Abstract
Over the past years, the assisted reproductive technologies (ARTs) have been accompanied by constant innovations. For instance, intracytoplasmic sperm injection (ICSI), time-lapse monitoring of the embryonic morphokinetics, and PGS are innovative techniques that increased the success of the ART. In the same trend, the use of artificial intelligence (AI) techniques is being intensively researched whether in the embryo or spermatozoa selection. Despite several studies already published, the use of AI within assisted reproduction clinics is not yet a reality. This is largely due to the different AI techniques that are being proposed to be used in the daily routine of the clinics, which causes some uncertainty in their use. To shed light on this complex scenario, this review briefly describes some of the most frequently used AI algorithms, their functionalities, and their potential use. Several databases were analyzed in search of articles where applied artificial intelligence algorithms were used on reproductive data. Our focus was on the classification of embryonic cells and semen samples. Of a total of 124 articles analyzed, 32 were selected for this review. From the proposed algorithms, most have achieved a satisfactory precision, demonstrating the potential of a wide range of AI techniques. However, the evaluation of these studies suggests the need for more standardized research to validate the proposed models and their algorithms. Routine use of AI in assisted reproduction clinics is just a matter of time. However, the choice of AI technique to be used is supported by a better understanding of the principles subjacent to each technique, that is, its robustness, pros, and cons. We provide some current (although incipient) and potential uses of AI on the clinic routine, discussing how accurate and friendly it could be. Finally, we propose some standards for AI research on the selection of the embryo to be transferred and other future hints. For us, the imminence of its use is evident, providing a revolutionary milestone that will impact the ART.







Similar content being viewed by others
References
Ledford H. IVF at 40: revisiting the revolution in assisted reproduction. Nature. 2018. https://doi.org/10.1038/d41586-018-05792-9.
Inhorn MC, Patrizio P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. 2014;21:411–26.
Vander Borght M, Wyns C. Fertility and infertility: definition and epidemiology. Clin Biochem. 2018;62:2–10.
Begum MR. Assisted reproductive technology: techniques and limitations. J Bangladesh Coll Physicians Surg. 1970;26:135–41.
Younglai EV, Holloway AC, Foster WG. Environmental and occupational factors affecting fertility and IVF success. Hum Reprod Update. 2005;11:43–57.
Srouji SS, Mark A, Levine Z, Betensky RA, Hornstein MD, Ginsburg ES. Predicting in vitro fertilization live birth using stimulation day 6 estradiol, age, and follicle-stimulating hormone. Fertil Steril. 2005;84:795–7.
Ottosen LDM, Kesmodel U, Hindkjær J, Ingerslev HJ. Pregnancy prediction models and eSET criteria for IVF patients-do we need more information? J Assist Reprod Genet. 2007;24:29–36.
Al-Shawwa M, Abu-Naser SS. Predicting birth weight using artificial neural network. Int J Acad Heal Med Res [Internet]. 2019; 3:9–14. Available from: www.ijeais.org/ijahmr
Hota HS, Shukla SP, Kiran GK. Review of intelligent techniques applied for classification and preprocessing of medical image data. Int J Comput Sci Issues. 2013;10:267–72.
He J, Baxter SL, Xu J, Xu J, Zhou X, Zhang K. The practical implementation of artificial intelligence technologies in medicine. Nat Med. 2019. https://doi.org/10.1038/s41591-018-0307-0.
Rich E, Knight K, Nair S. Artificial intelligence. 3rd ed. McGraw-Hill. 2008.
Peixoto MS, Barros LC, Bassanezi RC, Fernandes OA. An approach via fuzzy systems for dynamics and control of the soybean aphid. Proceedings of the 2015 Conference of the International Fuzzy Systems Association and the European Society for Fuzzy Logic and Technology. Atlantic Press. Adv Intel Syst Res. 2015;89:1295–301.
McCulloch WS, Pitts W. A logical calculus of the ideas immanent in nervous activity. Bull Math Biophys. 1943;5:115–33.
Hsu F. IBM’S deep blue chess grandmaster chips. IEEE Micro. 1999;63:70–81.
Da Silva IN, Spatti DH, Flauzino RA, Liboni LHB, Dos Reis Alves SF. Artificial neural networks, vol. 39. Cham: Springer International Publishing; 2017.
Durairaj M, Thamilselvan P. Applications of artificial neural network for IVF data analysis and prediction. J Eng Comput Appl Sci. 2013;2:11–5.
Milewski R, Kuczyńska A, Stankiewicz B, Kuczyński W. How much information about embryo implantation potential is included in morphokinetic data? A prediction model based on artificial neural networks and principal component analysis. Adv Med Sci. 2017;62:202–6.
Girela JL, Gil D, Johnsson M, Gomez-Torres MJ, De Juan J. Semen parameters can be predicted from environmental factors and lifestyle using artificial intelligence methods. Biol Reprod. 2013;88:1–8.
El-Shafeiy E, El-Desouky A, El-Ghamrawy S. An optimized artificial neural network approach based on sperm whale optimization algorithm for predicting fertility quality. Stud Inform Control. 2018;27:349–58.
Sahoo AJ, Kumar Y. Seminal quality prediction using data mining methods. Technol Health Care. 2014;22:531–45.
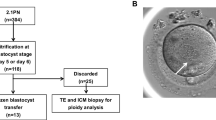
Miyagi Y, Habara T, Hirata R, Hayashi N. Feasibility of artificial intelligence for predicting live birth without aneuploidy from a blastocyst image. Reprod Med Biol. 2019;18:204–11.
Hassan MR, Al-Insaif S, Hossain MI, Kamruzzaman J. A machine learning approach for prediction of pregnancy outcome following IVF treatment. Neural Comput & Applic. 2018;32:2283–97. https://doi.org/10.1007/s00521-018-3693-9.
Manna C, Nanni L, Lumini A, Pappalardo S. Artificial intelligence techniques for embryo and oocyte classification. Reprod BioMed Online. 2013;26:42–9.
Candemir C. Estimating the semen quality from life style using fuzzy radial basis functions. Int J Mach Learn Comput. 2018;8:44–8.
Kumar V, Minz S. Feature selection: a literature review. Smart Comput Rev. 2014;4:211–29.
Ebrahimi A, Khamehchi E. Sperm whale algorithm: an effective metaheuristic algorithm for production optimization problems. J Nat Gas Sci Eng. 2016;29:211–22. https://doi.org/10.1016/j.jngse.2016.01.001.
Hornik K, Stinchcombe M, White H. Multilayer feedforward networks are universal approximators. Neural Netw. 1989;2:359–66.
Riley P. Three pitfalls to avoid in machine learning. Nature. 2019;572:27–9.
Gianaroli L, Magli MC, Gambardella L, Giusti A, Grugnetti C, Corani G. Objective way to support embryo transfer: a probabilistic decision. Hum Reprod. 2013;28:1210–20.
Hernández-González J, Inza I, Crisol-Ortíz L, Guembe MA, Iñarra MJ, Lozano JA. Fitting the data from embryo implantation prediction: learning from label proportions. Stat Methods Med Res. 2018;27:1056–66.
Morales DA, Bengoetxea E, Larrañaga P. Selection of human embryos for transfer by Bayesian classifiers. Comput Biol Med. 2008;38:1177–86.
Corani G, Magli C, Giusti A, Gianaroli L, Gambardella LM. A Bayesian network model for predicting pregnancy after in vitro fertilization. Comput Biol Med. 2013. https://doi.org/10.1016/j.compbiomed.2013.07.035.
Morales DA, Bengoetxea E, Larrañaga P, García M, Franco Y, Fresnada M, et al. Bayesian classification for the selection of in vitro human embryos using morphological and clinical data. Comput Methods Prog Biomed. 2008;90:104–16.
Uyar A, Bener A, Ciray HN. Predictive modeling of implantation outcome in an in vitro fertilization setting: an application of machine learning methods. Med Decis Mak. 2015;35:714–25.
Jakkula V. Tutorial on support vector machine (SVM). Sch EECS, Washington State Univ. 2006;1–13.
Lima CADM. Comitê de Máquinas: Uma Abordagem Unificada Empregando Máquinas de Vetores-Suporte. Repositorio da Produção Cientifica e Intelectual da Unicamp. 2004. http://www.repositorio.unicamp.br/handle/REPOSIP/261258.
Santos Filho E, Noble JA, Poli M, Griffiths T, Emerson G, Wells D. A method for semi-automatic grading of human blastocyst microscope images. Hum Reprod. 2012;27:2641–8.
Gardner D, Schoolcraft W. In-vitro culture of human blastocysts. In: Jansen R, Mortimer D, editors. Towards reproductive certainty: infertility and genetics beyond. Carnforth: Parthenon Press; 1999. p. 378–88.
Wang L-H, Fu Z-X, Ye S-Z, Ke D-G. Pattern recognition of IVF’s early embryo images based on support vector machines and texture features. Int J Eng Trends Technol. 2018;66:7–11.
Xu L, Wei X, Yin Y, Wang W, Tian Y, Zhou M. Automatic classification of human embryo microscope images based on LBP feature. Commun Comput Inf Sci. 2014;437:145–52.
Pathak B, Barooah D. Texture analysis based on the gray-level co-occurrence matrix considering possible orientations. Int J Adv Res Electr Electron Instrum Eng. 2013;2:4206–12.
Rahim A, Hossain N, Wahid T, Azam S. Face recognition using local binary patterns (LBP). Glob J Comput Sci Technol Graph Vis. 2013;13:469–81.
Galloway C, Swiatek L. Public relations and artificial intelligence: it’s not (just) about robots. Public Relat Rev. 2018;44:734–40.
Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2:230–43.
Goodfellow I, Bengio Y, Courville A. Deep learning. Cambridge: MIT Press; 2016.
Patil SN, Wali U, Swamy MK, Nagaraj SP, Patil N. Deep learning techniques for automatic classification and analysis of human in vitro fertilized (IVF) embryos. J Emerg Technol Innov Res. 2018;5:100–6.
Khan A, Gould S, Salzmann M. Segmentation of developing human embryo in time-lapse microscopy. International Symposium on Biomedical Imaging: From Nano to Macro, ISBI 2016; IEEE, TBC;930–934.
Chen T-J, Zheng W-L, Liu C-H, Huang I, Lai H-H, Liu M. Using deep learning with large dataset of microscope images to develop an automated embryo grading system. Fertil Reprod. 2019;1:51–6.
Matusevičius A, Dirvanauskas D, Maskeliūnas R, Raudonis V. Embryo cell detection using regions with convolutional neural networks. CEUR Workshop Proc. 1856;2017:89–93.
Miyagi Y, Habara T, Hirata R, Hayashi N. Feasibility of deep learning for predicting live birth from a blastocyst image in patients classified by age. Reprod Med Biol. 2019;18:190–203.
Dirvanauskas D, Maskeliunas R, Raudonis V, Damasevicius R. Embryo development stage prediction algorithm for automated time lapse incubators. Comput Methods Prog Biomed. 2019;177:161–74. https://doi.org/10.1016/j.cmpb.2019.05.027.
Cao Q, Liao SS, Meng X, Ye H, Yan Z, Wang P. Identification of viable embryos using deep learning for medical image. ACM 5th Int Conf Proceeding Ser. 2018;69–72.
Khosravi P, Kazemi E, Zhan Q, Malmsten JE, Toschi M, Zisimopoulos P, et al. Deep learning enables robust assessment and selection of human blastocysts after in vitro fertilization. NPJ Digital Med. 2019. https://doi.org/10.1038/s41746-019-0096-y.
Rad RM, Saeedi P, Au J, Havelock J. Blastomere cell counting and centroid localization in microscopic images of human embryo. 2018 IEEE 20th Int Work Multimed Signal Process MMSP 2018. IEEE; 2018;1–6.
Tran D, Cooke S, Illingworth PJ, Gardner DK. Deep learning as a predictive tool for fetal heart pregnancy following time-lapse incubation and blastocyst transfer. Hum Reprod. 2019;34:1011–8.
Bormann CL, Thirumalaraju P, Kanakasabapathy MK, Kandula H, Souter I, Dimitriadis I, et al. Consistency and objectivity of automated embryo assessments using deep neural networks. Fertil Steril. 2020;113:781–7.
VerMilyea M, Hall JMM, Diakiw SM, Johnston A, Nguyen T, Perugini D, et al. Development of an artificial intelligence-based assessment model for prediction of embryo viability using static images captured by optical light microscopy during IVF. Hum Reprod. 2020;35:770–84.
Kragh MF, Rimestad J, Berntsen J, Karstoft H. Automatic grading of human blastocysts from time-lapse imaging. Comput Biol Med. 2019;115:103494. https://doi.org/10.1016/j.compbiomed.2019.103494.
Ratna MB, Bhattacharya S, Abdulrahim B, McLernon DJ. A systematic review of the quality of clinical prediction models in in vitro fertilisation. Hum Reprod. 2020;35(1):100–16.
Acknowledgements
Grant # 2017 / 19323-5, 2018 / 24252-2 and 2018 / 19371-2 São Paulo Research Foundation (FAPESP).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Activation function
-
Mathematical function that determines the output value of the layer or the node. Used to introduce nonlinearity to the neural networks.
- Directed acyclic graph
-
Type of graph utilized in Bayesian networks aiming to detect the influence of variables has on the solution of a problem.
- Hidden layers
-
Layer(s) between the input and output layers, where the nodes process the input and output signals weighting them accordingly their importance.
- Hyperplane
-
It consists of some decision boundaries that help to classify the information into different classes or categories.
- Nodes
-
The basic information processing unit in a neural network, where inputs coming from entered variables are processed and outputs are released from the node.
- Split of dataset
-
It is the way in which the whole dataset is split into three subsets (i.e., training, validation, and test datasets).
- Test
-
The last step of the training process. After the model is trained and validated, it is subjected to the test dataset (completely different sample from the training and validation data). This process aims to measure the final accuracy of trained AI, since this step is no more supervised as the training step.
- Training
-
It is the first step to train an artificial neural network. It consists on the application of a sample (called training dataset), from which the machine will learn. The training dataset contains the features that characterize the subject to be evaluated and the targets to be predicted.
- Validation
-
The second step of the training process. Using the validation dataset, this step evaluates the model (i.e., the artificial neural network being trained) to ensure that AI training takes place correctly. With a different dataset from the training step, validation ensures that the model is not overfitted.
- Weights
-
Weights are assigned to represent the relative importance of the input coming to the node.
Rights and permissions
About this article
Cite this article
Fernandez, E.I., Ferreira, A.S., Cecílio, M.H.M. et al. Artificial intelligence in the IVF laboratory: overview through the application of different types of algorithms for the classification of reproductive data. J Assist Reprod Genet 37, 2359–2376 (2020). https://doi.org/10.1007/s10815-020-01881-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-01881-9