Abstract
Purpose
Atherosclerosis preferentially occurs near the junction of branching vessels, where blood recirculation tends to occur (Malek et al. in J Am Med Assoc 282(21):2035–2042, 1999, https://doi.org/10.1001/jama.282.21.2035). For decades, CFD has been used to predict flow patterns such as separation and recirculation zones in hemodynamic models, but those predictions have rarely been validated with experimental data. In the context of verification and validation (V&V), we first conduct a CFD benchmark calculation that reproduces the vortex detection experiments of Karino and Goldsmith (1980) with idealised branching blood vessels (Karino and Goldsmith in Trans. Am. Soc. Artif. Internal Organs 26:500–506, 1980). The critical conditions for the formation of recirculation vortices, the so-called critical Reynolds numbers, are the main parameters for comparison with the experimental data to demonstrate the credibility of the CFD workflow. We then characterise the wall shear stresses and develop a surrogate model for the size of formed vortices.
Methods
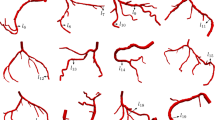
An automated parametric study generating more than 12,000 CFD simulations was performed, sweeping the geometries and flow conditions found in the experiments by Karino and Goldsmith. The flow conditions were restricted to steady-state laminar flow, with a range of inflow Reynolds numbers up to 350, with various flow ratios between the main branch outlet and side branch outlet. The side branch diameter was scaled relative to the main branch diameter, ranging from 1.05/3 to 3/3; and the branching angles ranged in size from \({45}^\circ\) to \(135^\circ\). Recirculation vortices were detected by the inversion of the velocity vector at certain locations, as well as by the inversion of the wall shear stress (WSS) vector.
Results
The CFD simulations demonstrated good agreement with the experimental data on the critical Reynolds numbers. The spatial distributions of WSS on each branch were analysed to identify potential regions of disease. Once a vortex is formed, the size of the vortex increases by the square root of the Reynolds number. The CFD data was fitted to a surrogate model that accurately predicts the vortex size without the need to run computationally more expensive CFD simulations.
Conclusions
This benchmark study validates the CFD simulation of vortex detection in idealised branching vessels under comprehensive flow conditions. This work also proposes a surrogate model for the size of the vortex, which could reduce the computational requirements in the studies related to branching vessels and complex vascular systems.














Similar content being viewed by others
References
Adams, B. M., M. S. Ebeida, M. S. Eldred, J. D. Jakeman, L. P. Swiler, J. Adam Stephens, D. M. Vigil, T. M. Wildey, W. J. Bohnhoff, K. R. Dalbey, J. P. Eddy, R. W. Hooper, K. T. Hu, L. E. Bauman, P. D. Hough, and A. Rushdi. Dakota, a multilevel parallel object-oriented framework for design optimization, parameter estimation, uncertainty quantification, and sensitivity analysis: Version 6.3 user’s manual. Technical report, National Technology and Engineering Solutions of Sandia, LLC, USA, 2015. https://dakota.sandia.gov//sites/default/files/docs/6.3/Users-6.3.0.pdf.
Antiga, L., and D. A. Steinman. Robust and objective decomposition and mapping of bifurcating vessels. Circ. Res. 23(6):704–713, 2004. https://doi.org/10.1109/TMI.2004.826946.
Asakura, T., and T. Karino. Flow patterns and spatial distribution of atherosclerotic lesions in human coronary arteries. Circ. Res. 66(4):1045–1066, 1990. https://doi.org/10.1161/01.RES.66.4.1045.
ASME. Assessing credibility of computational modeling through verification and validation: application to medical devices, 2019. https://www.asme.org/products/codes-standards/vv-40-2018-assessing-credibility-computational.
Borse, M., S. Bhushan, D. K. Walters, and G. W. Burgreen. Numerical simulations of flow pattern and particle trajectories in feline aorta for hypertrophic cardiomyopathy heart conditions. Eng. Appl. Comput. Fluid Mech. 12(1):57–73, 2018. https://doi.org/10.1080/19942060.2017.1339640.
Browne, L. D., K. Bashar, P. Griffin, E. G. Kavanagh, S. R. Walsh, and M. T. Walsh. The role of shear stress in arteriovenous fistula maturation and failure: a systematic review. PLoS ONE 10(12):1–24, 2015. https://doi.org/10.1371/journal.pone.0145795.
Bureau, M., J. Healy, D. Bourgoin, and M. Joly. Rheological hysteresis of blood at low shear rate. Biorheology 17(1–2):191–203, 1980.
Caro, C. G., J. M. Fitz-Gerald, and R. C. Schroter. Atheroma and arterial wall shear—observation, correlation and proposal of a shear dependent mass transfer mechanism for atherogenesis. Proc. R. Soc. Lond. B 177(1046):109–133, 1971. https://doi.org/10.1098/rspb.1971.0019.
Cecchi, E., C. Giglioli, S. Valente, C. Lazzeri, G. F. Gensini, R. Abbate, and L. Mannini. Role of hemodynamic shear stress in cardiovascular disease. Atherosclerosis 214(2):249–256, 2011. https://doi.org/10.1016/j.atherosclerosis.2010.09.008.
Chiu, J., and S. Chien. Effects of disturbed flow on vascular endothelium: pathophysiological basis and clinical perspectives. Physiol. Rev. 91(1):327–387, 2011. https://doi.org/10.1152/physrev.00047.2009.
Cho, Y. I., and K. R. Kensey. Effects of the non-Newtonian viscosity of blood on flows in a diseased arterial vessel. Part 1: steady flows. Biorheology 28(3–4):241–262, 1991. https://doi.org/10.3233/BIR-1991-283-415.
Ene-Iordache, B., and A. Remuzzi. Disturbed flow in radial-cephalic arteriovenous fistulae for haemodialysis: low and oscillating shear stress locates the sites of stenosis. Nephrol. Dial. Transplant. 27(1):358–368, 2012. https://doi.org/10.1093/ndt/gfr342.
Gundert, T. J., A. L. Marsden, W. Yang, and J. F. LaDisa, Jr. Optimization of cardiovascular stent design using computational fluid dynamics. J. Biomech. Eng. 134(1):011002, 2012. https://doi.org/10.1115/1.4005542.
He, X., and D. N. Ku. Flow in t-bifurcations: effect of the sharpness of the flow divider. Biorheology 32(4):447–458, 1995. https://doi.org/10.1016/0006-355X(95)00022-2.
Hellmuth, R., M. S. Bruzzi, and N. J. Quinlan. Analysis of shear-induced platelet aggregation and breakup. Ann. Biomed. Eng. 44(4):914–928, 2016. https://doi.org/10.1007/s10439-015-1409-1.
Institute, T. H. R. What is atherosclerosis? Online, 2019. https://www.hriuk.org/about-heart-disease/what-is-atherosclerosis.
Kalpakli, A., R. Örlü, N. Tillmark, and P. H. Alfredsson. Pulsatile turbulent flow through pipe bends at high Dean and Womersley numbers. J. Phys. Conf. Ser. 2011. https://doi.org/10.1088/1742-6596/318/9/092023.
Karino, T., and H. L. Goldsmith. Disturbed flow in models of branching vessels. Trans. Am. Soc. Artif. Internal Organs 26:500–506, 1980.
Kazakidi, A., A. M. Plata, S. J. Sherwin, and P. D. Weinberg. Effect of reverse flow on the pattern of wall shear stress near arterial branches. J. R. Soc. Interface 8(64):1594–1603, 2011. https://doi.org/10.1098/rsif.2011.0108.
Kazakidi, A., S. J. Sherwin, and P. D. Weinberg. Effect of Reynolds number and flow division on patterns of haemodynamic wall shear stress near branch points in the descending thoracic aorta. J. R. Soc. Interface 6(35):539–548, 2009. https://doi.org/10.1098/rsif.2008.0323.
Kratzer, M. A. A., and J. Kinder. Streamline pattern and velocity components of flow in a model of a branching coronary vessel-possible functional implication for the development of localized platelet deposition in Vitro. Microvasc. Res. 31(2):250–265, 1986. https://doi.org/10.1016/0026-2862(86)90038-5.
Ku, J. P., M. T. Draney, F. R. Arko, W. A. Lee, F. P. Chan, N. J. Pelc, C. K. Zarins, and C. A. Taylor. In vivo validation of numerical prediction of blood flow in arterial bypass grafts. Ann. Biomed. Eng. 30(6):743–752, 2002. https://doi.org/10.1114/1.1496086.
Lei, M., D. P. Giddens, S. A. Jones, F. Loth, and H. Bassiouny. Pulsatile flow in an end-to-side vascular graft model: comparison of computations with experimental data. J. Biomech. Eng. 123(1):80–87, 2001. https://doi.org/10.1115/1.1336145.
Libby, P., P. M. Ridker, and G. K. Hansson. Progress and challenges in translating the biology of atherosclerosis. Nature 473(7347):317–325, 2011. https://doi.org/10.1038/nature10146.
Malek, A. M., S. L. Alper, and S. Izumo. Hemodynamic shear stress and its role. J. Am. Med. Assoc. 282(21):2035–2042, 1999. https://doi.org/10.1001/jama.282.21.2035.
Marsden, A. L. Optimization in cardiovascular modeling. Annu. Rev. Fluid Mech. 46(1):519–546, 2014. https://doi.org/10.1146/annurev-fluid-010313-141341.
Patankar, S., and D. Spalding. A calculation procedure for heat, mass and momentum transfer in three-dimensional parabolic flows. Int. J. Heat Mass Transf. 15(10):1787–1806, 1972. https://doi.org/10.1016/0017-9310(72)90054-3.
Pedley, T. J., and X. Luo. Fluid mechanics of large blood vessels. Xi’an: Shaanxi People’s Press, 1995.
Schneiders, R. Octree-based hexahedral mesh generation. Int. J. Comput. Geometry Appl. 10(4):383–398, 2000. https://doi.org/10.1142/S021819590000022X.
Shaaban, A. M., and A. J. Duerinckx. Wall shear stress and early atherosclerosis: a review. Am. J. Roentgenol. 174(6):1657–1665, 2000.
Shin, D. H., R. Sandberg, and E. Richardson. Self-similarity of fluid residence time statistics in a turbulent round jet. J. Fluid Mech. 823:1–25, 2017.
Sousa, L. C., C. F. Castro, C. C. Antonio, and R. Chaves. Blood flow simulation and vascular reconstruction. J. Biomech. 45(15):2549–2555, 2012. https://doi.org/10.1016/j.jbiomech.2012.07.033.
Steinman, D. A., and F. Migliavacca. Editorial: Special issue on verification, validation, and uncertainty quantification of cardiovascular models: towards effective VVUQ for translating cardiovascular modelling to clinical utility. Cardiovasc. Eng. Technol. 9(4):539–543, 2018. https://doi.org/10.1007/s13239-018-00393-z.
Stewart, S. F. C., E. G. Paterson, G. W. Burgreen, P. Hariharan, M. Giarra, V. Reddy, S. W. Day, K. B. Manning, S. Deutsch, M. R. Berman, M. R. Myers, and R. A. Malinauskas. Assessment of CFD performance in simulations of an idealized medical device: results of FDA’s first computational interlaboratory study. Cardiovasc. Eng. Technol. 3(2):139–160, 2012. https://doi.org/10.1007/s13239-012-0087-5.
Sumi, T., A. Yamashita, S. Matsuda, S. Goto, K. Nishihira, E. Furukoji, H. Sugimura, H. Kawahara, T. Imamura, K. Kitamura, S. Tamura, and Y. Asada. Disturbed blood flow induces erosive injury to smooth musclecell-rich neointima and promotes thrombus formation in rabbitfemoral arteries. J. Thromb. Haemost. 8(6):1394–1402, 2010. https://doi.org/10.1111/j.1538-7836.2010.03843.x.
van Tricht, I., D. de Wachter, J. Tordoir, and P. Verdonck. Hemodynamics and complications encountered with arteriovenous fistulas and grafts as vascular access for hemodialysis: a review. Ann. Biomed. Eng. 33(9):1142–1157, 2005. https://doi.org/10.1007/s10439-005-5367-X.
Wootton, D. M., and D. N. Ku. Fluid mechanics of vascular systems, diseases, and thrombosis. Annu. Rev. Biomed. Eng. 1(1):299–329, 1999.
Acknowledgments
This work is partially funded by the School of Engineering of the University of Edinburgh, Korea Advanced Institute of Science and Technology (KAIST), Korea Institute of Science and Technology Information (KISTI), and Vascular Flow Technologies.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor David Steinman oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xue, Y., Hellmuth, R. & Shin, Dh. Formation of Vortices in Idealised Branching Vessels: A CFD Benchmark Study. Cardiovasc Eng Tech 11, 544–559 (2020). https://doi.org/10.1007/s13239-020-00477-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-020-00477-9