Abstract
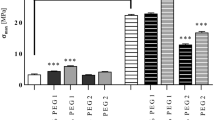
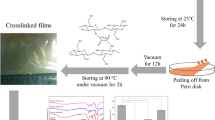
Chitosan-based glycerol-plasticized membranes were prepared aiming to develop low-cost and biocompatible material for wound dressing. They were produced by casting/solvent evaporation, and their formation mechanisms were attributed to intra- and inter-hydrogen bonds between materials. The results show that the glycerol acted as plasticizer and changed the proliferation of fibroblast cells on chitosan membranes. A high increase in the contact angle between water and membrane was observed comparing pure chitosan (more hydrophilic) and chitosan-glycerol (more hydrophobic) membranes. The angle values were found to be ~ 40 and ~ 130 degrees for chitosan and chitosan/glycerol 30% (w/w) membranes, respectively. In comparison with pure chitosan, glycerol-mixed membranes showed lower glass transition temperatures and are less brittle when handling. The antibacterial properties of such membranes against Gram-negative (E. coli) and Gram-positive (S. aureus and B. Cereus) microorganisms were tested, showing efficient growth inhibition. In vitro studies over fibroblast cells using plasticized membranes demonstrated good viability and enhanced cell proliferation in comparison with those composed of pure chitosan. Such results suggest that the as-prepared chitosan-glycerol membrane is a promising material for use as wound dressing in tissue engineering applications.





Similar content being viewed by others
References
Clark RAF, Ghosh K, Tonnesen MG (2007) Tissue engineering for cutaneous wounds. J Invest Dermatol 127:1018–1029. https://doi.org/10.1038/sj.jid.5700715
Madison KC (2003) Barrier function of the skin: “La Raison d’Être” of the epidermis. Epidermal Barrier Funct 121:231–241. https://doi.org/10.1046/j.1523-1747.2003.12359.x
Okonkwo UA, Dipietro LA (2017) Diabetes and wound angiogenesis. Int J Mol Sci 18:1–15. https://doi.org/10.3390/ijms18071419
Cristina A, Gonzalez DO (2016) Wound healing—A literature review *. An Bras Dermatol 91:614–620
Murphy PS, Evans GRD (2012) Advances in wound healing: a review of current wound healing products. Plast Surg Int. https://doi.org/10.1155/2012/190436
Mi F, Shyu S, Wu Y et al (2001) Fabrication and characterization of a sponge-like asymmetric chitosan membrane as a wound dressing. Biomaterials 22:165–173
Mir M, Najabat M, Afifa A et al (2018) Synthetic polymeric biomaterials for wound healing: a review. Prog Biomater 7:1–21. https://doi.org/10.1007/s40204-018-0083-4
Stejskalová A, Almquist BD (2017) Biomaterials science wound repair scholarship to pursue. Biomater Sci 5:1421–1434. https://doi.org/10.1039/c7bm00295e
Azad AK, Sermsintham N, Chandrkrachang S, Stevens WF (2004) Chitosan membrane as a wound-healing dressing: characterization and clinical application. Wiley Period Inc, Hoboken, pp 216–222. https://doi.org/10.1002/jbm.b.30000
He J, Cui WTQHS (2016) Fabrication of silk fibroin/cellulose whiskers – chitosan composite porous scaffolds by layer-by-layer assembly for application in bone tissue engineering. J Mater Sci 51:4399–4410. https://doi.org/10.1007/s10853-016-9752-7
Miguel SP, Moreira AF, Correia IJ (2019) Chitosan based-asymmetric membranes for wound healing: a review. Int J Biol Macromol 127:460–475. https://doi.org/10.1016/j.ijbiomac.2019.01.072
Colobatiu L, Gavan A, Mocan A et al (2019) Development of bioactive compounds-loaded chitosan films by using a QbD approach—A novel and potential wound dressing material. React Funct Polym 138:46–54. https://doi.org/10.1016/j.reactfunctpolym.2019.02.013
Chen X, Zhang M, Wang X et al (2017) Peptide-modified chitosan hydrogels promote skin wound healing by enhancing wound angiogenesis and inhibiting inflammation. Am J Transl Res 9:2352–2362
Ma Y, Xin L, Tan H et al (2017) Materials science & engineering C Chitosan membrane dressings toughened by glycerol to load antibacterial drugs for wound healing. Mater Sci Eng C 81:522–531. https://doi.org/10.1016/j.msec.2017.08.052
Sánchez- DI, López-cervantes J (2014) Chitosan/hydrophilic plasticizer-based films: preparation, physicochemical and antimicrobial properties. J Polym Environ 22:41–51. https://doi.org/10.1007/s10924-013-0621-z
Salgado CL, Sanchez EMS, Mano JF, Moraes AM (2012) Characterization of chitosan and polycaprolactone membranes designed for wound repair application. 659–667. https://doi.org/10.1007/s10853-011-5836-6
Muzzarelli RAA (2009) Chitins and chitosans for the repair of wounded skin, nerve, cartilage and bone. Carbohydr Polym 76:167–182. https://doi.org/10.1016/j.carbpol.2008.11.002
Caetano GF, Frade MAC, Andrade TAM et al (2015) Chitosan-alginate membranes accelerate wound healing. J Biomed Mater Res B Appl Biomater 103:1013–1022. https://doi.org/10.1002/jbm.b.33277
Bakshi PS, Selvakumar D, Kadirvelu K, Kumar NS (2018) Comparative study on antimicrobial activity and biocompatibility of N-selective chitosan derivatives. React Funct Polym 124:149–155. https://doi.org/10.1016/j.reactfunctpolym.2018.01.016
Goy RC, de Britto D, Assis OBG (2009) A review of the antimicrobial activity of chitosan. Polímeros 19:241–247. https://doi.org/10.1590/S0104-14282009000300013
Costa EM, Silva S, Vicente S et al (2017) Chitosan nanoparticles as alternative anti-staphylococci agents: bactericidal, antibiofilm and antiadhesive effects. Mater Sci Eng C 79:221–226. https://doi.org/10.1016/j.msec.2017.05.047
Dallan PRM, da Moreira P LM, Petinari L et al (2007) Effects of chitosan solution concentration and incorporation of chitin and glycerol on dense chitosan membrane properties. J Biomed Mater Res Appl Biomater 80:394–405. https://doi.org/10.1002/jbmb
Matica MA, Aachmann FL, Tondervik A et al (2019) Chitosan as a wound dressing starting material: antimicrobial properties and mode of action. Int J Mol Sci 20:5889–5922
Kumari S, Singh RP (2013) Glycolic acid-functionalized chitosan-Co 3 O 4 -Fe 3 O 4 hybrid magnetic nanoparticles-based nanohybrid scaffolds for drug-delivery and tissue engineering. J Mater Sci 48:1524–1532. https://doi.org/10.1007/s10853-012-6907-z
Kalaiselvimary J, Ramesh Prabhu M (2019) Fabrications and investigation of physicochemical and electrochemical properties of heteropoly acid-doped sulfonated chitosan-based polymer electrolyte membranes for fuel cell applications. Polym Bull 76:1401–1422. https://doi.org/10.1007/s00289-018-2445-4
Merlusca IP, Matiut DS, Lisa G et al (2018) Preparation and characterization of chitosan–poly(vinyl alcohol)–neomycin sulfate films. Polym Bull 75:3971–3986. https://doi.org/10.1007/s00289-017-2246-1
Kumar NVMR (2000) A review of chitin and chitosan applications. React Funct Polym 46:1–27. https://doi.org/10.1016/S1381-5148(00)00038-9
Escárcega-Galaz AA, Sánchez-Machado DI, López-Cervantes J et al (2018) Mechanical, structural and physical aspects of chitosan-based films as antimicrobial dressings. Int J Biol Macromol 116:472–481. https://doi.org/10.1016/j.ijbiomac.2018.04.149
Kenawy E, Omer AM, Tamer TM et al (2019) Fabrication of biodegradable gelatin/chitosan/cinnamaldehyde crosslinked membranes for antibacterial wound dressing applications. Int J Biol Macromol 139:440–448. https://doi.org/10.1016/j.ijbiomac.2019.07.191
Chen M, Runge T, Wang L et al (2018) Hydrogen bonding impact on chitosan plasticization. Carbohydr Polym 200:115–121. https://doi.org/10.1016/j.carbpol.2018.07.062
Pavinatto A, Victoria A, Mattos DA et al (2020) International Journal of Biological Macromolecules Coating with chitosan-based edible fi lms for mechanical/biological protection of strawberries. Int J Biol Macromol 151:1004–1011. https://doi.org/10.1016/j.ijbiomac.2019.11.076
Maria VD, Bernal C, Francois NJ (2017) Development of biodegradable films based on chitosan/glycerol blends suitable for biomedical applications. J Tissue Sci Eng. https://doi.org/10.4172/2157-7552.1000187
Nady N, Kandil SH (2018) Novel blend for producing porous chitosan-based films suitable for biomedical applications. https://doi.org/10.3390/membranes8010002
Souza NLGD, Munk M, Brandão HM, de Oliveira LFC (2018) Functionalization of poly(epichlorohydrin) using sodium hydrogen squarate: cytotoxicity and compatibility in blends with chitosan. Polym Bull 75:4627–4639. https://doi.org/10.1007/s00289-018-2290-5
Follmann HDM, Naves AF, Martins AF et al (2016) Advanced fibroblast proliferation inhibition for biocompatible coating by electrostatic layer-by-layer assemblies of heparin and chitosan derivatives. J Colloid Interf Sci 474:9–17. https://doi.org/10.1016/j.jcis.2016.04.008
Balouiri M, Sadiki M, Ibnsouda SK (2016) Methods for in vitro evaluating antimicrobial activity: a review. J Pharm Anal 6:71–79. https://doi.org/10.1016/j.jpha.2015.11.005
Chen S, Hao Y, Cui W et al (2013) Biodegradable electrospun PLLA/chitosan membrane as guided tissue regeneration membrane for treating periodontitis. J Mater Sci 48:6567–6577. https://doi.org/10.1007/s10853-013-7453-z
Epure V, Griffon M, Pollet E, Avérous L (2011) Structure and properties of glycerol-plasticized chitosan obtained by mechanical kneading. Carbohydr Polym 83:947–952. https://doi.org/10.1016/j.carbpol.2010.09.003
Desbrie J, Brugnerotto J, Lizardi J, et al (2001) An infrared investigation in relation with chitin and chitosan characterization. Polymer (Guildf) 42
Zhang D, Yang S, Zhang K et al (2018) Shape memory effect of chitosan/glycerol composite film in mixed water/ethanol solution. J Appl Polym Sci 47037:1–7. https://doi.org/10.1002/app.47037
Leceta I, Guerrero P, De La Caba K (2013) Functional properties of chitosan-based films. Carbohydr Polym 93:339–346. https://doi.org/10.1016/j.carbpol.2012.04.031
Clinical an Laboratory Standards Institute - CLSI - (2018) Performance standards for antimicrobial disk susceptibility tests, 13th edn. https://clsi.org/standards/products/microbiology/documents/m02/
Matuschek E, Brown DFJ, Kahlmeter G (2014) Development of the EUCAST disk diffusion antimicrobial susceptibility testing method and its implementation in routine microbiology laboratories. Clin Microbiol Infect 20:255–266. https://doi.org/10.1111/1469-0691.12373
Heather E, Foster DS, Longaker MT (2018) Fibroblasts and wound healing: an update. Regen Med 13:491–495
Bainbridge P, Healing W, Repair T (2013) Wound healing and the role of fibroblasts. J Wound Care 22:407–412
Acknowledgments
This study was partly financed by the Coordination for the Improvement in Higher Education Personnel – CAPES - Brazil (Finance Code 001), the São Paulo Research Foundation – FAPESP (Grant number: 2017/19470-8) and the National Council for Scientific and Technological Development – CNPq.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Caroni, J.G., de Almeida Mattos, A.V., Fernandes, K.R. et al. Chitosan-based glycerol-plasticized membranes: bactericidal and fibroblast cellular growth properties. Polym. Bull. 78, 4297–4312 (2021). https://doi.org/10.1007/s00289-020-03310-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00289-020-03310-4