci 63:168–175
Ruda R, Reifenberger G, Frappaz D et al (2018) EANO guidelines for the diagnosis and treatment of ependymal tumor. Neuro Oncol 20:445–456
Lee SH, Chung CK, Kim CH et al (2013) Long-term outcomes of surgical resection with or without adjuvant radiation therapy for treatment of spinal ependymoma: a retrospective multicenter study by the Korea Spinal Oncology Research Group. Neuro Oncol 15:921–929
Acknowledgements
The authors would like thank Ms. Junko Kurogi for her excellent technical assistance. The authors also would like to thank Enago (www.enago.jp) for the English language review. This work was supported by Japan Society for the Promotion of Science KAKENHI 17K08764 and a Grant-in-Aid for Clinical Research from Miyazaki University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fukushima, T., Ueda, T., Hirato, J. et al. RELA fusion-positive ependymoma accompanied by extensive desmoplasia: a case report. Brain Tumor Pathol 37, 159–164 (2020). https://doi.org/10.1007/s10014-020-00376-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10014-020-00376-w