Abstract
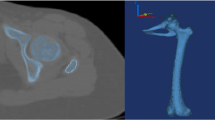
Bone structure can change by remodeling to adapt to mechanical status. Such change can result in bone affecting the long-term stability of the stem. The objective of this study was to propose a method to evaluate mechanical adaptation for preoperative planning of total hip arthroplasty. Finite element models of preoperative planning were examined in two ways: bone remodeling simulation and initial mechanical status of femur. A mathematical model of remodeling for long-term changes of bone was developed assuming that bone resorption/formation could be distinguished by strain magnitude of bone. Also, initial compatibility between stem and bone was set with four strain levels based on mechanostat theory. The results of bone remodeling simulation were shown average equivalent stress change was mainly observed in Gruen zone 1 and zone 7 where stress shielding or bone resorption could occur. The proportion of this value was the smallest in the first choice of the stem by a specialist surgeon. Also, these are showed same tendency with evaluation of initial strain distribution results that Gruen zone 1 and 7. Initial strain distribution after total hip arthroplasty was correlated with the long-term change of bone structures after total hip arthroplasty. Bone structure changes around prostheses occur due to changes in the mechanical environment, and this is correlated with strain distribution of immediate post-operative model. Findings of this study suggest that biomechanical indices might be useful for exploring difference in long-term fitting among different surgical plans.







Similar content being viewed by others
References
Klein-Nulend, J., Bacabac, R. G., & Mullender, M. G. (2001). Mechanobiology of bone tissue. Pathologie-Biologie, 53, 576–580.
Hughes, J. (2010). Biological underpinnings of Frost’s mechanostat thresholds: the important role of osteocytes. Journal of Musculoskelet Neuronal Interact, 10(April), 128–135.
Kaneps, A. J., Stover, S. M., & Lane, N. E. (1997). Changes in canine cortical and cancellous bone mechanical properties following immobilization and remobilization with exercise. Bone, 21(5), 419–423.
Frost, H. M. (2003). Bone’s mechanostat: a 2003 update. The Anatomical Record. Part A, Discoveries in Molecular, Cellular, and Evolutionary Biology, 275(2), 1081–1101.
Gu, G., Mulari, M., Peng, Z., Hentunen, T. A., & Väänänen, H. K. (2005). Death of osteocytes turns off the inhibition of osteoclasts and triggers local bone resorption. Biochemical and Biophysical Research Communications, 335(4), 1095–1101.
Tanck, E., Ruimerman, R., & Huiskes, R. (2006). Trabecular architecture can remain intact for both disuse and overload enhanced resorption characteristics. Journal of Biomechanics, 39(14), 2631–2637.
Skerry, T. M. (2008). The response of bone to mechanical loading and disuse: fundamental principles and influences on osteoblast/osteocyte homeostasis. Archives of Biochemistry and Biophysics, 473(2), 117–123.
Makarand, G., Joshi, S., Adavani, F., & Michael, H. (2000). Analysis of a femoral hip prosthesis designed to reduce stress shielding. Journal of Biomechanics, 33, 1655–1662.
Smolders, J. M. H., Hol, A., Rijnders, T., & van Susante, J. L. C. (2010). Changes in bone mineral density in the proximal femur after hip resurfacing and uncemented total hip replacement: A prospective randomised controlled study. The Journal of Bone and Joint Surgery British, 92(11), 1509–1514.
Sumner, D. R. (2015). Long-term implant fixation and stress-shielding in total hip replacement. Journal of Biomechanics, 48(5), 787–800.
Affatato, S., Zanini, F., & Carmignato, S. (2017). Micro X-ray computed tomography mass loss assessment of different UHMWPE: a hip joint simulator study on standard vs. cross-linked polyethylene. PLoS ONE, 12(1), e0170263.
Annapaola, P., Stefano, F., Milena, F., & Saverio, A. (2016). Is micro-computed tomography useful for wear assessment of ceramic femoral heads? A preliminary evaluation of volume measurements. Journal of Applied Biomaterials & Fundamental Materials, 14(4), e483–e489.
Kassi, J.-P., Heller, M. O., Stoeckle, U., Perka, C., & Duda, G. N. (2005). Stair climbing is more critical than walking in pre-clinical assessment of primary stability in cementless THA in vitro. Journal of Biomechanics, 38(5), 1143–1154.
Rondon, A., Sariali, E., Vallet, Q., & Grimal, Q. (2017). Modal analysis for the assessment of cementless hip stem primary stability in preoperative THA planning. Medical Engineering & Physics, 49, 79–88.
Kim, S. Y., Park, S., Park, Y. S., et al. (2015). Primary stability evaluation of a hip-joint implant systems according to different surgical methods and bone densities under cyclic loading condition. International journal of Precision Engineering and Manufacturing, 16(6), 1094–1100.
Ehrlich, P. J., & Lanyon, L. E. (2002). Mechanical strain and bone cell function: A review introduction: The strain-adaptive response of bone. Osteoporosis International, 13, 688–700.
Liedert, A., Kaspar, D., Blakytny, R., Claes, L., & Ignatius, A. (2006). Signal transduction pathways involved in mechanotransduction in bone cells. Biochemical and Biophysical Research Communications, 349(1), 1–5.
Coelho, P. G., Rodrigues, H. C., & Fernandes, P. R. (2008). Bone tissue adaptation—A hierarchical approach for apparent density and trabecular structure. Journal of Biomechanics, 41(1), S125.
Fernandes, P. R., Folgado, J., Jacobs, C., & Pellegrini, V. (2002). A contact model with ingrowth control for bone remodelling around cementless stems. Journal of Biomechanics, 35(2), 167–176.
Huiskes, R. (2000). If bone is the answer, then what is the question? Journal of Anatomy, 197(2), 145–156.
McNamara, L. M., & Prendergast, P. J. (2007). Bone remodelling algorithms incorporating both strain and microdamage stimuli. Journal of Biomechanics, 40(6), 1381–1391.
Mullender, M. G., & Huiskes, R. (1995). Proposal for the regulatory mechanism of Wolff’s law. Journal of Orthopedic Research, 13(4), 503–512.
Smith, T. S., Martin, R. B., Hubbard, M., & Bay, B. K. (1997). Surface remodeling of trabecular bone using a tissue level model. Journal of Orthopaedic Research, 15(4), 593–600.
Weinkamer, R., Hartmann, M. A., Brechet, Y., & Fratzl, P. (2004). Stochastic lattice model for bone remodeling and aging. Physical Review Letters, 93, 228102.
Duchmin, L., Bousson, V., Raossanaly, C., Bergot, C., Laredo, J., Skalli, W., et al. (2008). Prediction of mechanical properties of cortical bone by quantitative computed tomography. Medical Engineering & Physics, 30, 321–328.
Beaupré, G. S., Orr, T. E., & Carter, D. R. (1990). An approach for time-dependent bone modeling-application: A preliminary remodeling simulation. Journal of Orthopaedic Research, 8(5), 662–670.
Adachi, T., Tomita, Y., Sakaue, H., & Tanaka, M. (1997). Simulation of trabecular surface remodeling based on local stress nonuniformity. JSME International Series C, 40(4), 782–792.
Tsubota, K., Suzuki, Y., Yamada, T., Hojo, M., Makinouchi, M., & Adachi, T. (2009). Computer simulation of trabecular remodeling in human proximal femur using large-scale voxel FE models: approach to understanding Wolff’s law. Journal of Biomechanics, 42, 1088–1094.
Adachi, T., Tsubota, K., Tomita, Y., & Hollister, S. J. (2001). Trabecular surface remodeling simulation for cancellous bone using microstructural voxel finite element models. Journal of Biomechanical Engineering, 123(5), 403.
Kwon, J., Naito, H., Matsumoto, T., & Tanaka, M. (2010). Simulation model of trabecular bone remodeling considering effects of osteocyte apoptosis and targeted remodeling. Journal of Biomechanical Science and Engineering, 5(5), 539–551.
Cowin, S. C., Moss-Salentijn, L., & Moss, M. L. (1991). Candidates for the mechanosensory system in bone. Journal of Biomechanical Engineering, 113, 191–197.
Bacabac, R. G., Van Loon, J. J. W. A., & Klein-Nulend, J. (2007). Microgravity and bone cell mechanosensitivity. Biology in Space and Life on Earth: Effects of Spaceflight on Biological Systems, 22(5), 157–177.
Kwon, J., Naito, H., Matsumoto, T., & Tanaka, M. (2010). Computational study on trabecular bone remodeling in human femur under reduced weight-bearing conditions. Journal of Biomechanical Science and Engineering, 5(5), 552–564.
Engh, C., McGovern, T., & Harris, W. (1992). A quantitative evaluation of periprosthetic bone-remodeling after cementless total hip arthroplasty. Journal of Bone and Joint Surgery, 74, 1009–1020.
Engh, C., Hooten, J., Jr., Zettl-Schaffer, K., Ghaffarpour, M., McGovern, T., Macalino, G., et al. (1994). Porous-coated total hip replacement. Clinical Orthopaedics and Related Research, 298, 89–96.
Herrera, A., Panisello, J. J., Ibarz, E., Cegoñino, J., Puértolas, J. A., & Gracia, L. (2007). Long-term study of bone remodelling after femoral stem: a comparison between dexa and finite element simulation. Journal of Biomechanics, 40(16), 3615–3625.
Viceconti, M., Lattanzi, R., Antonietti, B., Paderni, S., Olmi, R., Sudanese, A., et al. (2003). CT-based surgical planning software improves the accuracy of total hip replacement preoperative planning. Medical Engineering & Physics, 25(5), 371–377.
Pancanti, A., Bernakiewicz, M., & Viceconti, M. (2003). The primary stability of a cementless stem varies between subjects as much as between activities. Journal of Biomechanics, 36(6), 777–785.
Otomaru, I., Nakamoto, M., Takao, M., Sugano, N., Kagiyama, Y., Yoshikawa, H., et al. (2008). Automated preoperative planning of femoral component for total hip arthroplasty (THA) from 3D CT images. Journal of Biomechanical Science and Engineering, 3(4), 478–489.
Alessandro, R., Roberto, D., & Saverio, A. (2019). Comparison of meshing strategies in THR finite element modelling. Materials, 12, 2332.
Ruggiero, A., Merola, M., & Affatato, S. (2018). Finite element simulations of hard-on-soft hip joint prosthesis accounting for dynamic loads calculated from a musculoskeletal model during walking. Materials, 11, 574.
Alejandro, D., Douglas, P., & Eduardo, S. (2005). Preoperative planning for primary total hip arthroplasty. Journal of the American Academy of Orthopaedic Surgeons, 13(7), 455–462.
Heather, P., Maria, I., Anshuman, S., Robert, N., & Elizabeth, P. (2019). Preoperative risk factors for opioid utilization after total hip arthroplasty. The Journal of Bone and Joint Surgery, 101(18), 1670–1678.
Boisgard, S., Descamps, S., & Bouillet, B. (2013). Complex primary total hip arthroplasty. Orthopaedics & Traumatology: Surgery & Research, 99(1), S34–S42.
Acknowledgements
This research was supported by the training program for advanced medical device industry professional manpower of Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health and Welfare, Republic of Korea. The authors would like to thank Prof. Yoshinobu Sato, Dr. Masaki Takao and Ph.D. Itaru Otomaru at Medical School of Osaka University for providing the preoperative planning CT-image data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kwon, J.Y., Kim, S.M. & Tanaka, M. Evaluation of Mechanical Adaptation on Preoperative Planning for Total Hip Arthroplasty. Int. J. Precis. Eng. Manuf. 21, 1975–1983 (2020). https://doi.org/10.1007/s12541-020-00390-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12541-020-00390-0