Abstract
Purpose
The purpose of this study was to investigate the clinical outcomes, urinary function, quality of life (QOL), and toxicities in high- or very high-risk prostate cancer patients undergoing single-fraction high-dose-rate brachytherapy (HDR-BT) with external beam radiotherapy (EBRT) and analyze the relationship between dosimetric parameters and toxicities.
Materials and methods
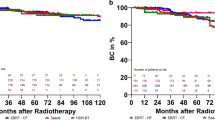
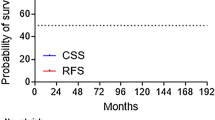
Between April 2014 and April 2019, 124 patients underwent 13-Gy HDR-BT followed by EBRT (46 Gy/23 fractions). Urinary function and QOL were evaluated using IPSS and 7-grade QOL Scale, respectively. Biochemical progression-free survival (bPFS) was calculated.
Results
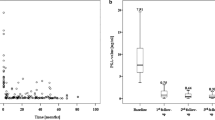
Median follow-up period was 35.8 months; all patients received neoadjuvant hormonal therapy and very high-risk patients received adjuvant hormonal therapy. Only one patient developed a grade 3 toxicity (hematuria). Multivariate analysis showed the dose covering 30% of the urethral volume, bladder volume receiving 75% of the dose, and dose covering 2 cc of rectum were independent predictors of acute G2 urinary frequency, acute G2 urinary retention, and late G2 rectal hemorrhage. IPSS and QOL scores significantly increased following HDR-BT and returned to baseline within 6 months. The 2-year bPFS was 99.2%.
Conclusion
The single-fraction HDR-BT with EBRT is a safe treatment for quicker recovery of urinary symptoms and QOL. The dose of at-risk organs correlated with toxicities.
Secondary abstract
Single-fraction high-dose-rate brachytherapy (HDR-BT) combined with external beam radiotherapy (EBRT) for prostate cancer is a safe treatment allowing for quicker recovery of urinary symptoms and QOL. The dose of at-risk organs correlated with toxicities.



Similar content being viewed by others
Change history
26 January 2021
In the original publication, Toshifumi Gabata should be listed the final author.
References
Cancer Statistics in Japan, Center for Cancer Control and Information Services, National Cancer Center. 2020. Available online: https://ganjoho.jp/reg_stat/statistics/stat/summary.html. Accessed Jan 18, 2020
Cooperberg MR, Broering JM, Carroll PR. Time trends and local variation in primary treatment of localized prostate cancer. J Clin Oncol. 2010;28:1117–23.
Mohler JL, Armstrong AJ, Bahnson RR, D’Amico AV, Davis BJ, Eastham JA, et al. Prostate cancer, version 1. 2016. J Natl Compr Canc Netw. 2016;14:19–30.
Spratt DE, Soni PD, McLaughlin PW, Merrick GS, Stock RG, Blasko JC, et al. American Brachytherapy Society Task Group Report: combination of brachytherapy and external beam radiation for high-risk prostate cancer. Brachytherapy. 2017;16:1–12.
Yamazaki H, Masui K, Suzuki G, Nakamura S, Shimizu D, Nishikawa T, et al. High-dose-rate brachytherapy monotherapy versus image-guided intensity-modulated radiotherapy with helical tomotherapy for patients with localized prostate cancer. Cancers (Basel). 2018;10:E322.
Falk AT, Demontoy S, Chamorey E, Chand ME, Gautier M, Azria D, et al. High-dose-rate brachytherapy boost for prostate cancer: Comparison of three different fractionation schemes. Brachytherapy. 2017;16:993–9.
Hijazi H, Chevallier D, Gal J, Chand ME, Gautier M, Hannoun-Levi JM. Prostate cancer boost using high-dose-rate brachytherapy: early toxicity analysis of 3 different fractionation schemes. J Contemp Brachytherapy. 2013;5:203–9.
Lauche O, Delouya G, Taussky D, Menard C, Béliveau-Nadeau D, Hervieux Y, et al. Single-fraction high-dose-rate brachytherapy using real-time transrectal ultrasound based planning in combination with external beam radiotherapy for prostate cancer: dosimetrics and early clinical results. J Contemp Brachytherapy. 2016;8:104–9.
Boladeras A, Santorsa L, Gutierrez C, Martinez E, Pera J, Pino F, et al. External beam radiotherapy plus single-fraction high dose rate brachytherapy in the treatment of locally advanced prostate cancer. Radiother Oncol. 2014;112:227–32.
Morton GC, Loblaw DA, Sankreacha R, Deabreu A, Zhang L, Mamedov A, et al. Single-fraction high-dose-rate brachytherapy and hypofractionated external beam radiotherapy for men with intermediate-risk prostate cancer: analysis of short- and medium-term toxicity and quality of life. Int J Radiat Oncol Biol Phys. 2010;77:811–7.
Pistis F, Guedea F, Pera J, Gutierrez C, Ventura M, Polo A, et al. External beam radiotherapy plus high-dose-rate brachytherapy for treatment of locally advanced prostate cancer: the initial experience of the Catalan Institute of Oncology. Brachytherapy. 2010;9:15–22.
Büchser D, Casquero F, Espinosa JM, Perez F, Minguez P, Martinez-Indart L, et al. Late toxicity after single dose HDR prostate brachytherapy and EBRT for localized prostate cancer: Clinical and dosimetric predictors in a prospective cohort study. Radiother Oncol. 2019;135:13–8.
Martell K, Mendez LC, Chung HT, Tseng CL, Alayed Y, Cheung P, et al. Results of 15 Gy HDR-BT boost plus EBRT in intermediate-risk prostate cancer: analysis of over 500 patients. Radiother Oncol. 2019;141:149–55.
Shahid N, Loblaw A, Chung HT, Cheung P, Szumacher E, Danjoux C, et al. Long-term toxicity and health-related quality of life after single-fraction high dose rate brachytherapy boost and hypofractionated external beam radiotherapy for intermediate-risk prostate cancer. Clin Oncol (R Coll Radiol). 2017;29:412–20.
Chicas-Sett R, Farga D, Perez-Calatayud MJ, Celada F, Roldan S, et al. High-dose-rate brachytherapy boost for prostate cancer: analysis of dose-volume histogram parameters for predicting late rectal toxicity. Brachytherapy. 2017;16:511–7.
Kragelj B, Zlatic J, Zaletel-Kragelj L. Avoidance of late rectal toxicity after high-dose-rate brachytherapy boost treatment for prostate cancer. Brachytherapy. 2017;16:193–200.
Yamada Y, Rogers L, Demanes DJ, Morton G, Prestidge BR, Pouliot J, et al. American Brachytherapy Society consensus guidelines for high-dose-rate prostate brachytherapy. Brachytherapy. 2012;1:20–322.
Hoskin PJ, Colombo A, Henry A, Niehoff P, Paulsen Hellebust T, Siebert FA, et al. GEC/ESTRO recommendations on high dose rate afterloading brachytherapy for localised prostate cancer: an update. Radiother Oncol. 2013;3:325–32.
Wilder RB, Chittenden L, Mesa AV, Bunyapanasarn J, Agustin J, Lizarde J, et al. A prospective study of intrafraction prostate motion in the prone vs. supine position. Int J Radiat Oncol Biol Phys. 2010;77:165–70.
Ikeda I, Mizowaki T, Sawada Y, Nakata M, Norihisa Y, Ogura M, et al. Assessment of interfractional prostate motion in patients immobilized in the prone position using a thermoplastic shell. J Radiat Res. 2014;55:168–74.
Roach M III, Hanks G, Thames H Jr, Schellhammer P, Shipley WU, Sokol GH, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys. 2006;65:965–74.
Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Kim Y, Hsu IC, Pouliot J. Measurement of craniocaudal catheter displacement between fractions in computed tomography-based high dose rate brachytherapy of prostate cancer. J Appl Clin Med Phys. 2007;8:2415.
Tiong A, Bydder S, Ebert M, Caswell N, Waterhouse D, Spry N, et al. A small tolerance for catheter displacement in high-dose rate prostate brachytherapy is necessary and feasible. Int J Radiat Oncol Biol Phys. 2010;76:1066–72.
Yoshida K, Yamazaki H, Nose T, Shiomi H, Yoshida M, Mikami M, et al. Needle applicator displacement during high-dose-rate interstitial brachytherapy for prostate cancer. Brachytherapy. 2010;9:36–41.
Fowler J, Chappell R, Ritter M. Is alpha/beta for prostate tumors really low? Int J Radiat Oncol Biol Phys. 2001;50:1021–31.
Brenner DJ, Martinez AA, Edmundson GK, Mitchell C, Thames HD, Armour EP. Direct evidence that prostate tumors show high sensitivity to fractionation (low alpha/beta ratio), similar to late-responding normal tissue. Int J Radiat Oncol Biol Phys. 2002;52:6–13.
Löser A, Beyer B, Carl CO, Löser B, Nagaraj Y, Frenzel T, et al. Toxicity and risk factors after combined high-dose-rate brachytherapy and external beam radiation therapy in men ≥75 years with localized prostate cancer. Strahlenther Onkol. 2019;195:374–82.
Tanimoto R, Bekku K, Katayama N, Kobayashi Y, Ebara S, Araki M, et al. Predictive factors for acute and late urinary toxicity after permanent interstitial brachytherapy in Japanese patients. Int J Urol. 2013;20:812–7.
Li X, Fang D, Cooperberg MR, Whitson JM, Lue TF, Zhou L, et al. Long-term follow-up of International Prostate Symptom Score (IPSS) in men following prostate brachytherapy. World J Urol. 2014;32:1061–6.
Miyake M, Tanaka N, Asakawa I, Hori S, Morizawa Y, Tatsumi Y, et al. Assessment of lower urinary symptom flare with overactive bladder symptom score and International Prostate Symptom Score in patients treated with iodine-125 implant brachytherapy: long-term follow-up experience at a single institute. BMC Urol. 2017;17:62.
Sanmamed N, Chung P, Berlin A, Adleman J, Borg J, Lao B, et al. Dose to the bladder neck in MRI-guided high-dose-rate prostate brachytherapy: impact on acute urinary toxicity and health-related quality of life. Brachytherapy. 2019;18:477–83.
Heidenreich A, Ohlmann CH, Polyakov S. Anatomical extent of pelvic lymphadenectomy in patients undergoing radical prostatecomy. Eur Urol. 2007;52:29–37.
Dirix P, Joniau S, Van den Bergh L, Isebaert S, Oyen R, Deroose CM, et al. The role of elective pelvic radiotherapy in clinically node-negative prostate cancer: a systematic review. Radiother Oncol. 2014;110:45–544.
Tharmalingam H, Tsang Y, Choudhury A, Alonzi R, Wylie J, Ahmed I, et al. External beam radiation therapy (EBRT) and high-dose-rate (HDR) brachytherapy for intermediate and high-risk prostate cancer: the impact of EBRT volume. Int J Radiat Oncol Biol Phys. 2020;106:525–33.
Acknowledgments
The authors thank all the staff in the radiotherapy section, all the urologists in our institution and all of the patients who participated in the study for their understanding and support. We would like to thank Editage (www.editage.com) for English language editing. This paper was presented at the 61st American Society for Radiation Oncology Annual Meeting on September 15-18, 2019.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: Takayuki Sakurai, Shigeyuki Takamatsu, and Tomoyasu Kumano; Methodology: Takayuki Sakurai and Shigeyuki Takamatsu; Validation: Takayuki Sakurai, Shigeyuki Takamatsu, and Toshifumi Gabata; Formal analysis: Takayuki Sakurai; Investigation: Takayuki Sakurai, Shigeyuki Takamatsu, Satoshi Shibata, Koji Iwata, Masashi Taka, Tomoyasu Kumano, Tomoyuki Makino, and Atsushi Mizokami; Resources: Takayuki Sakurai and Shigeyuki Takamatsu; Data curation: Takayuki Sakurai and Shigeyuki Takamatsu; Writing—original draft preparation: Takayuki Sakurai; Writing—review and editing: Takayuki Sakurai, Shigeyuki Takamatsu, and Tomoyasu Kumano; Visualization: Takayuki Sakurai; Supervision: Takayuki Sakurai; Project administration: Tomoyasu Kumano and Toshifumi Gabata. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical statement
Informed consent was obtained from all individual participants included in the study. This retrospective study was approved by the institutional review board of Kanazawa university hospital [approval: # 2016-326 (2074)]. All applicable institutional and/or national guidelines for the care were followed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Sakurai, T., Takamatsu, S., Shibata, S. et al. Toxicity and clinical outcomes of single-fraction high-dose-rate brachytherapy combined with external beam radiotherapy for high-/very high-risk prostate cancer: A dosimetric analysis of toxicity. Jpn J Radiol 38, 1197–1208 (2020). https://doi.org/10.1007/s11604-020-01023-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-020-01023-2