Parkinson Disease Associated Differences in Elective Orthopedic Surgery Outcomes: A National Readmissions Database Analysis
Abstract
Background:
Advances in the treatment of Parkinson’s disease (PD) have allowed for improvements in mortality and quality survival, making the management of comorbid conditions of aging, such as osteoarthritis, crucial.
Objective:
To determine the extent to which PD impacts hospitalization outcomes after an elective orthopedic procedure.
Methods:
This retrospective cohort study used data from the National Readmissions Database and included adults ages 40 and above with and without PD. Primary outcomes included length of stay of the index admission, discharge disposition and 30-day readmission. Logistic regression was used to compare the odds of readmission for PD patients compared to non-PD. Clinical conditions associated with readmission were compared between the two groups.
Results:
A total of 4,781 subjects with PD and 947,475 subjects without PD met inclusion criteria. Length of stay (LOS) during the index admission was longer for PD patients. PD patients were much more likely to be discharged to inpatient post-acute care (49.3% vs 26.2%) while non-PD subjects were more likely to be discharged home with (31.9% [PD] vs 44.8% [non-PD]) or without home health (18.7% [PD] vs 28.9% [non-PD]). A total of 271 PD patients (5.66%) and 28,079 non-PD patients (2.96%) were readmitted within 30 days following surgery. After adjusting for age, sex, socioeconomic status, expected payer, comorbidities, index admission LOS, year and discharge disposition, PD subjects were 31% more likely to be readmitted than non-PD subjects (AOR 1.31, 1.07–1.62).
Conclusions:
Parkinson’s disease patients were readmitted more often than non-PD patients, although the rate of readmission was still low.
INTRODUCTION
Parkinson’s disease (PD) is a common, disabling condition that affects almost 1 million in the United States alone, a number that will continue to increase as the population ages [1–3]. Advances in PD treatments have allowed for improvement in mortality and quality survival, making the management of comorbid conditions of aging crucial, as they may have a greater impact on PD survival and function than PD itself. Symptomatic osteoarthritis (OA) is common over the age of 60 [4, 5], which is when Parkinson’s disease is most likely to develop. Joint pain is responsible for up to half of reported chronic pain in PD patients and affects physical function and quality of life [6, 7].
Total hip arthroplasty (THA) and total knee arthroplasty (TKA) are effective surgical treatments to reduce joint related pain and improve physical function and quality of life in older adults with OA [8–10]. The literature on THA and TKA outcomes in PD patients is largely limited to case series of operations performed between the 1970s and 1990s [11–15]. Of the larger studies that have been done, all demonstrated that PD patients experienced relief of pain, the most common reason for surgery, but changes in functional status were less consistent [16–19]. Studies of perioperative complications associated with TKA and THA have suggested that comorbid PD is associated with increased rates of perioperative urinary tract infection, cognitive dysfunction, blood transfusion, periprosthetic infection, hip fracture, or dislocation [19–22]. Length of hospital stay for PD patients was also consistently longer [23, 24]. However, there are limited data on short term hospitalization outcomes, such as disposition and readmission as experienced by individuals with PD in the United States after elective orthopedic surgery. To address these gaps in knowledge and produce data that can guide surgeon consultations with PD patients, our study objectives were (1) to describe hospitalization outcomes (such as disposition, length of stay, cost, readmission) of individuals with and without comorbid PD undergoing an elective orthopedic procedure and (2) to determine the extent to which comorbid Parkinson disease impacts hospitalization outcomes after elective orthopedic procedure.
MATERIALS AND METHODS
Approvals and research protections
The University of Pennsylvania Human Protection Research Organization approved an exemption for the use of Health Care Utilization Project data for research analyses and publication.
Data source
Data used in this study came from the National Readmissions Database (NRD) for the years 2013 and 2014. The NRD is the only all-age, all-payer, national source of U.S. readmissions data and contains discharge data on 51.2% of the total US population and 49.3% of all US hospitalizations [25]. Unweighted, the NRD contains data on about 15 million discharges per year, and weighted, it is representative of all discharges and readmissions in the United States.
Study population
Our study sample included adults ages 40 and above who underwent elective orthopedic surgery in the inpatient setting and were included in the NRD database.
The NRD contains up to 25 ICD-9 codes per hospitalization record, and these were queried to identify Total Knee Replacement (ICD-9 “81.54”) and Total Hip Replacement (Total ICD-9 “81.51 and partial [hemiarthroplasty] 81.52”). Knee and hip replacements were chosen because they are among the most common elective orthopedic procedures performed in the United States and are procedures that may be particularly relevant to PD patients. Only primary replacements were included. We did not include revisions of knee or hip replacements, therefore outcomes for revisions were not addressed. The ICD-9 code for TKA includes total knee replacement, partial knee replacement, as well as bicompartmental, tricompartmental and unicompartmental (hemijoint) knee replacements. Individuals with comorbid Parkinson disease were identified using the ICD-9 code “332.0”. Individuals with missing, invalid or inconsistent data for our primary study variables (detailed below), were excluded.
Index admission characteristics
Data on patient, clinical, admission and hospital characteristics were extracted for the index, or orthopedic surgical, admission. Patient age, sex, insurance (Private, Medicare, Medicaid, uninsured), and socioeconomic status were examined as non-varying baseline patient characteristics. Patient race and ethnicity were not available in the dataset. The NRD contains Chronic Condition Indicator variables, which identify the presence of 29 common chronic medical conditions at the time of surgery, which were used to calculate the Elixhauser comorbidity score for each patient [26]. We also extracted data on hospital characteristics, including size, teaching status and ownership.
Study outcomes
Primary outcomes included (1) discharge disposition, (2) length of stay (in days), and (3) readmissions within 30 days of index discharge. Discharge disposition is collected by HCUP in categories that include routine (home or self care), transfer to short-term hospital, transfer to a facility (skilled nursing facility, intermediate care or other type of facility), discharge home with home health care, against medical advice and expired.
Characteristics associated with readmission
We examined whether patient characteristics, index hospitalization characteristics, or PD status were associated with readmission. We calculated the all cause 30-day readmission rate after knee replacement and hip replacement, stratified by PD status.
Statistical analysis
Statistical analyses were performed using SAS software, Version 9.4. All tests were two-tailed; a p-value less than 0.05 designated statistical significance. The Chi square text was used to compare index admission patient, clinical, admission and hospital characteristics between PD and non-PD patients who were readmitted. Multivariable logistic regression models were built with 30-day readmission as the binary outcome and PD status as the covariable of interest, adjusting for age, sex, socioeconomic status, expected payer, Elixhauser comorbidity score, index admission LOS, dataset year and discharge disposition. In order to maintain the sample design and preserve weights, we chose to perform multivariable logistic regression rather than propensity score matching, as studies have shown that multivariable adjustment generates very similar findings to propensity score matching [27]. LOS categories of 1 day, 2 days and 3 or more days were used in the models in order to capture LOS above and below the median for PD and non-PD patients. Elective knee and hip replacement surgeries were evaluated separately. A sensitivity analysis was performed to determine if there were differences in outcomes for complete vs partial hip replacements. We were unable to perform a sensitivity analysis for total and partial replacements since they are included in the same ICD-9 code.
RESULTS
Subject characteristics
A total of 4,781 persons with comorbid PD and 947,475 without PD met our study criteria. Table 1 displays socio demographic and hospital characteristics associated with elective TKA and THA. The mean age of persons with PD undergoing TKA was 70.9 years (SD 0.24), compared to 66.2 years (SD 0.05) in persons without PD (p < 0.001, t-test). THA surgeries were performed on older persons in general, and the PD + THA group was the oldest overall. The proportion of males varied by both surgery and PD diagnosis status. For TKA, males and females were nearly equally represented (51.8% male, 48.2% female) in the PD group only; a much smaller proportion of TKA surgeries in the non-PD group was male (37.5%). Sex trends were similar among persons in receipt of THA (Table 1). The overwhelming majority (>75%) of surgeries were performed in private hospitals, with large hospitals represented twice as often as those with small or medium bed sizes. Elective TKA and THA were performed most often at urban academic centers (Table 1).
Table 1
PD and non-PD patient characteristics for elective knee and hip replacement
| Elective knee replacement N = 720931 (column %) | Elective hip replacement N = 231325 (column %) | |||
| PD | No PD | PD | No PD | |
| (n = 3878) | (n = 717,056) | (n = 906) | (n = 230,419) | |
| Characteristic | ||||
| Age, mean (SD) | 70.87 (0.24) | 66.17 (0.05) | 72.68 (0.56) | 65.64 (0.09) |
| 40–49 | 21 (0.5) | 28931 (4) | * | 15486 (6.7) |
| 50–59 | 293 (7.6) | 149872 (20.9) | 86 (9.5) | 53248 (23.1) |
| 60–69 | 1364 (35.2) | 272144 (38) | 218 (24) | 77536 (33.6) |
| 70–79 | 1574 (40.6) | 205444 (28.7) | 380 (41.9) | 58859 (25.5) |
| 80+ | 623 (16.1) | 60665 (8.5) | 213 (23.5) | 25289 (11) |
| Sex | ||||
| Male | 2006 (51.8) | 268928 (37.5) | 483 (53.3) | 103641 (45) |
| Female | 1869 (48.2) | 448128 (62.5) | 423 (46.7) | 126778 (55) |
| Primary Payer | ||||
| Medicare | 3062 (79) | 406498 (56.7) | 741 (81.9) | 126041 (54.7) |
| Medicaid | 62 (1.6) | 23621 (3.3) | * | 8872 (3.9) |
| Private insurance | 700 (18.1) | 257595 (35.9) | 146 (16.1) | 87504 (38) |
| Self-Pay, No charge, Other | 50 (1.3) | 29341 (4.1) | * | 8002 (3.5) |
| Zip-code quartile | ||||
| $1 –$37,999 | 662 (17.1) | 144391 (20.1) | 178 (19.6) | 46034 (20) |
| $38,000 –$47,999 | 1074 (27.7) | 196408 (27.4) | 267 (29.5) | 61980 (26.9) |
| $48,000 –$63,999 | 1099 (28.4) | 195826 (27.3) | 204 (22.5) | 61641 (26.8) |
| $64000+ | 1040 (26.8) | 180432 (25.2) | 257 (28.3) | 60764 (26.4) |
| Length of stay (median, 95% CI) | 2.52, 2.04–2.99 | 2.30, 1.67–2.80 | 2.56, 2.06–3.22 | 2.17, 1.48–2.75 |
| 1–2 day | 879 (22.7) | 249938 (34.9) | 196 (21.7) | 97836 (42.5) |
| 3 days | 2049 (52.9) | 359297 (50.1) | 461 (51) | 99372 (43.1) |
| 4 or more days | 947 (24.4) | 107822 (15) | 248 (27.3) | 33211 (14.4) |
| Disposition after Index Admission | ||||
| Home /routine | 765 (19.7) | 208359 (29.1) | 130 (14.4) | 65641 (28.5) |
| Inpatient post-acute care | 1861 (48) | 191924 (26.8) | 497 (54.9) | 56536 (24.5) |
| Home with HHC | 1246 (32.2) | 316596 (44.2) | 278 (30.7) | 108156 (46.9) |
| Control/ownership of hospital | ||||
| Government, nonfederal | 342 (8.8) | 62807 (8.8) | 93 (10.3) | 21036 (9.1) |
| Private, not-for-profit | 3060 (79) | 554598 (77.3) | 683 (75.5) | 177650 (77.1) |
| Private, for-profit | 473 (12.2) | 99650 (13.9) | 129 (14.3) | 31733 (13.8) |
| Hospital bedsize | ||||
| Small | 892 (23) | 162913 (22.7) | 151 (16.7) | 43900 (19.1) |
| Medium | 1128 (29.1) | 204046 (28.5) | 248 (27.4) | 63358 (27.5) |
| Large | 1855 (47.9) | 350098 (48.8) | 506 (55.9) | 123161 (53.5) |
| Teaching status | ||||
| Metropolitan non-teaching | 1407 (36.3) | 270534 (37.7) | 343 (37.8) | 80305 (34.9) |
| Metropolitan teaching | 2091 (54) | 367507 (51.3) | 460 (50.8) | 125816 (54.6) |
| Non-metropolitan | 377 (9.7) | 79015 (11) | 103 (11.4) | 24298 (10.5) |
*Per HCUP data use agreement, events occurring in 10 or fewer individuals may not be publicly reported or displayed in tables.
Index hospitalization outcomes
Length of stay (LOS) was longer for PD patients who underwent TKA or THA, with a quarter having a LOS of 4 or more days compared to 15% of non-PD subjects (Table 1). In addition, PD patients who underwent TKA were much more likely to be discharged to inpatient post-acute care (48%) compared to the non-PD group (26.8%). Similarly, PD patients were discharged to inpatient post-acute care 54.9% of the time following THA compared to only 24.5% in the non-PD group. Non-PD subjects who underwent TKA were more likely to be discharged home with (32.2% [PD] vs 44.2% [non-PD]) or without home health (19.7% [PD] vs 29.1% [non-PD]). A similar relationship between PD and non-PD was seen for those undergoing THA (Table 1). Table 2 displays the distribution of specific comorbid diseases by PD status for each surgery. Persons with PD had a greater disease burden compared to persons without PD at the time of both TKA and THA, as evidenced by the average number of chronic diseases (after accounting for PD).
Table 2
Prevalence of Comorbid conditions at the time of elective orthopedic surgery in adults with and without Parkinson disease
| Elective knee replacement n with condition (%) | Elective hip replacement n with condition (%) | |||||
| PD (n = 3878) | No PD (n = 717,056) | Prevalence ratio PD/non-PD | PD (n = 906) | No PD (n = 230,419) | Prevalence ratio PD/non-PD | |
| Number of chronic | 5.34 (0.08) | 4.97 (0.03) | 5.16 (0.15) | 4.65 (0.03) | ||
| conditions excluding | ||||||
| PD mean (SD) | ||||||
| AIDS | * | 147 (0.02) | 0.00 | * | 259 (0.1) | * |
| Alcohol Abuse | 19 (0.5) | 7026 (1) | 0.50 | * | 3818 (1.7) | * |
| Deficiency anemias | 366 (9.4) | 61712 (8.6) | 1.10 | 100 (11.1) | 20343 (8.8) | 1.26 |
| Rheumatoid arthritis/collagen vascular disease | 131 (3.4) | 29599 (4.1) | 0.83 | 32 (3.5) | 8527 (3.7) | 0.95 |
| Chronic blood loss anemia | 55 (1.4) | 5844 (0.8) | 1.75 | * | 2534 (1.1) | * |
| Congestive heart failure | 122 (3.1) | 15299 (2.1) | 1.48 | 27 (3) | 4822 (2.1) | 1.43 |
| Chronic pulmonary disease | 558 (14.4) | 107613 (15) | 0.96 | 103 (11.4) | 32331 (14) | 0.81 |
| Coagulopathy | 109 (2.8) | 11022 (1.5) | 1.87 | 40 (4.4) | 3500 (1.5) | 2.93 |
| Depression | 721 (18.6) | 98377 (13.7) | 1.36 | 149 (16.4) | 27370 (11.9) | 1.38 |
| Diabetes, uncomplicated | 726 (18.7) | 137901 (19.2) | 0.97 | 129 (14.2) | 31653 (13.7) | 1.04 |
| Diabetes, complicated | 67 (1.7) | 15181 (2.1) | 0.81 | 25 (2.8) | 2926 (1.3) | 2.15 |
| Drug abuse | * | 4235 (0.6) | * | * | 1828 (0.8) | * |
| Hypertension | 2463 (63.6) | 481471 (67.1) | 0.95 | 544 (60.1) | 139029 (60.3) | 1.00 |
| Hypothyroidism | 587 (15.1) | 115269 (16.1) | 0.94 | 143 (15.8) | 31905 (13.8) | 1.14 |
| Liver disease | 26 (0.7) | 7831 (1.1) | 0.64 | 11 (1.3) | 2592 (1.1) | 1.18 |
| Lymphoma | 19 (0.5) | 1444 (0.2) | 2.50 | * | 682 (0.3) | * |
| Fluid and electrolyte disorders | 275 (7.1) | 51518 (7.2) | 0.99 | 94 (10.4) | 16703 (7.2) | 1.44 |
| Metastatic cancer | * | 373 (0.1) | * | * | 488 (0.2) | * |
| Obesity | 669 (17.3) | 181486 (25.3) | 0.68 | 85 (9.4) | 39959 (17.3) | 0.54 |
| Paralysis | * | 1482 (0.2) | * | * | 580 (0.3) | * |
| Peripheral vascular disorders | 125 (3.2) | 15960 (2.2) | 1.45 | 27 (3) | 5824 (2.5) | 1.20 |
| Psychoses | 173 (4.5) | 17616 (2.5) | 1.80 | 62 (6.9) | 4786 (2.1) | 3.29 |
| Pulmonary circulation disorders | 44 (1.1) | 6098 (0.9) | 1.22 | * | 1493 (0.6) | * |
| Renal failure | 244 (6.3) | 32814 (4.6) | 1.37 | 78 (8.6) | 9580 (4.2) | 2.05 |
| Solid tumor without metastasis | 12 (0.3) | 3047 (0.4) | 0.75 | 11 (1.2) | 1089 (0.5) | 2.40 |
| Peptic ulcer disease | * | 104 (0) | * | * | 37 (0) | * |
| Valvular disease | 145 (3.7) | 22916 (3.2) | 1.16 | 45 (5) | 7432 (3.2) | 1.56 |
| Weight loss | * | 1619 (0.2) | * | 11 (1.2) | 959 (0.4) | 3.00 |
*Per the HCUP data use agreement, events occurring in 10 or fewer individuals may not be publicly reported or displayed tables.
Readmission
A PD diagnosis was associated with a higher readmission rate. The 30- day readmission rate after TKA was 5.4% (n = 211) for persons with PD compared to 2.9% (n = 20, 856, p < 0.001) in persons without PD (Table 3). Similarly, readmissions after THA were twice as common among PD patients (6.6%, n = 60) versus non-PD patients (3.1%, n = 7,222, p < 0.001). After adjusting for age, sex, socioeconomic status, expected payer, comorbidities, index admission LOS, year and discharge disposition, PD subjects were 31% more likely to be readmitted than non-PD subjects (AOR 1.31, 1.07–1.62, unadjusted OR 1.97, 1.6–2.41) (Supplementary Table 1). As shown in Table 4, predictors of readmission differed by PD status. Among persons with PD, index hospitalization characteristics- large (versus small) hospital bed size (AOR 2.15, 1.18–3.91), and discharge to acute care or home with home health (versus routine home discharge, AOR 1.98, 1.01–3.86) were associated with statistically significant differences in odds of readmission. These structural factors also predicted readmission in non-PD patients. Additionally, patient characteristics, specifically older age, male sex, insurance, greater Elixhauser comorbidity score, and lower socioeconomic status predicted readmission among individuals without PD. Having an initial surgery in a rural hospital was associated with lower odds of readmission in the PD (AOR 0.82, 0.73–0.92) and the non-PD groups (AOR 0.81, 0.73–0.89) (Table 4).
Table 3
Number and cost of readmissions by PD status and Orthopedic procedure
| Number of all-cause 30-day readmissions | Percent readmitted within 30 days | Median cost $ per readmission | |
| PD | 281 | 5.18 | 22,218 (12,381–42,223) |
| Knee replacement | 211 | 5.43 | 21,536 (12,035–42,236) |
| Hip Replacement | 60 | 6.63 | 24,383 (13,225–43,911) |
| No PD | 30,252 | 2.96 | 23,136 (13,262–44,462) |
| Knee Replacement | 20,856 | 2.91 | 22,080 (12,843–41,504) |
| Hip Replacement | 7,222 | 3.13 | 27,546 (14,621–54,955) |
Table 4
Odds of readmission by patient clinical characteristics from index admission and PD status
| PD, Readmitted within 30 days | No PD, Readmitted within 30 days | |||
| AOR (95%) | P-value | AOR (95%) | P-value | |
| Characteristic | ||||
| Age | ||||
| 40–49 | ref | Ref | ||
| 50–59 | 0.57 (0.07–4.33) | 0.583 | 0.95 (0.85–1.07) | 0.3937 |
| 60–69 | 0.84 (0.14–5.21) | 0.852 | 0.88 (0.78–0.98) | 0.0243 |
| 70–79 | 0.76 (0.12–4.8) | 0.7744 | 1.04 (0.92–1.17) | 0.5699 |
| 80+ | 1.44 (0.22–9.28) | 0.7 | 1.59 (1.4–1.8) | <0.0001 |
| Sex | ||||
| Male | ref | ref | ||
| Female | 1.24 (0.82–1.88) | 0.2985 | 0.75 (0.71–0.78) | <0.0001 |
| Primary Payer | ||||
| Medicare | 1.76 (0.79–3.92) | 0.1675 | 1.43 (1.34–1.53) | <0.0001 |
| Medicaid | 2.68 (0.53–13.71) | 0.236 | 1.96 (1.77–2.17) | <0.0001 |
| Private insurance | Ref | Ref | ||
| Self-Pay, No-charge, Other | 0.98 (0.1–9.28) | 0.9888 | 1.34 (1.2–1.5) | <0.0001 |
| Zip-code quartile | ||||
| $1 –$37,999 | 1.44 (0.83–2.5) | 0.1896 | 1.11 (1.04–1.19) | 0.0024 |
| $38,000 –$47,999 | 0.94 (0.51–1.72) | 0.842 | 1 (0.94–1.06) | 0.9546 |
| $48,000 –$63,999 | 0.9 (0.51–1.6) | 0.7259 | 0.97 (0.92–1.03) | 0.3519 |
| $64000+ | Ref | Ref | ||
| Length of stay | ||||
| 1 day | ref | ref | ||
| 2 days | 1.01 (0.58–1.76) | 0.9828 | 1.15 (1.1–1.21) | <0.0001 |
| 3 or more days | 1.3 (0.72–2.34) | 0.3884 | 1.65 (1.55–1.76) | <0.0001 |
| Disposition Routine Home after Index Admission | ||||
| Yes | ref | ref | ||
| No | 1.98 (1.01–3.86) | 0.0468 | 1.26 (1.18–1.34) | <0.0001 |
| Number of chronic conditions | ||||
| 0–2 | ref | ref | ||
| 3 | 0.15 (0.02–1.23) | 0.0768 | 0.94 (0.85–1.03) | 0.1796 |
| 4 | 1.69 (0.61–4.67) | 0.3116 | 1.17 (1.09–1.26) | <0.0001 |
| ≥5 | 1.43 (0.63–3.27) | 0.395 | 1.68 (1.59–1.78) | <0.0001 |
| Control/ownership of hospital | ||||
| Government, nonfederal | Ref | Ref | ||
| Private, not-for-profit | 0.62 (0.32–1.19) | 0.1484 | 0.97 (0.89–1.05) | 0.4112 |
| Private, for-profit | 1.11 (0.54–2.29) | 0.7802 | 1.09 (0.98–1.2) | 0.1068 |
| Hospital bedsize | ||||
| Small | Ref | Ref | ||
| Medium | 1.63 (0.83–3.2) | 0.1592 | 1.11 (1.03–1.21) | 0.0083 |
| Large | 2.15 (1.18–3.91) | 0.0126 | 1.11 (1.04–1.2) | 0.0039 |
| Teaching status | ||||
| metropolitan non-teaching | 0.71 (0.29–1.77) | 0.4618 | 0.99 (0.93–1.04) | 0.6516 |
| metropolitan teaching | Ref | Ref | ||
| non-metropolitan | 0.71 (0.29–1.77) | 0.4618 | 0.81 (0.73–0.89) | <0.0001 |
Clinical conditions associated with readmission
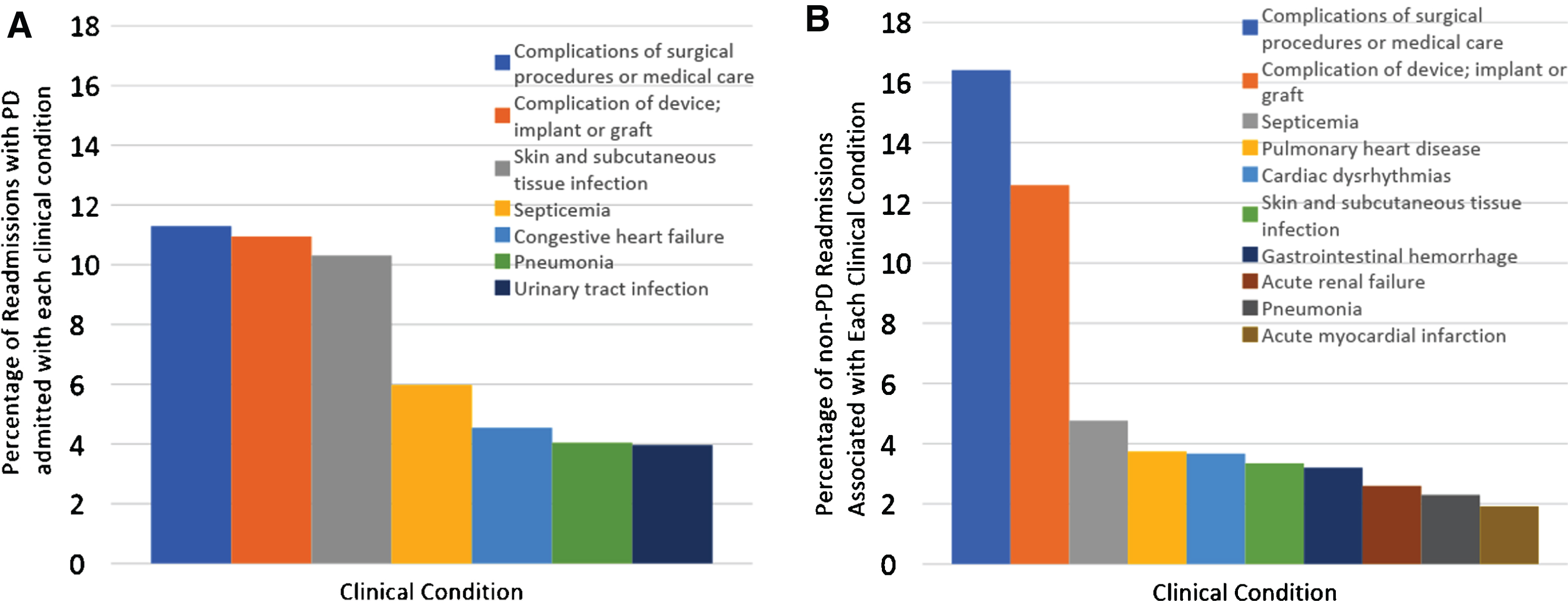
Figure 1 display the most common clinical diagnosis categories associated with 30-day readmission. “Complications of surgical procedures” and “complications of a surgical device or implant” were the most common conditions among readmitted persons (22.2% of PD patients; 29.0% of non-PD patients). PD patients were more often diagnosed with infections (skin and subcutaneous infection, sepsis, pneumonia and urinary tract infection), which accounted for almost one quarter of readmissions of PD patients but comprised only 10.4% of readmissions for non-PD patients.
Fig. 1
Clinical Conditions associated with readmission for PD and non-PD subjects. This figure displays the most common clinical diagnosis categories associated with 30 day readmission in (A) PD and (B) non-PD patients following elective orthopedic surgery. “Complications of surgical procedure” and “complications of a surgical device or implant” were the most common conditions among readmitted persons (22.2% of PD patients and 29.0% of non-PD patients). PD patients were more often diagnosed with infectious diseases (skin and subcutaneous infection, sepsis, pneumonia and urinary tract infection), which accounted for almost one quarter of readmissions for PD patients, but comprised only 10.4% of readmissions for non-PD patients.
Sensitivity analysis
A sensitivity analysis was performed to determine if there were any differences in outcomes for total vs. partial hip replacements in PD vs non-PD patients. The results are shown in Supplementary Tables 2–6. PD and non-PD patients who underwent partial hip replacement had a higher rate of 30-day readmission compared to those who underwent total hip replacement (Supplementary Table 4). There was no significant different in the odds of readmission for PD vs no PD for those who underwent partial hip replacement (Supplementary Table 5). In an unadjusted model, PD patients were 87% more likely to be readmitted within 30 days after total hip replacement compared to non-PD patients, however, after adjusting for age, sex, socioeconomic status, expected pay or, Elixhauser comorbidity score, index admission LOS and discharge disposition, the difference in odds was no longer significant (Supplementary Table 6). In a multivariable logistic regression model examining odds of readmission for PD vs no PD, there was no evidence of an interaction between procedure type (total knee replacement, partial hip replacement and total hip replacement) (unadjusted: p = 0.995, adjusted: 0.721).
DISCUSSION
As the population ages, conditions like PD and OA will become more common, and more commonly present in the same person. While there are data to support patient selection for joint replacement in the general population [28], there are currently limited data to guide clinical decision making for patients with both PD and symptomatic OA. In this study, we used a national dataset to examine short-term hospitalization outcomes associated with a comorbid diagnosis of PD following elective knee and hip arthroplasty in order to help inform patient selection and pre-operative counseling. We found that PD patients were older and had a greater comorbid disease burden at the time of surgery compared to non-PD patients. In addition, PD patients also experienced a longer length of stay and were less frequently discharged home. Finally, comorbid PD was associated with a readmission rate that was twice the average of non-PD patients, although still quite low, and the reasons for readmission among PD patients were similar for patients without PD.
PD patients had a different demographic and comorbidity profile at the time of surgery compared to non-PD patients. PD subjects were older, and a greater proportion were male. Despite OA being more common in women, it is not surprising that a slightly larger proportion of the PD group was male since PD is more common in men [4, 5, 29]. The PD group also had a higher comorbidity burden, even after adjusting for PD status. Some of this may be explained by the older age of the PD group, as many chronic diseases are associated with age [30]. In addition, several conditions are more common in Parkinson’s disease than the general population, including depression, psychosis, genitourinary disorders and diseases of the digestive system [31]. In this study, the PD group had a higher prevalence of depression and psychosis as expected, as well as CHF, deficiency anemias, coagulopathy, peripheral vascular disorders, renal failure and valvular disease. The combination of higher comorbidity burden, older age and PD may result in delays in pursuing surgery due to concerns over operating on a person with PD or focusing on stabilizing PD symptoms prior to performing elective surgery. Future studies may examine whether such delays provide benefits of reduced readmissions, result in delay of care without clinical benefit, or negatively impact patient centered and health care utilization outcomes.
In this study, PD patients had a longer hospital stay during the index admission, which is consistent with previous data from population-based studies in Finland and the US [23, 24]. Potential explanations include the development of post-operative altered mental status, medication mismanagement, poor reserve or poorer baseline functional status. Studies have shown that up to 50% of PD patients do not receive their medications on time and may not receive the correct medications, resulting in worsening mobility, and increased risk of acute delirium due to dopamine withdrawal [32]. In a study examining post-operative medication management, antidopaminergic medications were prescribed in 24/59 admissions, which can aggravate PD symptoms, contribute to altered mental status, trigger delirium and may result in a longer hospital stay [33, 34]. Post-operative delirium is more common in patients with PD compared to controls, and some degree of post-operative confusion has been reported in over 50% of PD patients following surgery [35, 36]. Hospitalized PD patients are also at greater risk of infection, including urinary tract infection and aspiration pneumonia [19], as well as other complications, including falls, urinary retention and respiratory insufficiency, all of which can contribute to longer stays [37]. The longer length of stay, therefore, may represent appropriate clinical care for individuals with comorbid PD, as well as misadventures due to improper timing and/or inconsistency of PD medications. Waiting for a return to cognitive baseline, when necessary prior to discharge, may provide assurance that post-operative cognitive dysfunction is not early evidence of an infection or post-operative delirium. It may also reflect clinical decision making which recognizes that premature discharge may be associated with increased risk of post-operative fall. In addition to longer hospital stays, PD patients were less likely to be discharged home and more likely to be discharged to a nursing facility, consistent with prior studies [38]. Longitudinal data on these patients was unavailable, so it is not clear if these were short-term stays due to increased care needs or long-term placements. Future studies may examine factors associated with long-term nursing home placement and the associated economic burden.
PD patients in this study had a higher readmission rate (5.66%) compared to non-PD patients (2.96%), however, the overall rate was quite low. The conditions prompting readmission were similar for PD and non-PD patients, including the two most common diagnoses of complications of surgical procedures and complications of the implanted device. While patients in both groups were readmitted with infection, it was more common among PD patients. A greater risk of post-operative infection (prosthetic and non-prosthetic) in PD has been previously demonstrated and was confirmed with the current data [20, 21]. Due to dysphagia and dysautonomia, PD patients are at higher risk for aspiration pneumonia and UTI, which can develop during or after a hospitalization and prompt readmission. These findings suggest that short-term hospitalization outcomes are similar for PD and non-PD patients with the exception of higher rates of infection and slightly higher rate of readmission. PD patients should be monitored closely for post-operative infection, and patients and their caregivers should be counseled on signs and symptoms of infection prior to discharge. Future studies are needed to examine functional gains experienced by PD patients to help determine if the benefits of surgical intervention outweigh the risks.
The majority of studies have demonstrated that THA and TKA are safe in patients with Parkinson’s disease and achieve excellent pain control [16–19]. Functional outcomes are less clear, but longer term are likely related at least in part to disease progression [13, 14, 39]. Our data add a national perspective to the growing evidence which suggests that PD patients experience different complications after elective orthopedic surgery, making patient selection, appropriate pre-operative counseling and post-operative monitoring paramount, and highlight the need for further study of these complications, particularly those which relate to infection.
It is important to view these data from a whole person perspective and consider the potential for surgical complications against potential risks of not performing surgery. PD patients may be more vulnerable to the negative effects of undertreated surgical orthopedic problems or delayed surgical therapy due to their underlying motor limitations. For example, a non-PD person with knee pain may walk with a cane, but the effect of a painful joint on a PD patient may mean they have to use a walker or are wheelchair bound. In addition, underuse of surgical therapy for orthopedic problems in PD may lead to higher use of centrally acting pain or spasmodic medications. These can have greater adverse effects on PD patients, including cognitive dysfunction, falls with injury, or worsened dysautonomia.
Strengths of this study include the use of a nationwide database that is not restricted by payer type. The NRD allows patients to be followed across hospitals within the state so readmissions at hospitals different from the index admission are not lost. There are also several limitations. These include limitations that accompany a retrospective design, including the potential for misclassification of an outcome or exposure variable and miscoding of variables in the dataset. In addition, we were not able to adjust for PD disease severity or pre-operative functional or cognitive status, which could have affected outcomes. The NRD does not include information on race or ethnicity, so we were unable to determine what effect race or ethnicity may have had on outcomes and whether these differed between PD and non-PD patients. This should be the subject of future studies. The data used in this study came from the years 2013-2014, and since then, there have been changes in the procedures for TKA and THA, as well as changes in anesthesia protocols, so the data may not be completely generalizable to outcomes for current surgeries. Lastly, this study focused on primary knee and hip replacements, so it did not address outcomes for revisions for either type of surgery. Despite these limitations, this study provides important information on post-operative outcomes for elective joint replacement in the PD population and can serve as a guide for pre-operative counseling and post-operative management.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
ACKNOWLEDGMENTS
This work was funded by the University of Pennsylvania Department of Neurology Translational Center of Excellence for Neuroepidemiology and Neurological Outcomes Research.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JPD-201992.
REFERENCES
[1] | Dorsey ER , Constantinescu R , Thompson JP , Biglan KM , Holloway RG , Kieburtz K , Marshall FJ , Ravina BM , Schifitto G , Siderowf A , Tanner CM ((2007) ) Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology 68: , 384–386. |
[2] | Ray Dorsey E , George BP , Leff B , Willis AW ((2013) ) The coming crisis: Obtaining care for the growing burden of neurodegenerative conditions. Neurology 80: , 1989–1996. |
[3] | Marras C , Beck JC , Bower JH , Roberts E , Ritz B , Ross GW , Abbott RD , Savica R , Van Den Eeden SK , Willis AW , Tanner C ((2018) ) Prevalence of Parkinson’s disease across North America. NPJ Parkinsons Dis 4: , 21. |
[4] | Vina ER , Kwoh CK ((2018) ) Epidemiology of osteoarthritis: Literature update. Curr Opin Rheumatol 30: , 160–167. |
[5] | Plotnikoff R , Karunamuni N , Lytvyak E , Penfold C , Schopflocher D , Imayama I , Johnson ST , Raine K ((2015) ) Osteoarthritis prevalence and modifiable factors: A population study. BMC Public Health 15: , 1195. |
[6] | Nègre-Pagès L , Regragui W , Bouhassira D , Grandjean H , Rascol O ((2008) ) Chronic pain in Parkinson’s disease: The cross-sectional French DoPaMiP survey. Mov Disord 23: , 1361–1369. |
[7] | Buhmann C , Wrobel N , Grashorn W , Fruendt O , Wesemann K , Diedrich S , Bingel U ((2017) ) Pain in Parkinson disease: A cross-sectional survey of its prevalence, specifics, and therapy. J Neurol 264: , 758–769. |
[8] | Aalund PK , Glassou EN , Hansen TB ((2017) ) The impact of age and preoperative health-related quality of life on patient-reported improvements after total hip arthroplasty. Clin Interv Aging 12: , 1951–1956. |
[9] | Bruyère O , Ethgen O , Neuprez A , Zègels B , Gillet P , Huskin JP , Reginster JY ((2012) ) Health-related quality of life after total knee or hip replacement for osteoarthritis: A 7-year prospective study. Arch Orthop Trauma Surg 132: , 1583–1587. |
[10] | Ethgen O , Bruyère O , Richy F , Dardennes C , Reginster J ((2004) ) Health-related quality of life in total hip and total knee arthroplasty. J Bone Joint Surg 86: , 963–974. |
[11] | Oni OOA , MacKenney RP ((1985) ) Total knee replacement in patients with Parkinson's disease. J Bone Joint Surg 67: , 424–425. |
[12] | Fast A , Mendelsohn E , Sosner J ((1994) ) Total knee arthroplasty in Parkinson’s disease. Arch Phys Med Rehabil 75: , 1269–1270. |
[13] | Duffy GP , Trousdale RT ((1996) ) Total knee arthoplasty in patients with Parkinson’s disease. J Arthroplasty 11: , 899–904. |
[14] | Weber M , Cabanela ME , Sim FH , Frassica FJ , Harmsen WS ((2002) ) Total hip replacement in patients with Parkinson’s disease. Int Orthop 26: , 66–68. |
[15] | Vince KG , Insall JN , Bannerman CE ((1989) ) Total knee arthroplasty in the patient with Parkinson’s disease. J Bone Joint Surg Br 71: , 51–54. |
[16] | Lazennec JY , Kim Y , Pour AE ((2018) ) Total hip arthroplasty in patients with Parkinson disease: Improved outcomes with dual mobility implants and cementless fixation. J. Arthroplasty 33: , 1455–1461. |
[17] | Tinning CG , Cochrane LA , Singer BR ((2013) ) Primary total knee arthroplasty in patients with parkinson’s disease: Analysis of outcomes. Acta Orthop Belg 79: , 301–306. |
[18] | Šponer P , Kučera T , Grinac M , Bezrouk A , Waciakowski D ((2017) ) The outcomes of total hip replacement in patients with Parkinson’s disease: Comparison of the elective and hip fracture groups. Parkinsons Dis 2017: , 1597463. |
[19] | Pepper PV , Goldstein MK ((1999) ) Postoperative complications in Parkinson’s disease. J Am Geriatr Soc 47: , 967–972. |
[20] | Mathew PG , Sponer P , Kucera T , Grinac M , Knízek J ((2013) ) Total HIP arthroplasty in patients with Parkinson’s disease. Acta Medica (Hradec Kralove) 56: , 110–116. |
[21] | Rondon AJ , Tan TL , Schlitt PK , Greenky MR , Phillips JL , Purtill JJ ((2018) ) Total joint arthroplasty in patients with Parkinson’s disease: Survivorship, outcomes, and reasons for failure. J. Arthroplasty 33: , 1028–1032. |
[22] | Huang YF , Chou YC , Yeh CC , Hu CJ , Cherng YG , Chen TL , Liao CC ((2016) ) Outcomes after non-neurological surgery in patients with Parkinson’s disease a nationwide matched cohort study. Medicine (Baltimore) 95: , e3196. |
[23] | Jämsen E , Puolakka T , Peltola M , Eskelinen A , Lehto MUK ((2014) ) Surgical outcomes of primary hip and knee replacements in patients with Parkinson’s disease: A nationwide registry-based case-controlled study. Bone Joint J 96 B: , 486–491. |
[24] | Newman JM , Sodhi N , Dalton SE , Khlopas A , Newman RP , Higuera CA , Mont MA ((2018) ) Does Parkinson disease increase the risk of perioperative complications after total hip arthroplasty? A nationwide database study. J. Arthroplasty 33: , S162–S166. |
[25] | Encyclopedia of Health Services Research, Healthcare Cost and Utilization Project (HCUP). |
[26] | Elixhauser A , Steiner C , Harris DR , Coffey RM ((1998) ) Comorbidity measures for use with administrative data. Med Care 36: , 8–27. |
[27] | Elze MC , Gregson J , Baber U , Williamson E , Sartori S , Mehran R , Nichols M , Stone GW , Pocock SJ ((2017) ) Comparison of propensity score methods and covariate adjustment: Evaluation in 4 cardiovascular studies. J Am Coll Cardiol 69: , 345–357. |
[28] | Schwartz FH , Lange J ((2017) ) Factors that affect outcome following total joint arthroplasty: A review of the recent literature. Curr Rev Musculoskelet Med 10: , 346–355. |
[29] | Hirsch L , Jette N , Frolkis A , Steeves T , Pringsheim T ((2016) ) The incidence of Parkinson’s disease: A systematic review and meta-analysis. Neuroepidemiology 46, 292-300. |
[30] | Divo MJ , Martinez CH , Mannino DM ((2014) ) Ageing and the epidemiology of multimorbidity. Eur Respir J 46: , 292–300. |
[31] | Leibson CL , Maraganore DM , Bower JH , Ransom JE , O’Brien PC , Rocca WA ((2006) ) Comorbid conditions associated with Parkinson’s disease: A population-based study. Mov Disord 21: , 446–455. |
[32] | Nageshwaran S , Hou M , Ejaz A , Toescu S , Proukakis C ((2013) ) An audit of inpatient Parkinson’s disease management at Barnet and Chase Farm Hospitals. J Neurol Neurosurg Psychiatry 84: , e2. |
[33] | Magdalinou KN , Martin A , Kessel B ((2007) ) Prescribing medications in Parkinson’s disease (PD) patients during acute admissions to a District General Hospital. Parkinsonism Relat Disord 13: , 539–540. |
[34] | Derry CP , Shah KJ , Caie L , Counsell CE ((2010) ) Medication management in people with Parkinson’s disease during surgical admissions. Postgrad Med J 86: , 334–337. |
[35] | Golden W , Lavender RC , Metzer WS ((1989) ) Acute postoperative confusion and hallucinations in Parkinson disease. Ann Intern Med 111: , 218–222. |
[36] | Klein C , Prokhorov T , Miniovitz A , Dobronevsky E , Rabey JM ((2009) ) Admission of Parkinsonian patients to a neurological ward in a community hospital. J Neural Transm 116: , 1509–1512. |
[37] | Oguh O , Videnovic A ((2012) ) Inpatient management of Parkinson disease: Current challenges and future directions. Neurohospitalist 2: , 28–35 |
[38] | Woodford H , Walker R ((2005) ) Emergency hospital admissions in idiopathic’s Parkinson’s disease. Mov Disord 20: , 1104–1108. |
[39] | Ashraf M , Priyavadhana S , Sambandam SN , Mounasamy V , Sharma OP ((2017) ) Total knee arthroplasty in patients with Parkinson’s disease- a critical analysis of available evidence. Open Orthop J 11: , 1087–1093. |



