Abstract
Background
There are no effective therapies to prevent the occurrence and progression of vertebrobasilar dolichoectasia (VBD). In this study, we investigated the relationship between serum levels of lipoprotein-associated phospholipase A2 (Lp-PLA2) and the occurrence and progression of VBD.
Methods
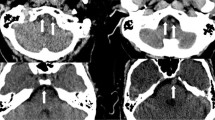
Sixty (60) cases without VBD and ischemia stroke were considered as Group A, 100 cases with VBD were further divided into Group B (VBD without ischemic stroke, n = 54) and Group C (VBD with first ever acute posterior circulation ischemic stroke, n = 46). Demographic data (such as gender and age) and past medical history (such as hypertension, diabetes, and smoking history) were collected. The levels of serum low-density lipoprotein cholesterol (LDL-C), hypersensitivity C reactive protein (hs-CRP), glycosylated hemoglobin (HbAlc), homocysteine (HCY), uric acid (UA), fibrinogen (Fib), and Lp-PLA2, etc. were measured. Logistic regression analysis was used to assess the related factors of VBD and ischemic stroke secondary to VBD.
Results
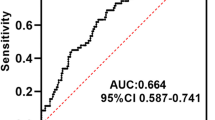
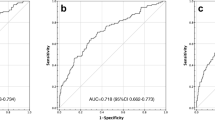
Logistic multivariate regression analysis showed that only age and the level of serum Lp-PLA2 were significantly higher in group B than those in group A (P < 0.012, P < 0.001, respectively), however, only the level of serum Lp-PLA2 was significantly higher in group C than those in group B (P < 0.001).
Conclusions
The serum marker Lp-PLA2 is an independent risk factor for the occurrence of VBD and the progression of VBD to posterior circulation ischemic stroke. Whether intervening on atherosclerosis could prevent the occurrence and development of VBD needs to be further studied.
Similar content being viewed by others
References
Ikeda K, Nakamura Y, Hirayama T, Sekine T, Nagata R, Kano O, Kawabe K, Kiyozuka T, Tamura M, Iwasaki Y (2010) Cardiovascular risk and neuroradiological profiles in asymptomatic vertebrobasilar dolichoectasia. Cerebrovasc Dis 30(1):23–28
Del BVJ, Ortiz JG, Biller J (2017) Intracranial arterial dolichoectasia. Front Neurol 8:344
Passero SG, Calchetti B, Bartalini S (2005) Intracranial bleeding in patients with vertebrobasilar dolichoectasia. Stroke. 36(7):1421–1425
Park JM, Koo JS, Kim BK, Kwon O, Lee JJ, Kang K, Lee JS, Lee J, Bae HJ (2013) Vertebrobasilar dolichoectasia as a risk factor for cerebral microbleeds. Eur J Neurol 20(5):824–830
Pico F, Labreuche J, Seilhean D, Duyckaerts C, Hauw JJ, Amarenco P (2007) Association of small-vessel disease with dilatative arteriopathy of the brain: neuropathologic evidence. Stroke. 38(4):1197–1202
Kim KJ, Kim JM, Bae YJ, Bae HJ, Jeon B, Kim JH, Han JH, Oh CW (2016) The association between vertebrobasilar dolichoectasia and hemifacial spasm. Parkinsonism Relat Disord 32:54–59
Ma X, Sun X, Yao J, Ni S, Gong J, Wang J, Li X (2013) Clinical analysis of trigeminal neuralgia caused by vertebrobasilar dolichoectasia. Neurosurg Rev 36(4):573–577 discussion 577-8
Huh G, Bae YJ, Woo HJ, Park JH, Koo JW, Song JJ. Vestibulocochlear symptoms caused by vertebrobasilar dolichoectasia. Clin Exp Otorhinolaryngol. 2019
Rodriguez CA, Mello NHO, OJH F, HAG T (2019) Painful tic convulsive as manifestation of vertebrobasilar dolichoectasia. Arq Neuropsiquiatr 77(6):445–446
Oishi Y, Ueda R, Kuranari Y, Imanishi T (2018) Vertebrobasilar dolichoectasia causing symptomatic hydrocephalus due to third ventricular compression. J Stroke Cerebrovasc Dis 27(12):3503–3504
Passero S, Filosomi G (1998) Posterior circulation infarcts in patients with vertebrobasilar dolichoectasia. Stroke. 29(3):653–659
Pico F, Labreuche J, Amarenco P (2015) Pathophysiology, presentation, prognosis, and management of intracranial arterial dolichoectasia. Lancet Neurol 14(8):833–845
Passero SG, Rossi S (2008) Natural history of vertebrobasilar dolichoectasia. Neurology. 70(1):66–72
Ubogu EE, Zaidat OO (2004) Vertebrobasilar dolichoectasia diagnosed by magnetic resonance angiography and risk of stroke and death: a cohort study. J Neurol Neurosurg Psychiatry 75(1):22–26
Yuan YJ, Xu K, Luo Q, Yu JL (2014) Research progress on vertebrobasilar dolichoectasia. Int J Med Sci 11(10):1039–1048
Thompson A, Gao P, Orfei L et al (2010) Lipoprotein-associated phospholipase A(2) and risk of coronary disease, stroke, and mortality: collaborative analysis of 32 prospective studies. Lancet. 375(9725):1536–1544
Giang DW, Perlin SJ, Monajati A, Kido DJ, Hollander J (1988) Vertebrobasilar dolichoectasia: assessment using MR. Neuroradiology. 30(6):518–523
Smoker WR, Price MJ, Keyes WD, Corbett JJ, Gentry LR (1986) High-resolution computed tomography of the basilar artery: 1. Normal size and position. AJNR Am J Neuroradiol 7(1):55–60
Oei HH, van der Meer IM, Hofman A et al (2005) Lipoprotein-associated phospholipase A2 activity is associated with risk of coronary heart disease and ischemic stroke: the Rotterdam study. Circulation. 111(5):570–575
Zhou F, Liu Y, Shi H, Huang Q, Zhou J (2018) Relation between lipoprotein-associated phospholipase A2 mass and incident ischemic stroke severity. Neurol Sci 39(9):1591–1596
Wang Y, Hu S, Ren L, Lei Z, Lan T, Cai J, Li C (2019) Lp-PLA2 as a risk factor of early neurological deterioration in acute ischemic stroke with TOAST type of large arterial atherosclerosis. Neurol Res 41(1):1–8
Alkuraishy HM, Al-Gareeb AI, Waheed HJ (2018) Lipoprotein-associated phospholipase A2 is linked with poor cardio-metabolic profile in patients with ischemic stroke: a study of effects of statins. J Neurosci Rural Pract 9(4):496–503
Kwon HM, Lee YS (2011) Dolichoectasia of the intracranial arteries. Curr Treat Options Cardiovasc Med 13(3):261–267
Wu X, Xu Y, Hong B, Zhao WY, Huang QH, Liu JM (2013) Endovascular reconstruction for treatment of vertebrobasilar dolichoectasia: long-term outcomes. AJNR Am J Neuroradiol 34(3):583–588
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This project was supported by the College Students Innovative Training Planning Project of Guangdong Province, Education Department (No. 201410560092) and this work was also supported by Sanming Project of Medicine in Shenzhen (SZSM201801014).
Rights and permissions
About this article
Cite this article
Liu, Y., Zhu, J., Deng, X. et al. Serum level of lipoprotein-associated phospholipase A2 is a potential biomarker of vertebrobasilar dolichoectasia and its progression to cerebral infarction. Neurol Sci 42, 599–605 (2021). https://doi.org/10.1007/s10072-020-04563-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04563-7