Abstract
Purpose
The natriuretic peptides (NPs) system, and mainly atrial natriuretic peptide (ANP), plays a key role in human metabolism and cardiometabolic disorders. Due to differences in NP levels and in prevalence of metabolic syndrome (MetS) between men and women, we aimed to explore the gender difference of association between N-terminal pro-atrial natriuretic peptide (NT-proANP) and MetS in a general population in China.
Methods
Participants’ weight, height, waist circumference, blood pressure, plasma NT-proANP, and other traditional biomarkers were measured. Multivariate logistic regression models were used to determine the association between plasma NT-proANP and MetS, and the odds ratio (OR) and 95% confidence interval (CI) were calculated for men and women, respectively.
Results
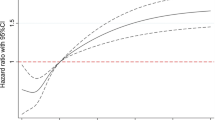
Among 2203 participants, 1361 (61.78%) were women, 687(30.77%) participants had MetS, and the average age was 53 years. Women had a higher level of NT-proANP than men. However, adjusted logistic regression demonstrated that men in the upper quartile group of NT-proANP had 0.60 (95% CI 0.39–0.92) times the risk of having MetS, while women in the upper quartile group had 1.10 (95% CI 0.77–1.56) times the risk of having MetS compared to the lower quartile group. Furthermore, with the increase of the level of NT-proANP, the ORs showed a declining trend in men (P = 0.017), but it was not statistically significant among women (P = 0.700).
Conclusions
There are gender differences in the relationship between NT-proANP and MetS, while an inverse association between plasma NT-proANP and MetS in men suggests that higher levels of NT-proANP may be a protective factor for MetS.

Similar content being viewed by others
References
Eva Kassi PP, Kaltsas G, Chrousos G (2011) Metabolic syndrome: definitions and controversies. BMC Med 9(48):2–13
Alizadeh S, Ahmadi M, Ghorbani Nejad B, Djazayeri A, Shab-Bidar S (2018) Metabolic syndrome and its components are associated with increased chronic kidney disease risk: evidence from a meta-analysis on 11 109 003 participants from 66 studies. Int J Clin Pract:e13201
Dohi T, Miyauchi K, Kasai T, Kajimoto K, Kubota N, Tamura H, Yokoyama T, Kojima T, Yokoyama K, Kurata T, Daida H (2009) Impact of metabolic syndrome on 10-year clinical outcomes among patients with acute coronary syndrome. Circ J 73:1454–1458
Brasil GA, Lima EM, Nascimento AM, Caliman IF, Medeiros AR, Silva MS et al (2015) Nandrolone decanoate induces cardiac and renal remodeling in female rats, without modification in physiological parameters: the role of ANP system. Life Sci 137:65–73
Song W, Wang H, Wu Q (2015) Atrial natriuretic peptide in cardiovascular biology and disease (NPPA). Gene 569(1):1–6
Schlueter N, de Sterke A, Willmes DM, Spranger J, Jordan J, Birkenfeld AL (2014) Metabolic actions of natriuretic peptides and therapeutic potential in the metabolic syndrome. Pharmacol Ther 144(1):12–27
Santhekadur PK, Kumar DP, Seneshaw M, Mirshahi F, Sanyal AJ (2017) The multifaceted role of natriuretic peptides in metabolic syndrome. Biomed Pharmacother 92:826–835
Gupta DK, Wang TJ (2015) Natriuretic peptides and cardiometabolic health. Circ J 79(8):1647–1655
Joyce CY, Chan OK, Wu F, Morser J, Dole WP, Wu Q (2005) Hypertension in mice lacking the proatrial natriuretic peptide convertase corin. PNAS 3:785–790
Coue M, Moro C (2016) Natriuretic peptide control of energy balance and glucose homeostasis. Biochimie 124:84–91
Zhang H, Mo X, Zhou Z, Zhu Z, HuangFu X, Xu T et al (2019) Associations among NPPA gene polymorphisms, serum ANP levels, and hypertension in the Chinese Han population. J Hum Hypertens 33(9):641–647
Speranza Rubattu SS, Ciavarella GM, Venturelli V, De Paolis P, Tocci G, De Biase L, Ferrucci A, Volpe M (2007) Reduced levels of N-terminal-proatrial natriuretic peptide in hypertensive patients with metabolic syndrome and their relationship with left ventricular mass. J Hypertens 22:833–839
Olsen MH, Hansen TW, Christensen MK, Gustafsson F, Rasmussen S, Wachtell K et al (2005) N-terminal pro brain natriuretic peptide is inversely related to metabolic cardiovascular risk factors and the metabolic syndrome. Hypertension 46(4):660–666
Wang TJ, Larson MG, Keyes MJ, Levy D, Benjamin EJ, Vasan RS (2007) Association of plasma natriuretic peptide levels with metabolic risk factors in ambulatory individuals. Circulation 115(11):1345–1353
Magnusson M, Jujic A, Hedblad B, Engstrom G, Persson M, Struck J et al (2012) Low plasma level of atrial natriuretic peptide predicts development of diabetes: the prospective Malmo diet and cancer study. J Clin Endocrinol Metab 97(2):638–645
Newton-Cheh C, Larson MG, Vasan RS, Levy D, Bloch KD, Surti A et al (2009) Association of common variants in NPPA and NPPB with circulating natriuretic peptides and blood pressure. Nat Genet 41(3):348–353
Cannone V, Boerrigter G, Cataliotti A, Costello-Boerrigter LC, Olson TM, McKie PM et al (2011) A genetic variant of the atrial natriuretic peptide gene is associated with cardiometabolic protection in the general community. J Am Coll Cardiol 58(6):629–636
Ellis KL, Newton-Cheh C, Wang TJ, Frampton CM, Doughty RN, Whalley GA et al (2011) Association of genetic variation in the natriuretic peptide system with cardiovascular outcomes. J Mol Cell Cardiol 50(4):695–701
Cannone V, Cefalu AB, Noto D, Scott CG, Bailey KR, Cavera G et al (2013) The atrial natriuretic peptide genetic variant rs5068 is associated with a favorable cardiometabolic phenotype in a Mediterranean population. Diabetes Care 36(9):2850–2856
Jujic A, Nilsson PM, Engstrom G, Hedblad B, Melander O, Magnusson M (2014) Atrial natriuretic peptide and type 2 diabetes development--biomarker and genotype association study. PLoS One 9(2):e89201
Cho DY, Koo JW (2018) Differences in metabolic syndrome prevalence by employment type and sex. Int J Environ Res Public Health 15(9):1798
Zhu Z, Zhang Q, Peng H, Zhong C, Liu Y, Huangfu X et al (2017) Plasma proANP1-98 levels are positively associated with central obesity: a cross-sectional study in a general population of China. Clin Chim Acta 469:26–30
Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, Flack JM, Carter BL, Materson BJ, Ram CVS, Cohen DL, Cadet J-C, Jean-Charles RR, Taler S, Kountz D, Townsend R, Chalmers J, Ramirez AJ, Bakris GL, Wang J, Schutte AE, Bisognano JD, Touyz RM, Sica D, Harrap SB (2014) Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens 32:3–15
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA et al (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645
Rosenzweig A, Seidman CE (1991) Atrial natriuretic factor and related peptide horiviones. Annu Rev Biochem 60:229–255
Gaggin HK, Januzzi JL Jr (2013) Biomarkers and diagnostics in heart failure. Biochim Biophys Acta 1832(12):2442–2450
Hsieh J-C, Wang J-H, Lee C-J, Chen Y-C, Liou H-H, Hsu B-G (2013) Low serum long-acting natriuretic peptide level correlates with metabolic syndrome in hypertensive patients: a cross-sectional study. Arch Med Res 44(3):215–220
Hsu BG, Shih MH, Yang YC, Ho GJ, Lee MC (2012) Fasting long-acting natriuretic peptide correlates inversely with metabolic syndrome in kidney transplant patients. Transplant Proc 44(3):646–650
Goharian TS, Goetze JP, Faber J, Andersen LB, Grontved A, Jeppesen JL (2017) Associations of proatrial natriuretic peptide with components of the metabolic syndrome in adolescents and young adults from the general population. Am J Hypertens 30(6):561–568
Wang JH, Lee CJ, Hsieh JC, Chen YC, Hsu BG (2014) Serum atrial natriuretic peptide level inversely associates with metabolic syndrome in older adults. Geriatr Gerontol Int 14(3):640–646
Fliser D, Buchholz K, Haller H (2004) Olmesartan EUTo, pravastatin in I, atherosclerosis I. Antiinflammatory effects of angiotensin II subtype 1 receptor blockade in hypertensive patients with microinflammation. Circulation 110(9):1103–1107
Rajagopalan S, Kurz S, Münzel T, Tarpey M, Freeman BA, Griendling KK, Harrison DG (1996) Angiotensin II–mediated hypertension in the rat increases vascular superoxide production via membrane NADH/NADPH oxidase activation. J Clin Invest 97(8):1916–1923
Janke J, Engeli S, Gorzelniak K, Luft FC, Sharma AM (2002) Mature adipocytes inhibit in vitro differentiation of human preadipocytes via angiotensin type 1 receptors. Diabetes 51:1699–1707
Lee KM, Lee MC, Lee CJ, Chen YC, Hsu BG (2018) Inverse association of N-terminal pro–B-type natriuretic peptide level with metabolic syndrome in kidney transplant patients. Transplant Proc 50(8):2496–2501
Wong PG, Armstrong DW, Tse MY, Brander EP, Pang SC (2013) Sex-specific differences in natriuretic peptide and nitric oxide synthase expression in ANP gene-disrupted mice. Mol Cell Biochem 374(1–2):125–135
Maria Vittoria Pitzalis MI, Massarib F, Guida P, Romito R, Forleo C, Vulpisc V, Rizzon P (2001) Infuence of gender and family history of hypertension on autonomic control of heart rate, diastolic function and brain natriuretic peptide. J Hypertens 19(1):143–8
Loke I, Squire IB, Davies JE, Ng LL (2003) Reference ranges for natriuretic peptides for diagnostic use are dependent on age, gender and heart rate. Eur J Heart Fail 5(5):599–606
Clerico A, Del Ry S, Maffei S, Prontera C, Emdin M, Giannessi D (2002) The circulating levels of cardiac natriuretic hormones in healthy adults: effects of age and sex. Clin Chem Lab Med 40:371–377
Karjalainen AH, Ruskoaho H, Vuolteenaho O, Heikkinen JE, Bäckström A-C, Savolainen MJ et al (2004) Effects of estrogen replacement therapy on natriuretic peptides and blood pressure. Maturitas 47(3):201–208
Jankowski M, Rachelska G, Donghao W, McCann SM, Gutkowsk J (2001) Estrogen receptors activate atrial natriuretic peptide in the rat heart. PNAS 98(20):11765–11770
Dockery F, Bulpitt CJ, Agarwal S, Vernon C, Nihoyannopoulos P, Kemp M et al (2008) Anti-androgens increase N-terminal pro-BNP levels in men with prostate cancer. Clin Endocrinol 68(1):59–65
Acknowledgments
We express our deep appreciation to the participants in this study and would also like to thank all members of the staff of the Center for Disease Prevention and Control of Gusu district for their support and assistance.
Availability of data and material
The data are available on request from the corresponding author at penghao@suda.edu.cn.
Funding
This study was supported by the National Natural Science Foundation of China (NO. 81903384), the Natural Science Foundation of Jiangsu Province (NO. BK20180841), and the Suzhou Science and Technology Project (NO. SS201853), and a project of the Priority Academic Program Development of Jiangsu Higher Education Institutions, China. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Qianlan Guo: Drafted the initial manuscript, made data analysis, and approved the final manuscript as submitted.
Qiu Zhang: Collected the study data, added in data analysis, critically reviewed the manuscript, and approved the final manuscript as submitted.
Yan He: Collected the study data, detected biomarkers, critically reviewed the manuscript, and approved the final manuscript as submitted.
Jijun Shi: Collected the study data, detected biomarkers, critically reviewed the manuscript, and approved the final manuscript as submitted.
Hongmei Li: Supervised the study implementation, study design, and analysis plan; revised the initial manuscript; and approved the final manuscript as submitted.
Hao Peng: Supervised the study implementation, study design, and analysis plan; revised the initial manuscript; and approved the final manuscript as submitted.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The protocols of this study were approved by the Soochow University Ethics Committee.
Informed consent
All participants signed the informed consent and participated in this study.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guo, Q., Zhang, Q., He, Y. et al. Gender difference of association between plasma N-terminal pro-atrial natriuretic peptide and metabolic syndrome. Hormones 19, 541–548 (2020). https://doi.org/10.1007/s42000-020-00222-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-020-00222-w