Abstract
Purpose
Ischemic stroke is a leading cause of disability worldwide. The volume of necrotic core in affected tissue plays a major role in selecting stroke patients for thrombolytic therapy or endovascular thrombectomy. In this study, we investigated a recently reported positron emission tomography (PET) agent 2-deoxy-2-[18F]fluoro-d-glucaric acid (FGA) to determine necrotic core in a model of transient middle cerebral artery occlusion (t-MCAO) in mice.
Procedures
The radiopharmaceutical, FGA, was synthesized by controlled, rapid, and quantitative oxidation of clinical doses of 2-deoxy-2-[18F]fluoro-d-glucose (FDG) in a one-step reaction using a premade kit. Brain stroke was induced in the left cerebral hemisphere of CD-1 mice by occluding the middle cerebral artery for 1 h, and then allowing reperfusion by removing the occlusion. One day post-ictus, perfusion single-photon emission tomography (SPECT) was performed with 99mTc-lableled hexamethylpropyleneamine oxime (HMPAO), followed by PET acquisition with FGA. Plasma and brain tissue homogenates were assayed for markers of inflammation and neurotrophins.
Results
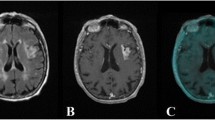
The kit-based synthesis was able to convert up to 2.2 GBq of FDG into FGA within 5 min. PET images showed 375 % more accumulation of FGA in the ipsilateral hemisphere than in the contralateral hemisphere. SPECT images showed that the ipsilateral HMPAO accumulation was reduced to 55 % of normal levels; there was a significant negative correlation between the ipsilateral accumulation of FGA and HMAPO (p < 0.05). FGA accumulation in stroke also correlated with IL-6 levels in the ipsilateral hemisphere. There was no change in IL-6 or TNFα in the plasma of stroke mice.
Conclusions
Accumulation of FGA correlated well with the perfusion defect and inflammatory injury. As a PET agent, FGA has potential to image infarcted core in the brain stroke injury with high sensitivity, resolution, and specificity.






Similar content being viewed by others
References
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P, American Heart Association Statistics Committee and Stroke Statistics Subcommittee (2017) Heart disease and stroke Statistics-2017 update: a report from the American Heart Association. Circulation 135:e146–e603
Donnan GA, Fisher M, Macleod M, Davis SM (2008) Stroke. Lancet 371:1612–1623
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, McTaggart RA, Torbey MT, Kim-Tenser M, Leslie-Mazwi T, Sarraj A, Kasner SE, Ansari SA, Yeatts SD, Hamilton S, Mlynash M, Heit JJ, Zaharchuk G, Kim S, Carrozzella J, Palesch YY, Demchuk AM, Bammer R, Lavori PW, Broderick JP, Lansberg MG (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 378:708–718
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, Yavagal DR, Ribo M, Cognard C, Hanel RA, Sila CA, Hassan AE, Millan M, Levy EI, Mitchell P, Chen M, English JD, Shah QA, Silver FL, Pereira VM, Mehta BP, Baxter BW, Abraham MG, Cardona P, Veznedaroglu E, Hellinger FR, Feng L, Kirmani JF, Lopes DK, Jankowitz BT, Frankel MR, Costalat V, Vora NA, Yoo AJ, Malik AM, Furlan AJ, Rubiera M, Aghaebrahim A, Olivot JM, Tekle WG, Shields R, Graves T, Lewis RJ, Smith WS, Liebeskind DS, Saver JL, Jovin TG (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 378:11–21
Read SJ, Hirano T, Abbott DF, Sachinidis JI, Tochon-Danguy HJ, Chan JG, Egan GF, Scott AM, Bladin CF, McKay WJ, Donnan GA (1998) Identifying hypoxic tissue after acute ischemic stroke using PET and 18F-fluoromisonidazole. Neurology 51:1617–1621
Castro P, Azevedo E, Serrador J, Rocha I, Sorond F (2017) Hemorrhagic transformation and cerebral edema in acute ischemic stroke: link to cerebral autoregulation. J Neurol Sci 372:256–261
(1997) Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. The NINDS t-PA Stroke Study Group. Stroke 28:2109–2118
Chang P, Prabhakaran S (2017) Recent advances in the management of acute ischemic stroke. F1000Research 6
Powers WJ, Rabinstein AA, Ackerson T et al (2018) 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 49:e46–e110
Wintermark M, Sanelli PC, Albers GW, Bello JA, Derdeyn CP, Hetts SW, Johnson MH, Kidwell CS, Lev MH, Liebeskind DS, Rowley HA, Schaefer PW, Sunshine JL, Zaharchuk G, Meltzer CC, American Society of Neuroradiology, American College of Radiology, Society of NeuroInterventional Surgery (2013) Imaging recommendations for acute stroke and transient ischemic attack patients: a joint statement by the American Society of Neuroradiology, the American College of Radiology and the Society of NeuroInterventional Surgery. J Am Coll Radiol 10:828–832
Houson HA, Nkepang GN, Hedrick AF, Awasthi V (2018) Imaging of isoproterenol-induced myocardial injury with (18)F labeled fluoroglucaric acid in a rat model. Nucl Med Biol 59:9–15
Taillefer R, Boucher L, Lambert R, Gregoire J, Phaneuf DC, Sikorsa H (1995) Technetium-99m antimyosin antibody (3-48) myocardial imaging: human biodistribution, safety and clinical results in detection of acute myocardial infarction. Eur J Nucl Med 22:453–464
Bokhari S, Castano A, Pozniakoff T, Deslisle S, Latif F, Maurer MS (2013) (99m)Tc-pyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidoses. Circ Cardiovasc Imaging 6:195–201
Khaw BA, Silva JD, Petrov A, Hartner W (2002) Indium 111 antimyosin and Tc-99m glucaric acid for noninvasive identification of oncotic and apoptotic myocardial necrosis. J Nucl Cardiol 9:471–481
Mdzinarishvili A, Geldenhuys WJ, Abbruscato TJ, Bickel U, Klein J, Van der Schyf CJ (2005) NGP1-01, a lipophilic polycyclic cage amine, is neuroprotective in focal ischemia. Neurosci Lett 383:49–53
Sydserff SG, Green AR, Cross AJ (1996) The effect of oedema and tissue swelling on the measurement of neuroprotection; a study using chlormethiazole and permanent middle cerebral artery occlusion in rats. Neurodegeneration 5:81–85
Harada S, Yamazaki Y, Tokuyama S (2013) Orexin-A suppresses postischemic glucose intolerance and neuronal damage through hypothalamic brain-derived neurotrophic factor. J Pharmacol Exp Ther 344:276–285
Shu X, Zhang Y, Xu H, Kang K, Cai D (2013) Brain-derived neurotrophic factor inhibits glucose intolerance after cerebral ischemia. Neural Regen Res 8:2370–2378
Tan JC, Dillon WP, Liu S, Adler F, Smith WS, Wintermark M (2007) Systematic comparison of perfusion-CT and CT-angiography in acute stroke patients. Ann Neurol 61:533–543
Oei MTH, Meijer FJA, van der Woude WJ, Smit EJ, van Ginneken B, Prokop M, Manniesing R (2017) Interleaving cerebral CT perfusion with neck CT angiography. Part I. Proof of concept and accuracy of cerebral perfusion values. Eur Radiol 27:2649–2656
Waaijer A, van Leeuwen MS, van Osch MJ et al (2007) Changes in cerebral perfusion after revascularization of symptomatic carotid artery stenosis: CT measurement. Radiology 245:541–548
Bollwein C, Plate A, Sommer WH, Thierfelder KM, Janssen H, Reiser MF, Straube A, von Baumgarten L (2016) Diagnostic accuracy of whole-brain CT perfusion in the detection of acute infratentorial infarctions. Neuroradiology 58:1077–1085
Lee DH, Kang DW, Ahn JS, Choi CG, Kim SJ, Suh DC (2005) Imaging of the ischemic penumbra in acute stroke. Korean J Radiol 6:64–74
Heiss WD, Sobesky J, Hesselmann V (2004) Identifying thresholds for penumbra and irreversible tissue damage. Stroke 35:2671–2674
Guadagno JV, Warburton EA, Aigbirhio FI, Smielewski P, Fryer TD, Harding S, Price CJ, Gillard JH, Carpenter TA, Baron JC (2004) Does the acute diffusion-weighted imaging lesion represent penumbra as well as core? A combined quantitative PET/MRI voxel-based study. J Cereb Blood Flow Metab 24:1249–1254
Heiss WD, Zaro Weber O (2017) Validation of MRI determination of the penumbra by PET measurements in ischemic stroke. J Nucl Med 58:187–193
Lee GH, Kim JS, Oh SJ, Kang DW, Kwon SU (2015) (18)F-fluoromisonidazole (FMISO) positron emission tomography (PET) predicts early infarct growth in patients with acute ischemic stroke. J Neuroimaging 25:652–655
Heiss WD (2014) Radionuclide imaging in ischemic stroke. J Nucl Med 55:1831–1841
Lee M, Zaharchuk G, Guzman R, Achrol A, Bell-Stephens T, Steinberg GK (2009) Quantitative hemodynamic studies in moyamoya disease: a review. Neurosurg Focus 26:E5
Read SJ, Hirano T, Abbott DF, Markus R, Sachinidis JI, Tochon-Danguy HJ, Chan JG, Egan GF, Scott AM, Bladin CF, McKay WJ, Donnan GA (2000) The fate of hypoxic tissue on 18F-fluoromisonidazole positron emission tomography after ischemic stroke. Ann Neurol 48:228–235
Markus R, Reutens DC, Kazui S et al (2004) Hypoxic tissue in ischaemic stroke: persistence and clinical consequences of spontaneous survival. Brain 127:1427–1436
Narula J, Petrov A, Pak KY, Khaw B-A (1995) 962-122 very early noninvasive imaging of acute myocardial infarcts with Tc-99m-glucarate. J Am Coll Cardiol 25:218A–218A
Morgan CD, Stephens M, Zuckerman SL, Waitara MS, Morone PJ, Dewan MC, Mocco J (2015) Physiologic imaging in acute stroke: patient selection. Interv Neuroradiol 21:499–510
Yaoita H, Uehara T, Brownell AL et al (1991) Localization of technetium-99m-glucarate in zones of acute cerebral injury. J Nucl Med 32:272–278
Khaw B-A, Nakazawa A, O'Donnell S, Pak K-Y, Narula J (1997) Avidity of technetium 99m glucarate for the necrotic myocardium: in vivo and in vitro assessment. J Nucl Cardiol 4:283–290
Gerson MC, McGoron AJ (1997) Technetium 99m glucarate: what will be its clinical role? J Nucl Cardiol 4:336–340
Choudhury PS, Savio E, Solanki KK et al (2012) (99m)Tc glucarate as a potential radiopharmaceutical agent for assessment of tumor viability: from bench to the bed side. World J Nucl Med 11:47–56
Waje-Andreassen U, Krakenes J, Ulvestad E, Thomassen L, Myhr KM, Aarseth J, Vedeler CA (2005) IL-6: an early marker for outcome in acute ischemic stroke. Acta Neurol Scand 111:360–365
Gandolfi M, Smania N, Vella A, Picelli A, Chirumbolo S (2017) Assessed and emerging biomarkers in stroke and training-mediated stroke recovery: state of the art. Neural Plast 2017:1389475
Li P, Mao L, Zhou G, Leak RK, Sun BL, Chen J, Hu X (2013) Adoptive regulatory T-cell therapy preserves systemic immune homeostasis after cerebral ischemia. Stroke 44:3509–3515
Sieber MW, Claus RA, Witte OW, Frahm C (2011) Attenuated inflammatory response in aged mice brains following stroke. PLoS One 6:e26288
Lui YW, Tang ER, Allmendinger AM, Spektor V (2010) Evaluation of CT perfusion in the setting of cerebral ischemia: patterns and pitfalls. AJNR Am J Neuroradiol 31:1552–1563
Knoepfli AS, Sekoranja L, Bonvin C, Delavelle J, Kulcsar Z, Rüfenacht D, Yilmaz H, Sztajzel R, Altrichter S, Lövblad KO (2009) Evaluation of perfusion CT and TIBI grade in acute stroke for predicting thrombolysis benefit and clinical outcome. J Neuroradiol 36:131–137
Alexandrov AV, Black SE, Ehrlich LE, Bladin CF, Smurawska LT, Pirisi A, Caldwell CB (1996) Simple visual analysis of brain perfusion on HMPAO SPECT predicts early outcome in acute stroke. Stroke 27:1537–1542
Umemura A, Suzuka T, Yamada K (2000) Quantitative measurement of cerebral blood flow by (99m)Tc-HMPAO SPECT in acute ischaemic stroke: usefulness in determining therapeutic options. J Neurol Neurosurg Psychiatry 69:472–478
Eicker SO, Turowski B, Heiroth HJ, Steiger HJ, Hanggi D (2011) A comparative study of perfusion CT and 99m Tc-HMPAO SPECT measurement to assess cerebrovascular reserve capacity in patients with internal carotid artery occlusion. Eur J Med Res 16:484–490
Lewis DH, Toney LK, Baron JC (2012) Nuclear medicine in cerebrovascular disease. Semin Nucl Med 42:387–405
Szigeti K, Horvath I, Veres DS et al (2015) A novel SPECT-based approach reveals early mechanisms of central and peripheral inflammation after cerebral ischemia. J Cereb Blood Flow Metab 35:1921–1929
Martin A, Mace E, Boisgard R et al (2012) Imaging of perfusion, angiogenesis, and tissue elasticity after stroke. J Cereb Blood Flow Metab 32:1496–1507
Ceulemans AG, Hernot S, Zgavc T, Caveliers V, Hachimi-Idrissi S, Sarre S, Lahoutte T, Michotte Y (2011) Serial semiquantitative imaging of brain damage using micro-SPECT and micro-CT after endothelin-1-induced transient focal cerebral ischemia in rats. J Nucl Med 52:1987–1992
Acknowledgments
Technical assistance from Ms. Andria Hedrick is acknowledged.
Funding
This study was partly funded by 1R41HL140919-01A1 STTR grant to Hexakit, Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
VA is partly employed by Hexakit, Inc. and is its owner.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Houson, H., Mdzinarishvili, A., Gali, H. et al. PET Detection of Cerebral Necrosis Using an Infarct-Avid Agent 2-Deoxy-2-[18F]Fluoro-d-Glucaric Acid (FGA) in a Mouse Model of the Brain Stroke. Mol Imaging Biol 22, 1353–1361 (2020). https://doi.org/10.1007/s11307-020-01513-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-020-01513-9