Abstract
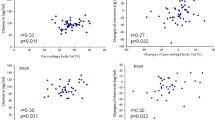
Infants born small for gestational age (SGA) are known to have increased risk of developing several pathologies, including the metabolic syndrome, when they grow up. It has been described that both the growth pattern of these children as well as the risk of their presenting future metabolic disorders can be influenced by the expression of adipokines. Among them, chemerin has demonstrated to be implicated in lipid and glucose metabolism, presenting higher circulating concentration in diabetic and obese subjects. Thus, the aim of this study was to analyze the association of anthropometric parameters and plasmatic biochemical parameters with circulating chemerin concentration in SGA children. This prospective, longitudinal study was carried out in plasma samples of Caucasian children born SGA at Hospital Universitario de Álava-Txagorritxu. Significant positive correlations were observed between chemerin concentrations at 3 months and insulin values at 3 months and also with triglyceride levels at 24 months. These associations were maintained after adjustment by anthropometric parameters. Therefore, we suggest that circulating chemerin concentration, measured at an early age, might be an indicator of future metabolic alterations in SGA children.

Similar content being viewed by others
References
Britt C, Sven C, Ove A (2005) Preterm and term births of small for gestational age infants: a population-based study of risk factors among nulliparous women. BJOG Int J Obstet Gynaecol 105(9):1011–1017
Lee PA, Chernausek SD, Hokken-Koelega A, Czernichow P (2003) International small for gestational age advisory board consensus development conference statement: management of short children born small for gestational age, April 24-October 1, 2001. Pediatrics 111:1253–1261
Saenger P, Czernichow P, Hughes I, Reiter EO (2007) Small for gestational age: short stature and beyond. Endocr Rev 28(2):219–251
Hokken-Koelega AC, De Ridder MA, Lemmen RJ, Den Hartog H, De Muinck Keizer-Schrama SM, Drop SL (1995) Children born small for gestational age: do they catch up? Pediatr Res 38:267–271
Saggese G, Fanos M, Simi F (2013) SGA children: auxological and metabolic outcomes - the role of GH treatment. J Matern Fetal Neonatal Med 26(2):64–67
Ahima RS, Flier JS (2000) Adipose tissue as an endocrine organ. Trends Endocrin Met 11(8):327–332
Fatima SS, Rehman R, Baig M, Khan TA (2014) New roles of the multidimensional adipokine: chemerin. Peptides 62:15–20
Rourke JL, Dranse HJ, Sinal CJ (2013) Towards an integrative approach to understanding the role of chemerin in human health and disease. Obes Rev 14(3):245–262
Barnea G, Strapps W, Herrada G, Berman Y, Ong J, Kloss B, Axel R, Lee KJ (2008) The genetic design of signaling cascades to record receptor activation. Proc Natl Acad Sci U S A 105:64–69
Samson M, Edinger AL, Stordeur P, Rucker J, Verhasselt V, Sharron M, Govaerts C, Mollereau C, Vassart G, Doms RW, Parmentier M (1998) ChemR23, a putative chemoattractant receptor, is expressed in monocyte-derived dendritic cells and macrophages and is a coreceptor for SIV and some primary HIV-1 strains. Eur J Immunol 28(5):1689–1700
Wittamer V, Franssen JD, Vulcano M, Mirjolet JF, Le Poul E, Migeotte I, Brezillon S, Tyldesley R, Blanpain C, Detheux M, Mantovani A, Sozzani S, Vassart G, Parmentier M, Communi D (2003) Specific recruitment of antigen-presenting cells by chemerin, a novel processed ligand from human inflammatory fluids. J Exp Med 198(7):977–985
Zabel BA, Nakae S, Zuniga L, Kim JY, Ohyama T, Alt C, Pan J, Suto H, Soler D, Allen SJ, Handel TM, Song CH, Galli SJ, Butcher EC (2008) Mast cell-expressed orphan receptor CCRL2 binds chemerin and is required for optimal induction of IgE-mediated passive cutaneous anaphylaxis. J Exp Med 205(10):2207–2220
Mattern A, Zellmann T, Beck-Sickinger AG (2014) Processing, signaling, and physiological function of chemerin. IUBMB Life 66(1):19–26
Ernst MC, Haidl ID, Zuniga LA, Dranse HJ, Rourke JL, Zabel BA, Butcher EC, Sinal CJ (2012) Disruption of the chemokine-like receptor-1 (CMKLR1) gene is associated with reduced adiposity and glucose intolerance. Endocrinology 153(2):672–682
Goralski KB, McCarthy TC, Hanniman EA, Zabel BA, Butcher EC, Parlee SD, Muruganandan S, Sinal CJ (2007) Chemerin, a novel adipokine that regulates adipogenesis and adipocyte metabolism. J Biol Chem 282(38):28175–28188
Bozaoglu K, Bolton K, McMillan J, Zimmet P, Jowett J, Collier G, Walder K, Segal D (2007) Chemerin is a novel adipokine associated with obesity and metabolic syndrome. Endocrinology 148(10):4687–4694
Bozaoglu K, Segal D, Shields KA, Cummings N, Curran JE, Comuzzie AG, Mahaney MC, Rainwater DL, VandeBerg JL, MacCluer JW, Collier G, Blangero J, Walder K, Jowett JBM (2009) Chemerin is associated with metabolic syndrome phenotypes in a Mexican-American population. J Clin Endocrinol Metab 94(8):3085–3098
Shin HY, Lee DC, Chu SH, Jeon JY, Lee MK, Im JA, Lee JW (2012) Chemerin levels are positively correlated with abdominal visceral fat accumulation. Clin Endocrinol 77(1):47–50
Tonjes A, Fasshauer M, Kratzsch J, Stumvoll M, Bluher M (2010) Adipokine pattern in subjects with impaired fasting glucose and impaired glucose tolerance in comparison to normal glucose tolerance and diabetes. PLoS One 5(11):e13911
Yang M, Yang G, Dong J, Liu Y, Zong H, Liu H, Boden G, Li L (2010) Elevated plasma levels of chemerin in newly diagnosed type 2 diabetes mellitus with hypertension. J Investig Med 58(7):883–886
Chakaroun R, Raschpichler M, Kloting N, Oberbach A, Flehmig G, Kern M, Schon MR, Shang E, Lohmann T, Dressler M, Fasshauer M, Stumvoll M, Bluher M (2012) Effects of weight loss and exercise on chemerin serum concentrations and adipose tissue expression in human obesity. Metabolism 61(5):706–714
Ress C, Tschoner A, Engl J, Klaus A, Tilg H, Ebenbichler CF, Patsch JR, Kaser S (2010) Effect of bariatric surgery on circulating chemerin levels. Eur J Clin Investig 40(3):277–280
Carrascosa A, Fernández JM, Ferrández A, López-Siguero JP, López D, Sánchez E (2010) Estudios españoles de crecimiento. Available from: http://www.aeped.es/noticias/estudios-espanolescrecimiento-2010. Last Accessed May 2020
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419
Léniz A, Portillo MP, Fernandez-Quintela A, Macarulla MT, Sarasua-Miranda A, Del Hoyo M, Diez-Lopez I (2019) Has the adipokine profile an influence on the catch-up growth type in small for gestational age infants? J Physiol Biochem 75:311–319
Barker DJ, Gluckman PD, Godfrey KM, Harding JE, Owens JA, Robinson JS (1993) Fetal nutrition and cardiovascular disease in adult life. Lancet 341(8850):938–941
Kajantie E, Barker DJ, Osmond C, Forsen T, Eriksson JG (2008) Growth before 2 years of age and serum lipids 60 years later: the Helsinki birth cohort study. Int J Epidemiol 37(2):280–289
Varvarigou AA (2010) Intrauterine growth restriction as a potential risk factor for disease onset in adulthood. J Pediatr Endocrinol Metab 3:215–224
Owen CG, Whincup PH, Odoki K, Gilg JA, Cook DG (2003) Birth weight and blood cholesterol level: a study in adolescents and systematic review. Pediatrics 111(5 Pt 1):1081–1089
de Jong M, Cranendonk A, van Weissenbruch MM (2015) Components of the metabolic syndrome in early childhood in very-low-birth-weight infants and term small and appropriate for gestational age infants. Pediatr Res 78(4):457–461
Castanys-Munoz E, Kennedy K, Castaneda-Gutierrez E, Forsyth S, Godfrey KM, Koletzko B, Ozanne SE, Rueda R, Schoemaker M, van der Beek EM, van Buuren S, Ong KK (2017) Systematic review indicates postnatal growth in term infants born small-for-gestational-age being associated with later neurocognitive and metabolic outcomes. Acta Paediatr 106(8):1230–1238
Dominguez Hernandez C, Klunder Klunder M, Huang F, Flores Armas EM, Velazquez-Lopez L, Medina-Bravo P (2016) Association between abdominal fat distribution, adipocytokines and metabolic alterations in obese low-birth-weight children. Pediatr Obes 11(4):285–291
De Henauw S, Michels N, Vyncke K, Hebestreit A, Russo P, Intemann T, Peplies J, Fraterman A, Eiben G, de Lorgeril M, Tornaritis M, Molnar D, Veidebaum T, Ahrens W, Moreno LA, IDEFICS consortium (2014) Blood lipids among young children in Europe: results from the European IDEFICS study. Int J Obes 38(2):S67–S75
Prieto Albino L, Mateos Montero C, Galan Rebollo A, Arroyo Diez J, Vadillo Machota JM (1999) The lipid profile in the children and adolescents of caceres province. Aten Primaria 23(7):404–410
Bobbert T, Schwarz F, Fischer-Rosinsky A, Maurer L, Mohlig M, Pfeiffer AF, Mai K, Spranger J (2016) Chemerin and prediction of diabetes mellitus type 2. Clin Endocrinol 82(6):838–843
Sledzinska M, Szlagatys-Sidorkiewicz A, Brzezinski M, Kazmierska K, Sledzinski T, Kaminska B (2017) Serum chemerin in children with excess body weight may be associated with ongoing metabolic complications - a pilot study. Adv Med Sci 62(2):383–386
Cheon DY, Kang JG, Lee SJ, Ihm SH, Lee EJ, Choi MG, Yoo HJ, Kim CS (2017) Serum chemerin levels are associated with visceral adiposity, independent of waist circumference, in newly diagnosed type 2 diabetic subjects. Yonsei Med J 58(2):319–325
Boyuk B, Guzel EC, Atalay H, Guzel S, Mutlu LC, Kucukyalcin V (2015) Relationship between plasma chemerin levels and disease severity in COPD patients. Clin Respir J 9(4):468–474
Mohamed AA, Sabry S, Abdallah AM, Elazeem NAA, Refaey D, Algebaly HAF, Fath GAE, Omar H (2017) Circulating adipokines in children with nonalcoholic fatty liver disease: possible noninvasive diagnostic markers. Ann Gastroenterol 30(4):457–463
Zhang G, Xiao M, Zhang L, Zhao Y, Yang Q (2017) Association of serum chemerin concentrations with the presence of atrial fibrillation. Ann Clin Biochem 54(3):342–347
Ba HJ, Xu LL, Qin YZ, Chen HS (2019) Serum chemerin levels correlate with determinants of metabolic syndrome in obese children and adolescents. Clin Med Insights Pediatr 13:1179556519853780
Maghsoudi Z, Kelishadi R, Hosseinzadeh-Attar MJ (2016) The comparison of chemerin, adiponectin and lipid profile indices in obese and non-obese adolescents. Diabetes Metab Syndr 10(1):S43–S46
Takahashi M, Takahashi Y, Takahashi K, Zolotaryov FN, Hong KS, Kitazawa R, Iida K, Okimura Y, Kaji H, Kitazawa S, Kasuga M, Chihara K (2008) Chemerin enhances insulin signaling and potentiates insulin-stimulated glucose uptake in 3T3-L1 adipocytes. FEBS Lett 582(5):573–578
Takahashi M, Okimura Y, Iguchi G, Nishizawa H, Yamamoto M, Suda K, Kitazawa R, Fujimoto W, Takahashi K, Zolotaryov FN, Hong KS, Kiyonari H, Abe T, Kaji H, Kitazawa S, Kasuga M, Chihara K, Takahashi Y (2011) Chemerin regulates beta-cell function in mice. Sci Rep 1:123
Shimamura K, Matsuda M, Miyamoto Y, Yoshimoto R, Seo T, Tokita S (2009) Identification of a stable chemerin analog with potent activity toward ChemR23. Peptides 30(8):1529–1538
Haberl EM, Pohl R, Rein-Fischboeck L, Feder S, Eisinger K, Krautbauer S, Sinal CJ, Buechler C (2018) Ex vivo analysis of serum chemerin activity in murine models of obesity. Cytokine 104:42–45
Toulany J, Parlee SD, Sinal CJ, Slayter K, McNeil S, Goralski KB (2016) CMKLR1 activation ex vivo does not increase proportionally to serum total chemerin in obese humans. Endocrine Connect 5(6):70–81
Chang SS, Eisenberg D, Zhao L, Adams C, Leib R, Morser J, Leung L (2016) Chemerin activation in human obesity. Obesity (Silver Spring) 24(7):1522–1529
Buechler C, Feder S, Haberl EM, Aslanidis C (2019) Chemerin isoforms and activity in obesity. Int J Mol Sci 20(5):1128
Funding
This work was supported by grants from Pfizer International (2012/13), Government of the Basque Country (IT-572-13) and Instituto de Salud Carlos III (CIBERobn).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol has been approved by the Ethical Committee of the Hospital Universitario de Álava-Txagorritxu (HUA) (Ref. 2012-050).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• Serum chemerin and triglycerides are correlated at 3 and 24 months of life.
• Chemerin could be proposed as a biomarker of prognosis for serum triglycerides.
• Serum chemerin also correlates with plasma insulin and glucose values at 3 months.
Rights and permissions
About this article
Cite this article
Léniz, A., Fernández-Quintela, A., del Hoyo, M. et al. Chemerin concentrations in infants born small for gestational age: correlations with triglycerides and parameters related to glucose homeostasis. J Physiol Biochem 77, 133–140 (2021). https://doi.org/10.1007/s13105-020-00750-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13105-020-00750-4