Introduction
For adults globally, mental, neurologic, and substance-use (MNS) disorders are the greatest contributor to years lived with disability (YLDs) – accounting for almost one-third of all YLDs [Institute for Health Metrics and Evaluation (IHME), 2017]. This finding is true in both high-income and low- and middle-income countries (LMICs). Depression alone accounts for 35% of all YLDs for mental disorders in countries with a low socio-demographic index, and over 6% of YLDs from any health condition (IHME, 2017). Yet, even with this widespread recognition of MNS disorders – and depression in particular – as key drivers of global disability, the gap between knowledge of evidence-based prevention and treatment approaches in the literature and its application in community settings is large. In high-income settings, only one in five patients with depression receive minimally-adequate treatment, with gaps increasing to one in nine in upper-middle-income countries and 1 in 27 for lower-middle-income countries (Thornicroft et al., Reference Thornicroft, Chatterji, Evans-Lacko, Gruber, Sampson, Aguilar-Gaxiola, Al-Hamzawi, Alonso, Andrade, Borges, Bruffaerts, Bunting, De Almeida, Florescu, De Girolamo, Gureje, Haro, He, Hinkov, Karam, Kawakami, Lee, Navarro-Mateu, Piazza, Posada-Villa, De Galvis and Kessler2017). Others have written that a comprehensive ‘mental health care gap’ would likely be much larger, as it would include the biomedical treatment gap, combined with the psychosocial care gap as well as the physical health care gap (Pathare et al., Reference Pathare, Brazinova and Levav2018). The recent landmark Lancet Commission on Global Mental Health and Sustainable Development (Patel et al., Reference Patel, Saxena, Lund, Thornicroft, Baingana, Bolton, Chisholm, Collins, Cooper, Eaton, Herrman, Herzallah, Huang, Jordans, Kleinman, Medina-Mora, Morgan, Niaz, Omigbodun, Prince, Rahman, Saraceno, Sarkar, De Silva, Singh, Stein, Sunkel and UnÜtzer2018) highlighted that even amongst high-income countries that have increased access to, and use of, evidence-based treatments for mood disorders from 1990 to 2015, the population-level prevalence of these conditions has not decreased. In fact, from 1991 to 2016, the disability burden of MNS disorders has steadily increased across both low- and high-income countries, although the largest increases (almost a doubling) have been seen in low-income countries (Patel et al., Reference Patel, Saxena, Lund, Thornicroft, Baingana, Bolton, Chisholm, Collins, Cooper, Eaton, Herrman, Herzallah, Huang, Jordans, Kleinman, Medina-Mora, Morgan, Niaz, Omigbodun, Prince, Rahman, Saraceno, Sarkar, De Silva, Singh, Stein, Sunkel and UnÜtzer2018).
To address the particularly large depression care gap in LMICs, the past decade has seen increased investment in pragmatic effectiveness trials to generate the evidence-base for mental health treatment in LMICs. The Disease Control Priorities, 3rd Edition, states that sufficient evidence exists for effectiveness and cost-effectiveness for preventative, drug, physical interventions, and psychosocial interventions for individuals with depressive disorders globally (Patel et al., Reference Patel, Chisholm, Parikh, Charlson, Degenhardt, Dua, Ferrari, Hyman, Laxminarayan, Levin, Lund, Medina Mora, Petersen, Scott, Shidhaye, Vijayakumar, Thornicroft and Whiteford2016). Due to very limited trained mental health human resources in LMICs (Saxena et al., Reference Saxena, Thornicroft, Knapp and Whiteford2007; Kakuma et al., Reference Kakuma, Minas, van Ginneken, Dal Poz, Desiraju, Morris, Saxena and Scheffler2011), many interventions tested to date in LMICs have employed task-shifting, using lay health workers or peers to deliver low-intensity behavioral interventions, often in collaboration with primary care staff who can deliver psychopharmacological or other higher-intensity interventions as needed. In the past few years, this evidence base for depression treatment has matured, with numerous pragmatic effectiveness trials across LMICs showing effectiveness for trans-diagnostic delivered psychological therapies (Bolton et al., Reference Bolton, Lee, Haroz, Murray, Dorsey, Robinson, Ugueto and Bass2014; Murray et al., Reference Murray, Dorsey, Haroz, Lee, Alsiary, Haydary, Weiss and Bolton2014; Weiss et al., Reference Weiss, Murray, Zangana, Mahmooth, Kaysen, Dorsey, Lindgren, Gross, Murray, Bass and Bolton2015; Rahman et al., Reference Rahman, Hamdani, Awan, Bryant, Dawson, Khan, Azeemi, Akhtar, Nazir, Chiumento, Sijbrandij, Wang, Farooq and Van Ommeren2016; Bryant et al., Reference Bryant, Schafer, Dawson, Anjuri, Mulili, Ndogoni, Koyiet, Sijbrandij, Ulate, Harper Shehadeh, Hadzi-Pavlovic and van Ommeren2017; Bonilla-Escobar et al., Reference Bonilla-Escobar, Fandino-Losada, Martinez-Buitrago, Santaella-Tenorio, Tobon-Garcia, Munoz-Morales, Escobar-Roldan, Babcock, Duarte-Davidson, Bass, Murray, Dorsey, Gutierrez-Martinez and Bolton2018; Murray et al., Reference Murray, Hall, Dorsey, Ugueto, Puffer, Sim, Ismael, Bass, Akiba, Lucid, Harrison, Erikson and Bolton2018; Khan et al., Reference Khan, Hamdani, Chiumento, Dawson, Bryant, Sijbrandij, Nazir, Akhtar, Masood, Wang, Wang, Uddin, van Ommeren and Rahman2019), problem solving therapy (Chibanda et al., Reference Chibanda, Weiss, Verhey and Simms2016b), interpersonal psychotherapy (Bolton et al., Reference Bolton, Bass, Verdeli, Clougherty and Ndogoni2003, Reference Bolton, Bass, Betancourt, Onyango, Clougherty, Neugebauer, Murray and Verdeli2007; Bass et al., Reference Bass, Neugebauer, Clougherty, Verdeli, Wickramaratne, Ndogoni, Speelman, Weissman and Bolton2006), behavioral activation (Chowdhary et al., Reference Chowdhary, Anand, Dimidjian, Shinde, Weobong, Balaji, Hollon, Rahman, Wilson, Verdeli, Araya, King, Jordans, Fairburn, Kirkwood and Patel2016; Patel et al., Reference Patel, Weobong, Weiss, Anand, Bhat, Katti, Dimidjian, Araya, Hollon, King, Vijayakumar, Park, McDaid, Wilson, Velleman, Kirkwood and Fairburn2017; Weobong et al., Reference Weobong, Weiss, McDaid, Singla, Hollon, Nadkarni, Park, Bhat, Katti, Anand, Dimidjian, Araya, King, Vijayakumar, Wilson, Velleman, Kirkwood, Fairburn and Patel2017), cognitive behavioral therapy (Rahman et al., Reference Rahman, Malik, Sikander, Roberts and Creed2008; Maselko et al., Reference Maselko, Sikander, Bhalotra, Bangash, Ganga, Mukherjee, Egger, Franz, Bibi, Liaqat, Kanwal, Abbasi, Noor, Ameen and Rahman2015), cognitive processing therapy (Bass et al., Reference Bass, Annan, McIvor Murray, Kaysen, Griffiths, Cetinoglu, Wachter, Murray and Bolton2013), family-based interventions (Jordans et al., Reference Jordans, Tol, Ndayisaba and Komproe2013; Betancourt et al., Reference Betancourt, Ng, Kirk, Munyanah, Mushashi, Ingabire, Teta, Beardslee, Brennan, Zahn, Stulac, Cyamatare and Sezibera2014, Reference Betancourt, Ng, Kirk, Brennan, Beardslee, Stulac, Mushashi, Nduwimana, Mukunzi, Nyirandagijimana, Kalisa, Rwabukwisi and Sezibera2017), and stepped-care multi-component interventions (Araya et al., Reference Araya, Rojas, Fritsch, Gaete, Rojas, Simon and Peters2003; Rojas et al., Reference Rojas, Fritsch, Solis, Jadresic, Castillo, Gonzalez, Guajardo, Lewis, Peters and Araya2007; Patel et al., Reference Patel, Weiss, Chowdhary, Naik, Pednekar, Chatterjee, De Silva, Bhat, Araya, King, Simon, Verdeli and Kirkwood2010, Reference Patel, Weiss, Chowdhary, Naik, Pednekar, Chatterjee, Bhat, Araya, King, Simon, Verdeli and Kirkwood2011; Adewuya et al., Reference Adewuya, Adewumi, Momodu, Olibamoyo, Adesoji, Adegbokun, Adeyemo, Manuwa and Adegbaju2018; Jordans et al., Reference Jordans, Luitel, Kohrt, Rathod, Garman, De Silva, Komproe, Patel and Lund2019), among others. However, of these effective interventions, few have moved beyond the pilot phase of researcher-controlled implementation in LMICs to routine implementation at scale and with quality (Wainberg et al., Reference Wainberg, Scorza, Shultz, Helpman, Mootz, Johnson, Neria, Bradford, Oquendo and Arbuckle2017).
Almost a decade ago, four of the five highest-priority Grand Challenges in Global Health highlighted by Collins et al. (Reference Collins, Patel, Joestl, March, Insel and Daar2011) focused on improving the implementation of existing treatments and expanding access to care – hallmarks of the field of implementation science. Recently, there have been calls by researchers and funders alike to increase the focus of the field of global mental health on implementation science, given the rapidly maturing evidence-base for effective treatments in LMICs (Betancourt and Chambers, Reference Betancourt and Chambers2016). The field of implementation science focuses on developing, testing, and utilizing implementation strategies to optimize the delivery of evidence-based interventions in routine practice (Eccles and Mittman, Reference Eccles and Mittman2006). Implementation science is highly interdisciplinary, leveraging methods across traditional clinical research, the social sciences, public health, economics, political science, industrial engineering, and business to develop, test, and employ implementation strategies – methods to enhance implementation outcomes for evidence-based interventions in routine practice (Proctor et al., Reference Proctor, Powell and McMillen2013). Recently, the field has adopted specific recommendations for specifying implementation strategies (Proctor et al., Reference Proctor, Powell and McMillen2013), and Powell et al. (Reference Powell, Waltz, Chinman, Damschroder, Smith, Matthieu, Proctor and Kirchner2015) have developed an initial compilation of 73 distinct implementation strategies through the Expert Recommendations for Implementing Change (ERIC) project (Powell et al., Reference Powell, Waltz, Chinman, Damschroder, Smith, Matthieu, Proctor and Kirchner2015). The success of an implementation strategy is most often measured through improvements in the implementation outcomes of acceptability, adoption, appropriateness, cost, feasibility, fidelity, penetration, and sustainability targeting a given evidence-based intervention (Proctor et al., Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011). Given the large burden of mental disorders in LMICs and the persistent care and treatment gaps, the field of implementation science has a critical role to play as evidence-based interventions are scaled-up and optimized for delivery across LMICs.
The aim of the current study was to systematically review the existing studies focused on implementation science for depression interventions in LMICs. Given the evolving and multi-disciplinary nature of the field of implementation science, the specific terms used define it are heterogeneous and mixed. Thus, the current review included all studies conducted in an LMIC that reported an implementation outcome (Proctor et al., Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011) tied to an intervention [a program, practice, principle, procedure, product, pill, or policy (Brown et al., Reference Brown, Curran, Palinkas, Aarons, Wells, Jones, Collins, Duan, Mittman, Wallace, Tabak, Ducharme, Chambers, Neta, Wiley, Landsverk and Cheung2017)] addressing depression as at least one of the primary outcomes of interest. Given the preeminence of implementation strategies to the field of implementation science, we also abstracted implementation strategy information and coded according to ERIC classifications (Powell et al., Reference Powell, Waltz, Chinman, Damschroder, Smith, Matthieu, Proctor and Kirchner2015). We chose to focus the current review on implementation science for interventions addressing depression given it represents the largest individual burden of MNS conditions in LMICs. We hope that this paper can provide a summary of the state of implementation research for depression interventions in LMICs, and aid stakeholders in identifying gaps and prioritizing future work in this area.
Methods
Protocol, registration, and reporting guidelines
This project is registered in the PROSPERO international prospective register of systematic reviews under record ID CRD42018084203 and title ‘Implementation science for depression interventions in low- and middle-income countries: a systematic review’. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines for systematic reviews (Liberati et al., Reference Liberati, Altman, Tetzlaff, Mulrow, Gotzsche, Ioannidis, Clarke, Devereaux, Kleijnen and Moher2009), which is available in online Supplementary Appendix 1.
Search strategy
The lead author (BHW) searched four electronic bibliographic databases (PubMed; PsycINFO; CINAHL; and EMBASE) for articles published through 20 March 2019. We searched for articles including all four general search concepts, including: (1) depression; (2) an intervention, program, impact, or implementation; (3) implementation outcomes as defined by Proctor et al. (Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011); and (4) studies conducted in LMICs, as defined by the World Bank Country and Lending Groups (2018). We developed a list of terms for each concept in collaboration with an information scientist. The PsycINFO search excluded dissertations, while the CINAHL focused only on scholarly peer-reviewed journals. See online Supplementary Appendix 2 for the detailed search strategy used.
Study selection
Studies were included that: (1) were published in English; (2) were based in an LMIC according to the World Bank at the time of study data collection (including low-income; lower-middle-income; and upper-middle-income economies) (World Bank Country and Lending Groups, 2018); and (3) reported an implementation outcome as defined by Proctor et al. (Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011) tied to an intervention [a program, practice, principle, procedure, product, pill, or policy (Brown et al., Reference Brown, Curran, Palinkas, Aarons, Wells, Jones, Collins, Duan, Mittman, Wallace, Tabak, Ducharme, Chambers, Neta, Wiley, Landsverk and Cheung2017)] targeting depression as at least one of the primary outcomes of interest (see Table 1 for specific implementation outcome definitions used). Unpublished and non-peer-reviewed research studies were excluded. We utilized Covidence to import bibliographic data and screen/review studies (Covidence Systematic Review Software, 2020). Two independent reviewers from a team of five (BHW; WHH; CJ; DLA; and JMB) independently reviewed each abstract at the title/abstract, full-text review, and the extraction phase. Studies passed the title/abstract phase if depression was mentioned and it was possible that the study had been conducted in an LMIC. Disagreements were resolved through discussion until consensus was reached. Articles were excluded if the full-text was unavailable after consulting with an information scientist at the University of Washington.
Table 1. Implementation outcome definitions used for systematic review based on Proctor's implementation outcome framework (Proctor et al., Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011)

Data abstraction
Four authors (BHW; CJ; DLA; and JMB) independently piloted a structured abstraction form with five studies; all co-authors reviewed, critiqued, suggested improvements, and approved the final version. Two authors (BHW and WHH) independently abstracted study, intervention, and implementation strategy characteristics. After independently abstracting study information, the two authors (BHW and WHH) verified each abstraction, resolving any disagreement through discussion until consensus was reached. At the study level, we collected: (1) the year the study was published; (2) country and region of the study as defined by the World Bank in 2018 (World Bank Country and Lending Groups, 2018); (3) the primary research study design; (4) implementation outcomes reported; (5) detailed information on the depression intervention of interest; and (6) detailed information on implementation strategies tested (see Table 2 for categories of data abstraction).
Table 2. Study, depression intervention, implementation strategy, and implementation outcome descriptive statistics (N = 79)
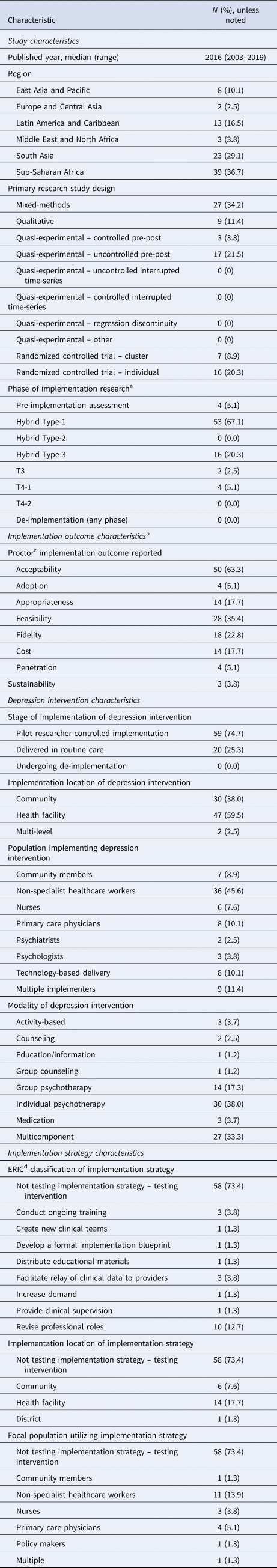
a Phase of implementation research is defined as per Fig. 1.
b More than one implementation outcome possible, thus, total percentages exceed 100%.
c Implementation outcomes were defined as per Proctor's implementation outcome framework (Proctor et al., Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011).
d ERIC classification refers to the Expert Recommendations for Implementing Change project and the list of 73 distinct implementation strategies (Powell et al., Reference Powell, Waltz, Chinman, Damschroder, Smith, Matthieu, Proctor and Kirchner2015).
We defined implementation outcomes using the Proctor implementation outcomes framework (Proctor et al., Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011) (see Table 1). All implementation outcomes required actual measurement and data reporting from target populations; for example, qualitative narrative descriptions of overall ‘lessons learned’ without explicit data reporting were excluded.
We defined the phase of implementation research for each study across a modified translational research continuum (see Fig. 1). Building on consensus definitions from systematic reviews (Fort et al., Reference Fort, Herr, Shaw, Gutzman and Starren2017) and recent efforts to situate implementation research in the traditional translational research continuum (Brown et al., Reference Brown, Curran, Palinkas, Aarons, Wells, Jones, Collins, Duan, Mittman, Wallace, Tabak, Ducharme, Chambers, Neta, Wiley, Landsverk and Cheung2017), we envision depression interventions progressing from studies testing depression interventions for efficacy in highly-controlled settings (T2-1), to pragmatic intervention effectiveness trials with increased focus on external validity (T2-2). These studies come before those focused on testing and optimizing of implementation strategies for a given depression intervention (T3). This T3 phase has been titled ‘pure implementation research’ by Curran et al. (Reference Curran, Bauer, Mittman, Pyne and Stetler2012) and most often occurs after clinical intervention effectiveness has been shown. Hybrid effectiveness-implementation trials aim to speed the transition from pragmatic effectiveness trials (T2-2) to pure implementation research (T3) and the eventual work to evaluate and optimize the scale-up of evidence-based interventions for population health impact in T4-1. Following Curran et al. (Reference Curran, Bauer, Mittman, Pyne and Stetler2012), we defined Hybrid Type-1 as those studies with a primary aim of assessing intervention effectiveness and a secondary aim to report implementation outcomes for a depression intervention. Process evaluations published separately from main trial outcomes but embedded in larger Hybrid Type-1 studies were coded as Hybrid Type-1. Studies were coded as a ‘pre-implementation assessment’ if they reported implementation outcomes prior to implementation of a given depression intervention or strategy. In Fig. 1 we situate these studies as occurring before T2-2, as in our review they most commonly occurred before depression intervention effectiveness testing. Hybrid Type-2 studies were coded as having dual primary aims of assessing intervention effectiveness and testing an implementation strategy. Hybrid Type-3 studies were coded as having the primary aim of testing an implementation strategy while reporting on intervention effectiveness or patient-level outcomes. We define phase T4-1 as studies focused on evaluating and optimizing the scale-up of interventions and strategies in routine care for population health impact. We anticipate that these studies will often make use of known evidence-based implementation strategies found effective in stage T3. The last stage of the translational research continuum (T4-2) is the continuous optimization and improvement of ongoing routine delivery of an intervention that is being delivered at scale. This phase could follow models being proposed of ‘embedded research’ (Churruca et al., Reference Churruca, Ludlow, Taylor, Long, Best and Braithwaite2019; Lieu and Madvig, Reference Lieu and Madvig2019) and/or ‘learning evaluation’ (Balasubramanian et al., Reference Balasubramanian, Cohen, Davis, Gunn, Miriam Dickinson, Miller, Crabtree and Stange2015) where implementation researchers and practitioners collaborate to continuously improve the delivery of ongoing evidence-based interventions in routine systems. We consider de-implementation as occurring at each phase of the implementation research continuum. For example, while testing real-world intervention effectiveness (T2-2), one could also nest simultaneous study of de-implementation of other ineffective, wasteful, or harmful interventions targeting the same population (T2-2-DI).

Fig. 1. Situating implementation outcomes, research designs, and other key factors across the translational highway from efficacy research (T2-1) to continuous optimization of implementation in routine care (T4-2).
We defined the depression intervention as the specific proximal program, practice, principle, procedure, product, pill, or policy (Brown et al., Reference Brown, Curran, Palinkas, Aarons, Wells, Jones, Collins, Duan, Mittman, Wallace, Tabak, Ducharme, Chambers, Neta, Wiley, Landsverk and Cheung2017) that targeted depression symptoms. For depression intervention data abstraction, we coded the level of implementation as pilot researcher-controlled implementation, whether a given depression intervention was implemented in routine care, or whether the study was focused on de-implementation of a depression intervention. We also abstracted the implementation location of the depression intervention, the population implementing the intervention, and the modality of the depression intervention. Activity-based modalities were defined as depression interventions focused on a specific behavior for decreasing symptoms, such as running, yoga, or meditation. Counseling was defined as general one-on-one meetings not focused on a specific psychotherapy, such as general HIV or life-skills counseling. Education/information was defined as passive delivery of knowledge outside of a psychotherapy or counseling context, such as pamphlets or radio spots.
We coded implementation strategies only if the primary focus of the study was testing the effect of an implementation strategy, rather than testing the effects of a depression intervention. For studies meeting these criteria, we abstracted the implementation location of a given implementation strategy, the focal population utilizing the implementation strategy, and coded implementation strategy modalities according to the ERIC project's compilation of 73 distinct implementation strategies (Proctor et al., Reference Proctor, Powell and McMillen2013; Powell et al., Reference Powell, Waltz, Chinman, Damschroder, Smith, Matthieu, Proctor and Kirchner2015).
Analysis
We imported our final reporting excel sheet into Stata 15 for analyses. Analyses focused on generating a qualitative summary of research aims, methods, approaches, implementation outcomes, implementation strategies, and depression interventions tested to date to inform future research. Descriptively, we calculated percentages for categorical variables and for our continuous variable, year study was published, we calculated the median and range. Quantitative meta-analyses of study findings were not an aim of the current study given the heterogeneity in research questions, depression interventions, implementation strategies, and outcomes reported. See online Supplementary File S1 for full data abstraction form and study data.
Results
Study selection
A total of 8714 unique studies were screened and 759 full-text articles were assessed for eligibility. Of these, 79 studies met our inclusion criteria (see Fig. 2 for PRISMA flow diagram). Of the 680 studies that were excluded at the full-text phase, the primary reason for exclusion was not reporting an implementation outcome (n = 370; 54.4%), not occurring in an LMIC (n = 86; 12.6%), not published in English (n = 52; 7.6%), and unable to locate the article full text (n = 48; 7.1%).

Fig. 2. PRISMA flow diagram.
Study characteristics
The 79 studies in our sample were published between 2003 and 2019, with the median published in 2016 and the mean being published in late 2014 (see Table 2). The number of studies has increased since 2015, with less than 10 studies published every year from 2003 to 2015, compared to 12 studies in 2016, 10 studies in 2017, 15 studies in 2018, and 8 studies published through 20 March 2019. The first three studies, published between 2003 and 2006, reported: (1) adoption and cost for the implementation strategy of ongoing training of primary health care nurses for depression treatment in Zimbabwe (Abas et al., Reference Abas, Mbengeranwa, Chagwedera, Maramba and Broadhead2003); (2) acceptability and fidelity of a psycho-educational depression intervention in Mexico (Lara et al., Reference Lara, Navarro, Acevedo, Berenzon, Mondragón and Rubí2004); and (3) the costs associated with a multi-component stepped-care depression program for treating women with depression in Chile (Araya et al., Reference Araya, Flynn, Rojas, Fritsch and Simon2006).
The majority of studies were from Sub-Saharan Africa (n = 39; 36.7%), although only eight total countries in this region were represented, with South Africa (n = 9; 31.0%), Zimbabwe (n = 6; 20.7%), and Nigeria (n = 6; 20.7%) accounting for more than half of all articles published in the region (see Fig. 3 for world map of included studies). South Asia had the second greatest representation with 23 studies (29.1%); however, these were from only three countries: India (n = 14; 60.1%), Pakistan (n = 6; 26.1%), and Nepal (n = 3; 13.0%). Thirteen studies (16.5%) were from Latin America and the Caribbean, with the majority of studies coming from Mexico (n = 5; 38.5%) and Chile (n = 4; 30.8%). East Asia and the Pacific had relatively poor representation with only eight total studies (10.1%). Only five total studies were conducted across Europe and Central Asia (n = 2; 2.5%) and Middle East and North Africa (n = 3; 3.8%).

Fig. 3. Thematic world map for distribution of included studies (N = 79).
In terms of primary study designs, the most common design was mixed-methods (n = 27; 34.2%), using both qualitative and quantitative methods to address specific primary research questions. In terms of studies utilizing primary quantitative research study designs (n = 43; 54.4%), the most common design was quasi-experimental uncontrolled pre-post (n = 17; 21.5%), followed by individual randomized trials (n = 16, 20.3%), cluster randomized trials (n = 7; 8.9%), and quasi-experimental controlled pre-post designs (n = 3; 3.8%). No studies used quasi-experimental designs with the strongest causal inference, such as controlled interrupted time-series or regression discontinuity. Nine studies used pure qualitative research designs (11.4%).
In terms of phase of implementation research, the majority of studies were Hybrid Type-1 effectiveness-implementation designs (n = 53; 67.1), followed by Hybrid Type-3 designs (n = 16; 20.3), pre-implementation assessments (n = 4; 5.1%), T4-1 (n = 4; 5.1%), and T3 (n = 2; 2.5%). No studies assessed de-implementation at any phase, utilized Hybrid Type-2 designs, or targeted the last phase of T4-2. Three of the four studies targeting phase T4-1 were conducted in Chile (Vicente et al., Reference Vicente, Kohn, Levav, Espejo, Saldivia and Sartorius2007; Alvarado et al., Reference Alvarado, Rojas, Minoletti, Alvarado and Domínguez2012; Araya et al., Reference Araya, Alvarado, Sepúlveda and Rojas2012), with one study from Zimbabwe (Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016a). For example, Araya et al. (Reference Araya, Alvarado, Sepúlveda and Rojas2012) conducted a mixed-methods study reporting on feasibility, cost, and sustainability to inform the optimization of implementation strategies for the National Depression Detection and Treatment Program which was in the process of scale-up across routine primary care in Chile. Similarly, Chibanda et al. (Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016a) reported initial appropriateness and adoption of the ‘Friendship Bench’ program as it was in the process of being scaled-up across 60 primary care facilities in Zimbabwe.
Implementation outcome characteristics
The 79 studies in our sample focused primarily on reporting early-stage implementation outcomes of acceptability (n = 50; 63.3%), feasibility (n = 28; 35.4%), and appropriateness (n = 14; 17.7%). Fidelity was also commonly measured (n = 19; 22.8%), as was cost (n = 14; 17.7%). Very few studies reported adoption (n = 4; 5.1%) or the later-stage implementation outcomes of penetration (n = 4, 5.1%) or sustainability (n = 3, 3.8%). In terms of studies reporting less-commonly reported implementation outcomes, Adewuya et al. (Reference Adewuya, Adewumi, Momodu, Olibamoyo, Adesoji, Adegbokun, Adeyemo, Manuwa and Adegbaju2018) reported adoption as the percentage of trained nurses (95.2%) who actively were delivering a pilot multicomponent screening, psychoeducation, psychological therapy, and medication intervention in primary care settings in Nigeria. Chatterjee et al. (Reference Chatterjee, Chowdhary, Pednekar, Cohen, Andrew, Andrew, Araya, Simon, King, Telles, Verdeli, Clougherty, Kirkwood and Patel2008) reported penetration as the percentage of patients (53%) who tested positive for a common mental disorder – including depression – who received the first session of psycho-education in their project testing the revision of professional roles (task-shifting) for a multicomponent depression intervention in routine primary care in India. Abas et al. (Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016) reported on the quantitative sustainability of ‘Friendship Bench’ project activities up to 8 years after the initial pilot project ended and the depression intervention was formally integrated into routine care settings in Zimbabwe.
Depression intervention characteristics
Seventy-five percent (n = 59) of depression interventions included in the studies occurred as part of pilot researcher-controlled implementation, rather than being implemented under routine care conditions. For example, in a Hybrid Type-1 study, Khan et al. (Reference Khan, Hamdani, Chiumento, Dawson, Bryant, Sijbrandij, Nazir, Akhtar, Masood, Wang, Wang, Uddin, van Ommeren and Rahman2019) reported the acceptability, feasibility, and initial clinical outcomes for patients attended by lay health workers randomized to implement group-based problem management plus (PM+) compared with enhanced usual care in Pakistan. Thus, the primary aim of this study was to test group PM+ as a novel depression intervention rather than testing an implementation strategy to enhance implementation outcomes for a depression intervention being delivered in routine implementation settings, as would occur in a Hybrid Type-3 or T3 study (see Table 3 for detailed study descriptions). By contrast, in a Hybrid Type-3 study, Shidhaye et al. (Reference Shidhaye, Murhar, Gangale, Aldridge, Shastri, Parikh, Shrivastava, Damle, Raja, Nadkarni and Patel2017) reported the costs associated with an implementation strategy focused on increasing population-level demand for the existing routine depression care. The primary aim of their study was increase contact coverage of existing routinely-implemented depression interventions.
Table 3. Included studies (N = 79) and associated detailed study, intervention, and implementation strategy information

The depression interventions of interest were most often delivered at the health facility level (n = 47; 59.5), followed by the community level (n = 30; 38.0%), and multi-level programs (n = 2; 2.5%). Most depression interventions were delivered by non-specialist healthcare workers (n = 36; 45.6%) who did not have specific specialist mental health training and were not trained as a nurse or other clinical providers. Other common providers included team-based delivery (9, 11.4%); primary care physicians (8, 10.1%), and technology-based delivery (8, 10.1%). The modality for depression intervention was most commonly individual psychotherapy (n = 30, 38.0%), followed by multi-component interventions (n = 27; 33.3%) that commonly included both psychotherapy and psychotropic medication. Group psychotherapy was also common, with 14 studies (17.3%). Few studies focused on medication alone (n = 3; 3.7%), activity-based treatments (n = 3; 3.7%), or education/information (n = 1; 1.2%).
Implementation strategy characteristics
Seventy-three percent of studies (n = 58) had the primary aim of testing the depression intervention of interest, rather than testing an implementation strategy to enhance implementation outcomes for a given depression intervention. Of the 21 studies (26.5%) testing an implementation strategy, the majority employed the strategy at the health facility level (n = 14; 66.6%), followed by the community (n = 6; 28.6%) and the district levels (n = 1; 4.8%). For example, in a Hybrid Type-3 study, Maulik et al. (Reference Maulik, Tewari, Devarapalli, Kallakuri and Patel2016) assessed the acceptability and feasibility of a community-based electronic decision-support implementation strategy to facilitate the relay of clinical data from non-specialist health workers in the community to primary care providers to improve routinely-provided public-sector depression care in India. Additionally, Jordans et al. (Reference Jordans, Luitel, Kohrt, Rathod, Garman, De Silva, Komproe, Patel and Lund2019) reported fidelity and penetration resulting from an implementation strategy to work with policy-makers at the district level to develop a formal implementation blueprint focused on improving routinely-delivered depression care in Nepal.
Of the 21 studies testing implementation strategies, the majority employed non-specialist healthcare workers in strategy implementation (n = 11; 52%), followed by primary care physicians (n = 4; 19.0%) and nurses (n = 3; 14.2%). The ERIC classification of implementation strategies highlighted revising professional roles as the dominant strategy (n = 10; 47.6%). These studies primarily focused on testing task-sharing approaches to optimize implementation outcomes of depression interventions. For example, Alvarado et al. (Reference Alvarado, Rojas, Minoletti, Alvarado and Domínguez2012) studied the cost and sustainability of revising the professional roles of primary care providers to implement a stepped-care multicomponent depression treatment program in routine care settings in Chile. Buttorff et al. (Reference Buttorff, Hock, Weiss, Naik, Araya, Kirkwood, Chisholm and Patel2012) reported the cost and penetration of testing the strategy of revising professional roles to have non-specialist workers deliver depression care in routine primary care settings in India.
Other implementation strategies commonly tested included facilitating the relay of clinical data to providers (n = 3; 14.3%) and conducting ongoing training (n = 3; 14.3%). For example, Tewari et al. (Reference Tewari, Kallakuri, Devarapalli, Jha, Patel and Maulik2017) reported the acceptability, feasibility, and fidelity of a community-based electronic decision-support implementation strategy to facilitate the relay of clinical depression data from the community to primary care providers in India. Gureje et al. (Reference Gureje, Abdulmalik, Kola, Musa, Yasamy and Adebayo2015) reported fidelity associated with the conducting ongoing training of primary healthcare workers in the WHO Mental Health Gap Action Programme Intervention Guide to integrate depression treatment with primary care in Nigeria. Five of the eight distinct ERIC strategies tested were covered by only one study, including: (1) creating new clinical teams; (2) developing a formal implementation blueprint; (3) distributing educational materials; (4) increasing demand; and (5) providing clinical supervision. Sixty-five of the 73 distinct ERIC strategies were not represented by studies in our sample.
Discussion
Our systematic review found a relatively large body of implementation research targeting depression interventions in LMICs. Researchers are increasing their use of modern methods in implementation science, with a growing focus on reporting implementation outcomes, testing implementation strategies, and using pragmatic study designs to optimize the delivery of evidence-based interventions in routine settings. Nevertheless, our review identified significant gaps in the literature. The vast majority of existing implementation research focuses on early-stage implementation outcomes, such as acceptability, appropriateness, and feasibility, with a paucity of studies focusing on later-stage outcomes such as cost, penetration, and sustainability. In addition, only one quarter of studies had the primary aim of testing an implementation strategy. The majority of studies reported implementation outcomes as part of a ‘process evaluation’ complementary to a pragmatic trial or pilot study focused on evaluating clinical effectiveness for a depression intervention. Thus, the bulk of studies identified in our review were labeled as ‘Hybrid Type-1 effectiveness-implementation’ designs (Curran et al., Reference Curran, Bauer, Mittman, Pyne and Stetler2012). With this continued focus on clinical effectiveness, it is no surprise that three quarters of included studies were studying a depression intervention delivered under pilot researcher-controlled implementation, rather than in routine care. Furthermore, we found only four studies that were focused on evaluating and optimizing the scale-up of depression interventions for population health impact in LMICs. We also found specific LMIC regions with few existing studies, including the Middle East and North Africa and Europe and Central Asia. Overall, our findings corroborate a recent systematic review focused on implementation science for stigma reduction interventions in LMICs (Kemp et al., Reference Kemp, Jarrett, Kwon, Song, Jetté, Sapag, Bass, Murray, Rao and Baral2019a) which found that the majority of studies utilized Hybrid Type-1 designs, qualitative research methods, and reported the implementation outcomes of acceptability and feasibility.
Assessing depression intervention effectiveness in a randomized controlled trial along with a mixed-methods process evaluation to assess early-stage implementation outcomes tied to depression intervention acceptability, appropriateness, feasibility, or initial fidelity is an optimal approach for a Hybrid Type-1 research design. Yet, even among the 57 studies at this stage, only two (Murray et al., Reference Murray, Dorsey, Haroz, Lee, Alsiary, Haydary, Weiss and Bolton2014; Adewuya et al., Reference Adewuya, Adewumi, Momodu, Olibamoyo, Adesoji, Adegbokun, Adeyemo, Manuwa and Adegbaju2018) reported the early-stage implementation outcome of adoption. This is not surprising since pilot researcher-controlled implementation projects often hire separate research staff as implementers and thus ‘non-participation’ (or lack of adoption) of these separate paid staff is not common. Nevertheless, the lack of reporting on adoption, paired with the dearth of studies reporting on penetration, means that little is known regarding the uptake, initial implementation, or potential routine institutionalization of depression interventions in LMICs – key implementation outcomes for effective and sustained scale-up of depression interventions. Future research, even at T2-2 and Hybrid Type-1 stages, could focus on approximating real-world routine implementation conditions to allow effective reporting of provider and organizational adoption and implementation costs. Where possible, these studies should also build in funding for assessment of later-stage penetration and sustainability (maintenance) once research-based implementation has ended as has been advocated by the RE-AIM evaluation framework for decades (Glasgow et al., Reference Glasgow, Vogt and Boles1999). Researchers working at this stage could also consider increased utilization of high-quality quasi-experimental designs with optimal design features for causal inference, rather than the current dominance of randomized trials and poor-quality uncontrolled pre-post quasi-experimental designs (Bärnighausen et al., Reference Bärnighausen, Tugwell, Røttingen, Shemilt, Rockers, Geldsetzer, Lavis, Grimshaw, Daniels, Brown, Bor, Tanner, Rashidian, Barreto, Vollmer and Atun2017; Geldsetzer and Fawzi, Reference Geldsetzer and Fawzi2017; Reeves et al., Reference Reeves, Wells and Waddington2017). The highest-quality quasi-experimental designs for causal inference in routine implementation settings of controlled interrupted time-series (Bernal et al., Reference Bernal, Cummins and Gasparrini2017) and regression discontinuity (Bor et al., Reference Bor, Moscoe, Mutevedzi, Newell and Bärnighausen2014) were not represented in our review.
Of the 21 studies testing implementation strategies, over 70% (n = 16) were Hybrid Type-3 designs, followed by studies at phases T3 (n = 2; 9.5%), and T4-1 (n = 3; 14.3%). Compared to Hybrid Type-1 studies, Hybrid Type-3 studies were more likely to use quasi-experimental designs (7 of 16; 43.8% v. 10 of 53; 18.9%) and less likely to use randomized designs (2 of 16; 12.5% v. 21 of 53; 39.6%). Furthermore, no study with a primary aim to test an implementation strategy used individual randomization, compared to 27.6% (17 of 58) of studies with a primary aim to test intervention effectiveness. This pattern is in line with the fact that pragmatic cluster randomized trials and high-quality quasi-experimental designs are the gold standard research designs for testing and optimizing implementation strategies for an intervention delivered in routine care. Using individual randomization at the later phases of the implementation research continuum is logistically difficult, and can potentially alter routine systems of implementation, decreasing both internal and external validity. As expected, implementation outcome distributions were similar across Hybrid Type-1 and Hybrid Type-3 studies. The six studies situated at T3 and T4-1 were more likely to focus on the later-stage implementation outcomes of cost (n = 3; 50.0%) and sustainability (n = 2; 33.3%); these studies were also more likely to report adoption (n = 2; 33.3%). As visualized in Fig. 1, we suggest that the most relevant implementation outcomes at the testing implementation strategy phase (T3) are similar at T2-2 or when using Hybrid designs. Although, at stage T3, implementation outcome reporting should target both the implementation strategy being tested along with the target depression intervention. For example, if testing an implementation strategy to improve the adoption of a depression intervention, researchers will also be interested in measuring, assessing, and optimizing the adoption of the implementation strategy.
Almost half of the 21 studies testing implementation strategies focused on assessing the effectiveness of revising professional roles, most often through task-sharing to provide depression care led by primary care providers or lay health workers in a stepped-care approach supervised by specialist providers. Only eight of the 73 distinct ERIC implementation strategies (Powell et al., Reference Powell, Waltz, Chinman, Damschroder, Smith, Matthieu, Proctor and Kirchner2015) had any representation in our review, with five strategies being tested in only one study. For efficient generation of evidence given the large number of potential distinct implementation strategies – not to mention multicomponent or blended groups of strategies – we suggest future implementation research considers increased use of adaptive trial designs, such as sequential multiple assignment randomized trials (SMART); (Lei et al., Reference Lei, Nahum-shani, Lynch, Oslin and Murphy2012) or multiphase optimization strategy trials (MOST) (Collins et al., Reference Collins, Murphy and Strecher2007) which can allow testing multiple strategies across multiple doses in a single trial. Quasi-experimental designs, natural experiments, and descriptive analyses utilizing routine data systems and naturally-occurring heterogeneity in implementation strategies should also be prioritized to help rapidly identify, test, and optimize the scale-up of promising implementation strategies in LMICs (Wagenaar et al., Reference Wagenaar, Sherr, Fernandes and Wagenaar2016).
Overall, our findings that the majority of existing implementation studies on depression interventions in LMICs are utilizing Hybrid Type-1 designs could reflect three things. First, that researchers and implementers working in LMICs do not believe we have sufficient evidence for depression intervention effectiveness across diverse contexts to move to later implementation research phases. Second, few researchers and implementers have the necessary skills or knowledge to effectively extend past traditional clinical research designs focused on depression intervention effectiveness testing toward testing implementation strategies (T3), optimizing scale-up in routine systems settings (T4-1), or continuous optimization in routine systems settings (T4-2). Third, research funders have yet to fully embrace the field of implementation science and the value of moving beyond traditional clinical research paradigms.
To address the first point, we argue that with the publishing of the Disease Control Priorities, 3rd Edition in 2016 outlining that sufficient evidence exists for effectiveness and cost-effectiveness for depression interventions globally (Patel et al., Reference Patel, Chisholm, Parikh, Charlson, Degenhardt, Dua, Ferrari, Hyman, Laxminarayan, Levin, Lund, Medina Mora, Petersen, Scott, Shidhaye, Vijayakumar, Thornicroft and Whiteford2016), the time is now for increased investments in implementation research and to move beyond testing intervention effectiveness and toward testing implementation strategies (T3), scale-up (T4-1), and continuous optimization of routine implementation (T4-2). The second point will require the development and re-training of a pipeline of researchers with expertise outside of traditional clinical research paradigms centered on highly-controlled randomized trials as the lone gold standard research design. As the field of global mental health progresses away from pragmatic clinical intervention studies and toward optimizing the scaling-up (T4-1) of best-evidence interventions and associated implementation strategies and continuous ‘embedded research’ and ‘learning evaluation’ of interventions and strategies already scaled-up (T4-1), we anticipate that a number of key evolutions will occur. Implementation outcome reporting will center on later stage costs, fidelity, penetration, and sustainability of both interventions and implementation strategies. Clinical researchers will have to be re-trained or partner with various disciplinary experts to implement analytical designs focused more on high-quality quasi-experimental approaches, continuous improvement and systems optimization borrowing from industrial engineering and business domains, along with novel systems modeling approaches (Royston, Reference Royston2011; Sherr et al., Reference Sherr, Gimbel, Rustagi, Nduati, Cuembelo, Farquhar, Wasserheit and Gloyd2014; Wagner et al., Reference Wagner, Crocker, Liu, Cherutich, Gimbel, Fernandes, Mugambi, Ásbjörnsdóttir, Masyuko, Wagenaar, Nduati and Sherr2019). These methods will be of increasing importance due to the need to model, test, and continuously improve complex webs of multiple evidence-based interventions and implementation strategies for depression operating across contexts and in non-linear pathways (Galea et al., Reference Galea, Riddle and Kaplan2010; Kemp et al., Reference Kemp, Wagenaar and Haroz2019b). Studies operating at the level of entire districts, provinces, or nations in LMICs will have the necessary primary focus on external validity and will focus on continuous reporting of implementation outcomes using routine data systems (Victora et al., Reference Victora, Habicht and Bryce2004; Wagenaar et al., Reference Wagenaar, Sherr, Fernandes and Wagenaar2016). To catalyze later phases of implementation research in LMICs, funding agencies, governments, and stakeholders will need to recognize their role in funding ongoing real-world implementation of depression interventions, not simply focusing on funding one-off research-based implementation projects.
This review has several important limitations. First, given available resources, we were only available to review papers published in English, likely systematically excluding studies emanating from certain LMICs. Second, this review focused on peer-reviewed studies. Given the barriers to publishing in international peer-reviewed journals, especially for LMIC investigators, this likely biases our findings to papers published by internationally-connected and funded investigators. Third, given the heterogeneous language and terminology used in the burgeoning field of implementation science, making strict distinctions between ‘evidence-based depression interventions’ and ‘implementation strategies’ of interest, as well as coding implementation strategies into distinct ERIC classifications (Powell et al., Reference Powell, Waltz, Chinman, Damschroder, Smith, Matthieu, Proctor and Kirchner2015) is challenging. Similarly, coding the stage of implementation research is also difficult and somewhat qualitative in nature, as implementation researchers themselves have not adopted a comprehensive and common language to situate their studies along the implementation research continuum. Fourth, given the size of this review, we focused data abstraction on implementation outcomes and high-level coding of depression intervention characteristics. We did not abstract detailed information on implementation context, the use of implementation science frameworks, or on the diversity of specific depression interventions – areas that could be of interest for future systematic reviews. Last, we did not code the level of analysis for implementation outcomes which we suggest future researchers conduct. This is important to distinguish, for example, client-level adoption or sustainability (reach and maintenance, respectively in the RE-AIM framework, Glasgow et al., Reference Glasgow, Vogt and Boles1999) from provider- or organizational-level adoption or sustainability.
Conclusions
Our systematic review of implementation outcomes and strategies for depression interventions in LMICs found that existing research has focused largely on early-stage implementation outcomes. Most studies had the primary aim of testing the pragmatic effectiveness of a depression intervention in pilot researcher-controlled settings paired with a ‘process evaluation’ to collect information on implementation context. Thus, the majority of studies were Hybrid Type-1 effectiveness-implementation designs, with very few studies focused on evaluating and optimizing strategies for scale-up of depression interventions in routine care. Even though the ostensible focus of the field of implementation science is to test implementation strategies to optimize the real-world implementation of evidence-based interventions, only a quarter of studies had a primary aim to test implementation strategies for interventions implemented in routine care. Approximately half of these studies testing implementation strategies were focused on testing revised professional roles, or task-shifting, for depression intervention implementation. Only eight of the 73 distinct ERIC implementation strategies were represented in our systematic review. Future implementation research should focus on testing implementation strategies and optimizing the use of evidence-based strategies to scale-up and improve the quality of routine depression care. These studies should use high-quality pragmatic research designs such as controlled interrupted time-series, regression discontinuity, stepped-wedge randomized trials, and novel complex systems modeling approaches, as well as focus on later-stage implementation outcomes such as cost, penetration, and sustainability. Certain LMIC regions, such as Middle East and North Africa and Europe and Central Asia could be prioritized for investments given the paucity of existing studies.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/gmh.2020.1.
Data
All data are available in online Supplementary File S1.
Author contributions
BHW conceived the idea. CGK provided assistance with the search strategy and systematic review methods. All authors contributed to article review, data extraction, and data interpretation. All authors read and approved the final manuscript.
Financial support
BHW was supported by grant number K01MH110599 from the U.S. National Institute of Mental Health. CGK was supported by grant number F31MH112397 from the U.S. National Institute of Mental Health. JMB was supported by a Postdoctoral Fellowship grant from the Canadian Institutes of Health Research (CIHR). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or CIHR.
Conflict of interest
The authors report no conflict of interest.
Ethical standards
N/A, systematic review.
Consent for publication
N/A, systematic review.










