Abstract
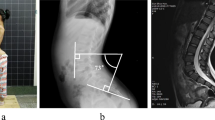
A 15-year-old female former gymnast with a history of pectus excavatum was reviewed due to unexplained paraparesis and urinary incontinence since age 10. Symptoms were commenced with intolerable upper back pain and development of a soft mass at the sacrum that remitted spontaneously. Brain and whole spine MRI imaging and blood and CSF testing were normal. The combination of skeletal, neurological, and bladder symptoms with normal lumbar MRI and abnormal urodynamic and neurophysiological studies led to the clinical suspicion of occult tethered cord syndrome (oTCS). Surgical cord “untethering” was performed leading to remarkable postoperative clinical improvement. oTCS is a recently defined functional disorder of the spinal cord due to fixation (tethering) of the conus medullaris by inelastic elements that may lead to severe neurological impairment. High clinical suspicion is required as oTCS is a treatable spinal cord disorder.


Similar content being viewed by others
Data availability
Data and material are available upon request.
References
Yamada S, Zinke DE, Sanders D. (1981) Pathophysiology of “tethered cord syndrome.” J Neurosurg 54:494–503 https://doi.org/10.3171/jns.1981.54.4.0494
Raghavan N, Barkovich AJ, Edwards M (1989) MR imaging in the tethered spinal cord syndrome. AJR Am J Roentgenol 152(4):843–852. https://doi.org/10.2214/ajr.152.4.843
Selçuki M, Vatansever S, Inan S, Erdemli E, Bağdatoğlu C, Polat A (2003) Is a filum terminale with a normal appearance really normal? Childs Nerv Syst 19(1):3–10
Tu A, Steinbok P (2013) Occult tethered cord syndrome: a review. Childs Nerv Syst 29:1635–1640. https://doi.org/10.1007/s00381-013-2129-1
Broderick KM, Munoz O, Herndon CDA, Joseph DB, Kitchens DM (2015) Utility of urodynamics in the management of asymptomatic tethered cord in children. World J Urol 33(8):1139–1142. https://doi.org/10.1007/s00345-014-1414-2
Leung V, Pugh J, Norton JA (2015) Utility of neurophysiology in the diagnosis of tethered cord syndrome J. Neurosurg Pediatr 15(4):434–437. https://doi.org/10.3171/2014.10.PEDS1434
Wehby MC, O’Hollaren PS, Abtin K, Hume JL, Richards BJ (2004) Occult tight filum terminale syndrome: results of surgical untethering. Pediatr Neurosurg 40:51–57. https://doi.org/10.1159/000078908
Kanda S, Akiyama T, Chikuda H, Yamaguchi T, Saita K (2015) An unusual presentation of adult tethered cord syndrome associated with severe chest and upper Back pain. Case Rep Orthop 2015:926185–926185. https://doi.org/10.1155/2015/926185
James HE, Schut L (1974) The spontaneous remission of a large sacro-coccygeal lipomeningocele sac with presentation of a tethered cord syndrome neuropadiatrie. 5(3):340–343. https://doi.org/10.1055/s-0028-1091713
Filippidis AS, Kalani MY, Theodore N, Rekate HL (2010) Spinal cord traction, vascular compromise, hypoxia, and metabolic derangements in the pathophysiology of tethered cord syndrome. Neurosurg Focus 29:E9. https://doi.org/10.3171/2010.3.FOCUS1085
Cornette L, Verpoorten C, Casaer P (1998) Concerning the article by Andar UB et al. Pediatr Neurosurg 1997; 26: 17-24: upper and lower motor neuron dysfunction in closed spinal dysraphism. Pediatr Neurosurg 29(4):222–223. https://doi.org/10.1159/000028726
Levin KH, Daube JR, Spinal Cord Infarction (1984) Another cause of “lumbosacral Polyradiculopathy”. Neurology. 34(3):389–390. https://doi.org/10.1212/wnl.34.3.389
Horowitz SH, Patel N (2003) Peripheral neurophysiology of acute distal spinal cord infarction. Pediatr Neurol 28(1):64–65. https://doi.org/10.1016/s0887-8994(02)00495-2
Caton MT, Huff JS (2020) Spinal cord ischemia. [Updated 2019 Jun 8]. In: StatPearls [Internet]. Treasure Island (FL). StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK539870/
Acknowledgments
The author would like to thank the patient and the family.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Informed consent
Patient’s consent to participate and for publication are available upon request.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsiptsios, D., Sysoev, K., Anastasiadis, A. et al. Occult tethered cord syndrome: a reversible cause of paraparesis not to be missed. Childs Nerv Syst 36, 2089–2092 (2020). https://doi.org/10.1007/s00381-020-04701-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04701-8