Abstract
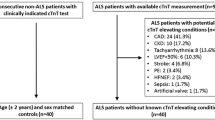
Objective
To characterize the clinical, radiological, and pathological manifestations of 18 cases showing neurogenic calf amyotrophy with creatine kinase (CK) elevation by entrapment radiculopathy (NCACKEER).
Methods
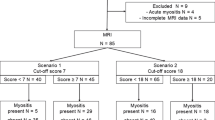
We retrospectively reviewed and evaluated the medical records of patients who complained of weakness or atrophy of the calf muscles in our department between 2004 and 2019. We identified 18 cases fulfilling the proposed criteria of NCACKEER. We extracted neurological, laboratory, neurophysiological, and neuroradiological data from all cases. Moreover, we evaluated biopsy specimens from the gastrocnemius in four cases.
Results
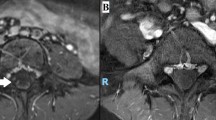
Eighteen NCACKEER cases exhibited the characteristic findings that can discriminate previously known myopathies or polyneuropathies affecting distal legs. We noticed male predominance (72%) with an average age at diagnosis of 65.6 years. Muscle weakness or atrophy was localized in the distal legs, with Achilles tendon reflexes absent in all cases. We observed elevated serum CK levels with a range from 237 to 2294 IU/L. All electromyography (EMG) studies showed neurogenic changes in the affected muscles. Lumbar spinal MRI exhibited either spinal canal stenosis at various vertebral levels or intervertebral foraminal stenosis at L4/5 and L5/S1 in all cases with significant straightening spinal and sacral alignments. All muscle biopsy specimens showed findings of neurogenic muscular degeneration with no inflammatory infiltrations. Cases with higher CK elevation had more necrotic muscle fibers.
Conclusion
We established the clinical characteristics of NCACKEER. Evaluations of serum CK level and skeletal muscle CT imaging are useful for screening, and lumbar spinal MRI, EMG and/or muscle biopsy are necessary for diagnostic confirmation.




Similar content being viewed by others
Data availability
Anonymized data can be made available by request to qualified investigators.
References
Benditz A, Boluki D, Weber M, Zeman F, Grifka J, Vollner F (2017) Comparison of lumbar lordosis in lateral radiographs in standing position with supine MR Imaging in consideration of the Sacral Slope. RoFo : Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin 189:233–239
Bernat JL, Ochoa JL (1978) Muscle hypertrophy after partial denervation: a human case. J Neurol Neurosurg Psychiatry 41:719–725
Beydoun SR, Shapiro C, Engel WK (1993) Calf muscle hypertrophy, complex repetitive discharges and spinal stenosis. Muscle Nerve 16:322–323
Cooper WH, Ringel SP, Treihaft MM, Hall KA (1985) Calf enlargement from S-1 radiculopathy. Report of two cases. J Neurosurg 62:442–444
Costa J, Graca P, Evangelista T, de Carvalho M (2005) Pain and calf hypertrophy associated with spontaneous repetitive discharges treated with botulinum toxin. Clin Neurophysiol 116:2847–2852
De BeuckeleerVanhoenacker LF, De Schepper A Jr, De SeynaeveSchepper PA (1999) Hypertrophy and pseudohypertrophy of the lower leg following chronic radiculopathy and neuropathy: imaging findings in two patients. Skeletal Radiol 28:229–232
de Visser M, Verbeeten B Jr, Lyppens KC (1986) Pseudohypertrophy of the calf following S1 radiculopathy. Neuroradiology 28:279–280
Drozdowski W, Dzieciol J (1994) Neurogenic muscle hypertrophy in radiculopathy. Acta Neurol Scand 89:464–468
Felice KJ, Whitaker CH, Grunnet ML (2003) Benign calf amyotrophy: clinicopathologic study of 8 patients. Arch Neurol 60:1415–1420
Gobbele R, Schoen SW, Schroder JM, Vorwerk D, Schwarz M (1999) S-1 radiculopathy as a possible predisposing factor in focal myositis with unilateral hypertrophy of the calf muscles. J Neurol Sci 170:64–68
Gross R, Degive C, Dernis E, Plat M, Dubourg O, Puechal X (2008) Focal myositis of the calf following S1 radiculopathy. Semin Arthritis Rheum 38:20–27
Hemmi S, Shirakawa S, Kurokawa K, Sunada Y (2013) Unilateral calf hypertrophy and focal myositis induced by S1 radiculopathy: dramatic response to steroid treatment. BMJ Case Rep 2013:bcr2013200870
Ishimoto Y, Yoshimura N, Muraki S, Yamada H, Nagata K, Hashizume H, Takiguchi N, Minamide A, Oka H, Kawaguchi H, Nakamura K, Akune T, Yoshida M (2012) Prevalence of symptomatic lumbar spinal stenosis and its association with physical performance in a population-based cohort in Japan: the Wakayama Spine Study. Osteoarthr Cartil 20:1103–1108
Khan SY, Hilton-Jones D, Rigby SP (2005) A swollen calf. Lancet 365:1662
Kottlors M, Mueller K, Kirschner J, Glocker FX (2009) Muscle hypertrophy of the lower leg caused by L5 radiculopathy. Jt Bone Spine 76:562–564
Krendel DA, Hedaya EV, Gottleib AJ (1992) Calf enlargement, S1 radiculopathy, and focal myositis. Muscle Nerve 15:517–518
Lapresle J, Fardeau M, Said G (1973) True muscular hypertrophy secondary to peripheral nerve disorder. Clinical and histological study in a case of calf hypertrophy induced by sciatica. Rev Neurol 128:153–160
Mattle HP, Hess CW, Ludin HP, Mumenthaler M (1991) Isolated muscle hypertrophy as a sign of radicular or peripheral nerve injury. J Neurol Neurosurg Psychiatry 54:325–329
Mielke U, Ricker K, Emser W, Boxler K (1982) Unilateral calf enlargement following S1 radiculopathy. Muscle Nerve 5:434–438
Montagna P, Martinelli P, Rasi F, Cirignotta F, Govoni E, Lugaresi E (1984) Muscular hypertrophy after chronic radiculopathy. Arch Neurol 41:397–398
Nakamura T, Ueno T, Arai A, Suzuki C, Nishino I, Tomiyama M (2019) Continuous hyperCKemia without calf muscle hypertrophy associated with S1 radiculopathy. Rinsho Shinkeigaku 59:592–595
Pareyson D, Morandi L, Scaioli V, Marazzi R, Boiardi A, Sghirlanzoni A (1989) Neurogenic muscle hypertrophy. Report of two cases. J Neurol 236:292–295
Ricker K, Rohkamm R, Moxley RT 3rd (1988) Hypertrophy of the calf with S-1 radiculopathy. Arch Neurol 45:660–664
Streichenberger N, Meyronet D, Fiere V, Pellissier JF, Petiot P (2004) Focal myositis associated with S-1 radiculopathy: report of two cases. Muscle Nerve 29:443–446
Swartz KR, Fee DB, Trost GR, Waclawik AJ (2002) Unilateral calf hypertrophy seen in lumbosacral stenosis: case report and review of the literature. Spine 27:E406–E409
Toribatake Y, Baba H, Kawahara N, Mizuno K, Tomita K (1997) The epiconus syndrome presenting with radicular-type neurological features. Spinal Cord 35:163–170
Volpi N, Ginanneschi F, Cerase A, Carbone SF, Agliano M, Lorenzoni P, Bellini M, Bartalini S, Di Pietro G, Rossi A (2018) Calf muscle hypertrophy following S1 radiculopathy: a stress disorder caused by hyperactivity with variable response to treatmen. Clin Neuropathol 37:146–150
Walcott BP, Nahed BV, Redjal N, Stein TD, Kahle KT, Coumans JV (2011) Pathological mechanism of lumbar disc herniation resulting in neurogenic muscle hypertrophy. J Clin Neurosci 18:1682–1684
Yang X, Kong Q, Song Y, Liu L, Zeng J, Xing R (2014) The characteristics of spinopelvic sagittal alignment in patients with lumbar disc degenerative diseases. Eur Spine J 23:569–575
Young A, Getty J, Jackson A, Kirwan E, Sullivan M, Parry CW (1983) Variations in the pattern of muscle innervation by the L5 and S1 nerve roots. Spine 8:616–624
Acknowledgements
The authors sincerely thank all patients for their participation in this study.
Funding
This study was supported in part by Grants-in-Aid for Scientific Research (C) (18K07491 to MI, 19K07813 to YI) from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Author information
Authors and Affiliations
Contributions
MS and YI contributed to the conception and design of this study. MS, HK and YF reviewed the muscle pathology. HK, KM, MI, KN, YF and YI contributed to the interpretation and critical revision of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no disclosures.
Ethical approval
The ethical committee of research on human subjects at the Gunma University Graduate School of Medicine approved the protocol of this study (HS2019-210).
Patient consent for publication
Written consent was obtained from Case 3 and the case presented in Fig. 3d.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shibata, M., Kasahara, H., Makioka, K. et al. Neurogenic calf amyotrophy with CK elevation by entrapment radiculopathy; clinical, radiological, and pathological analyses of 18 cases. J Neurol 267, 3528–3540 (2020). https://doi.org/10.1007/s00415-020-10021-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-10021-3