Abstract
Purpose
To define the relationship between 3D radiological features, psychological factors, and back pain prevalence and intensity in patients with adolescent idiopathic scoliosis (AIS).
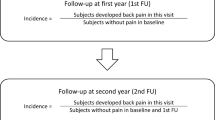
Methods
Consecutive AIS patients answered self-reported questionnaires and underwent simultaneous posterior–anterior and lateral scans of the spine (EOS Imaging, Paris, France). 3D reconstructions of the spine and pelvis reported 18 parameters in the coronal, sagittal, and axial plane.
Results
Hundred and twenty-four patients with AIS were included in the study. Overall, 90% of AIS patients reported having some back pain over the last 6 months and 85.8% over the last 30 days. Pain intensity in the last month was reported to be mild in 37.5%, moderate in 31.8%, moderate to severe in 24.3%, and severe in 6.54% of cases. Location of back pain was associated with location of main curve (P = 0.036). Low back pain was associated with higher lumbar apical AVR and lower lumbar lordosis (P < 0.05). Independent risk factors for back pain in AIS were pain catastrophizing (B = 0.061, P = 0.035), poorer self-reported state of mental health (B = − 0.872, P = 0.023), decreased thoracic kyphosis (B = − 0.033, P = 0.044) and greater pelvic asymmetry (B = 0.146, P = 0.047). There was a significant association between self-reported pain intensity in the last 24 h and levels of catastrophizing. Pain catastrophizing level influenced the relationship between deformity severity and pain intensity. In low catastrophizers, there was a significant association between greater deformity severity and higher pain levels.
Conclusions
Back pain in AIS is multifactorial and associated with psychological and morphological parameters. Pain catastrophizing is an important construct in AIS-related pain and should be taken into consideration when evaluating these patients.





Similar content being viewed by others
References
Teles AR, Ocay DD, Bin Shebreen A, Tice A, Saran N, Ouellet JA, Ferland CE (2019) Evidence of impaired pain modulation in adolescents with idiopathic scoliosis and chronic back pain. Spine J 19:677–686. https://doi.org/10.1016/j.spinee.2018.10.009
Landman Z, Oswald T, Sanders J, Diab M, Spinal Deformity Study G (2011) Prevalence and predictors of pain in surgical treatment of adolescent idiopathic scoliosis. Spine 36:825–829. https://doi.org/10.1097/BRS.0b013e3181de8c2b
Ramirez N, Johnston CE, Browne RH (1997) The prevalence of back pain in children who have idiopathic scoliosis. J Bone Joint Surg Am 79:364–368
Theroux J, Le May S, Fortin C, Labelle H (2015) Prevalence and management of back pain in adolescent idiopathic scoliosis patients: a retrospective study. Pain Res Manag 20:153–157
Morse LJ, Kawakami N, Lenke LG, Sucato DJ, Sanders JO, Diab M (2012) Culture and ethnicity influence outcomes of the Scoliosis Research Society Instrument in adolescent idiopathic scoliosis. Spine 37:1072–1076. https://doi.org/10.1097/BRS.0b013e31823ed962
Pellegrino LN, Avanzi O (2014) Prospective evaluation of quality of life in adolescent idiopathic scoliosis before and after surgery. J Spinal Disord Tech 27:409–414. https://doi.org/10.1097/BSD.0b013e3182797a5e
Weiss HR (2008) Adolescent idiopathic scoliosis (AIS)—an indication for surgery? A systematic review of the literature. Disabil Rehabil 30:799–807. https://doi.org/10.1080/09638280801889717
Balague F, Pellise F (2016) Adolescent idiopathic scoliosis and back pain. Scoliosis Spinal Disord 11:27. https://doi.org/10.1186/s13013-016-0086-7
Matamalas A, Bago J, D'Agata E, Pellise F (2014) Body image in idiopathic scoliosis: a comparison study of psychometric properties between four patient-reported outcome instruments. Health Qual Life Outcomes 12:81. https://doi.org/10.1186/1477-7525-12-81
Bisson D, Lama D, Abduljabbar F, Rosenzweig DH, Saran N, Ouellet JA, Haglund L (2018) Facet joint degeneration in adolescent idiopathic scoliosis. JOR Spine. https://doi.org/10.1002/jsp2.1016
Ferrero E, Lafage R, Diebo BG, Challier V, Illharreborde B, Schwab F, Skalli W, Guigui P, Lafage V (2017) Tridimensional analysis of rotatory subluxation and sagittal spinopelvic alignment in the setting of adult spinal deformity. Spine Deform 5:255–264. https://doi.org/10.1016/j.jspd.2017.01.003
Trammell TR, Schroeder RD, Reed DB (1988) Rotatory olisthesis in idiopathic scoliosis. Spine 13:1378–1382
Shen J, Kadoury S, Labelle H, Roy-Beaudry M, Aubin CE, Parent S (2017) Geometric torsion in adolescent idiopathic scoliosis: a new method to differentiate between Lenke 1 subtypes. Spine 42:E532–E538. https://doi.org/10.1097/BRS.0000000000001866
Shen J, Kadoury S, Labelle H, Parent S (2016) Geometric torsion in adolescent idiopathic scoliosis: a surgical outcomes study of lenke type 1 patients. Spine 41:1903–1907. https://doi.org/10.1097/BRS.0000000000001651
Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC (2001) Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain 17:52–64
Severeijns R, Vlaeyen JW, van den Hout MA, Weber WE (2001) Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clin J Pain 17:165–172
Wojtowicz AA, Greenley RN, Gumidyala AP, Rosen A, Williams SE (2014) Pain severity and pain catastrophizing predict functional disability in youth with inflammatory bowel disease. J Crohns Colitis 8:1118–1124. https://doi.org/10.1016/j.crohns.2014.02.011
Asmundson GJ, Noel M, Petter M, Parkerson HA (2012) Pediatric fear-avoidance model of chronic pain: foundation, application and future directions. Pain Res Manag 17:397–405
Vervoort T, Eccleston C, Goubert L, Buysse A, Crombez G (2010) Children's catastrophic thinking about their pain predicts pain and disability 6 months later. Eur J Pain 14:90–96. https://doi.org/10.1016/j.ejpain.2009.03.001
Crombez G, Bijttebier P, Eccleston C, Mascagni T, Mertens G, Goubert L, Verstraeten K (2003) The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. Pain 104:639–646
Guite JW, McCue RL, Sherker JL, Sherry DD, Rose JB (2011) Relationships among pain, protective parental responses, and disability for adolescents with chronic musculoskeletal pain: the mediating role of pain catastrophizing. Clin J Pain 27:775–781. https://doi.org/10.1097/AJP.0b013e31821d8fb4
Walker LS, Sherman AL, Bruehl S, Garber J, Smith CA (2012) Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain 153:1798–1806. https://doi.org/10.1016/j.pain.2012.03.026
Miro J, Castarlenas E, Huguet A (2009) Evidence for the use of a numerical rating scale to assess the intensity of pediatric pain. Eur J Pain 13:1089–1095. https://doi.org/10.1016/j.ejpain.2009.07.002
Ruskin D, Lalloo C, Amaria K, Stinson JN, Kewley E, Campbell F, Brown SC, Jeavons M, McGrath PA (2014) Assessing pain intensity in children with chronic pain: convergent and discriminant validity of the 0 to 10 numerical rating scale in clinical practice. Pain Res Manag 19:141–148
Beausejour M, Joncas J, Goulet L, Roy-Beaudry M, Parent S, Grimard G, Forcier M, Lauriault S, Labelle H (2009) Reliability and validity of adapted French Canadian version of Scoliosis Research Society Outcomes Questionnaire (SRS-22) in Quebec. Spine 34:623–628. https://doi.org/10.1097/BRS.0b013e3181973e58
Parkerson HA, Noel M, Page MG, Fuss S, Katz J, Asmundson GJ (2013) Factorial validity of the English-language version of the Pain Catastrophizing Scale–child version. J Pain 14:1383–1389. https://doi.org/10.1016/j.jpain.2013.06.004
Pielech M, Ryan M, Logan D, Kaczynski K, White MT, Simons LE (2014) Pain catastrophizing in children with chronic pain and their parents: proposed clinical reference points and reexamination of the Pain Catastrophizing Scale measure. Pain 155:2360–2367. https://doi.org/10.1016/j.pain.2014.08.035
Canals J, Marti-Henneberg C, Fernandez-Ballart J, Cliville R, Domenech E (1992) Scores on the State-Trait Anxiety Inventory for children in a longitudinal study of pubertal Spanish youth. Psychol Rep 71:503–512. https://doi.org/10.2466/pr0.1992.71.2.503
Schisler T, Lander J, Fowler-Kerry S (1998) Assessing children's state anxiety. J Pain Symptom Manag 16:80–86
Julian LJ (2011) Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken) 63(Suppl 11):S467–472. https://doi.org/10.1002/acr.20561
Sangole A, Aubin CE, Labelle H, Lenke L, Jackson R, Newton P, Stokes IA, Scoliosis Research Society DSC (2010) The central hip vertical axis: a reference axis for the Scoliosis Research Society three-dimensional classification of idiopathic scoliosis. Spine 35:E530–534. https://doi.org/10.1097/BRS.0b013e3181da38b8
Sekiya T, Aota Y, Yamada K, Kaneko K, Ide M, Saito T (2018) Evaluation of functional and structural leg length discrepancy in patients with adolescent idiopathic scoliosis using the EOS imaging system: a prospective comparative study. Scoliosis Spinal Disord 13:7. https://doi.org/10.1186/s13013-018-0152-4
Ferrero E, Lafage R, Challier V, Diebo B, Guigui P, Mazda K, Schwab F, Skalli W, Lafage V (2015) Clinical and stereoradiographic analysis of adult spinal deformity with and without rotatory subluxation. Orthop Traumatol Surg Res 101:613–618. https://doi.org/10.1016/j.otsr.2015.04.008
Steib JP, Dumas R, Mitton D, Skalli W (2004) Surgical correction of scoliosis by in situ contouring: a detorsion analysis. Spine 29:193–199. https://doi.org/10.1097/01.BRS.0000107233.99835.A4
Boyer L, Shen J, Parent S, Kadoury S, Aubin CE (2018) Accuracy and precision of seven radiography-based measurement methods of vertebral axial rotation in adolescent idiopathic scoliosis. Spine Deform 6:351–357. https://doi.org/10.1016/j.jspd.2017.12.004
Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 83:1169–1181
Theroux J, Le May S, Hebert JJ, Labelle H (2017) Back pain prevalence is associated with curve-type and severity in adolescents with idiopathic scoliosis: a cross-sectional study. Spine 42:E914–E919. https://doi.org/10.1097/BRS.0000000000001986
Djurasovic M, Glassman SD, Sucato DJ, Lenke LG, Crawford CH 3rd, Carreon LY (2018) Improvement in scoliosis research society-22r pain scores after surgery for adolescent idiopathic scoliosis. Spine 43:127–132. https://doi.org/10.1097/BRS.0000000000001978
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, Pencina MJ, Kattan MW (2010) Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21:128–138. https://doi.org/10.1097/EDE.0b013e3181c30fb2
Topalis C, Grauers A, Diarbakerli E, Danielsson A, Gerdhem P (2017) Neck and back problems in adults with idiopathic scoliosis diagnosed in youth: an observational study of prevalence, change over a mean four year time period and comparison with a control group. Scoliosis Spinal Disord 12:20. https://doi.org/10.1186/s13013-017-0125-z
Sato T, Hirano T, Ito T, Morita O, Kikuchi R, Endo N, Tanabe N (2011) Back pain in adolescents with idiopathic scoliosis: epidemiological study for 43,630 pupils in Niigata City, Japan. Eur Spine J 20:274–279. https://doi.org/10.1007/s00586-010-1657-6
Calvo-Munoz I, Gomez-Conesa A, Sanchez-Meca J (2013) Prevalence of low back pain in children and adolescents: a meta-analysis. BMC Pediatr 13:14. https://doi.org/10.1186/1471-2431-13-14
Kovacs FM, Gestoso M, Gil del Real MT, Lopez J, Mufraggi N, Mendez JI (2003) Risk factors for non-specific low back pain in schoolchildren and their parents: a population based study. Pain 103:259–268
Barrey C, Roussouly P, Le Huec JC, D'Acunzi G, Perrin G (2013) Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J 22(Suppl 6):S834–841. https://doi.org/10.1007/s00586-013-3030-z
Quinn KP, Dong L, Golder FJ, Winkelstein BA (2010) Neuronal hyperexcitability in the dorsal horn after painful facet joint injury. Pain 151:414–421. https://doi.org/10.1016/j.pain.2010.07.034
Sabharwal S, Zhao C, McKeon JJ, McClemens E, Edgar M, Behrens F (2006) Computed radiographic measurement of limb-length discrepancy. Full-length standing anteroposterior radiograph compared with scanogram. J Bone Joint Surg Am 88:2243–2251. https://doi.org/10.2106/JBJS.E.01179
Gurney B (2002) Leg length discrepancy. Gait Posture 15:195–206
Pasha S, Aubin CE, Sangole AP, Labelle H, Parent S, Mac-Thiong JM (2014) Three-dimensional spinopelvic relative alignment in adolescent idiopathic scoliosis. Spine 39:564–570. https://doi.org/10.1097/BRS.0000000000000193
Winter RB, Pinto WC (1986) Pelvic obliquity. Its causes and its treatment. Spine 11:225–234
Levangie PK (1999) The association between static pelvic asymmetry and low back pain. Spine 24:1234–1242
Al-Eisa E, Egan D, Deluzio K, Wassersug R (2006) Effects of pelvic skeletal asymmetry on trunk movement: three-dimensional analysis in healthy individuals versus patients with mechanical low back pain. Spine 31:E71–79. https://doi.org/10.1097/01.brs.0000197665.93559.04
Havran M, Scholten JD, Breuer P, Lundberg J, Kochersberger G, Newman D, Weiner DK (2016) Deconstructing chronic low back pain in the older adult-step-by-step evidence and expert-based recommendations for evaluation and treatment: part XII: leg length discrepancy. Pain Med 17:2230–2237. https://doi.org/10.1093/pm/pnw270
Rannisto S, Okuloff A, Uitti J, Paananen M, Rannisto PH, Malmivaara A, Karppinen J (2015) Leg-length discrepancy is associated with low back pain among those who must stand while working. BMC Musculoskelet Disord 16:110. https://doi.org/10.1186/s12891-015-0571-9
Nault ML, Allard P, Hinse S, Le Blanc R, Caron O, Labelle H, Sadeghi H (2002) Relations between standing stability and body posture parameters in adolescent idiopathic scoliosis. Spine 27:1911–1917
Sahli S, Rebai H, Ghroubi S, Yahia A, Guermazi M, Elleuch MH (2013) The effects of backpack load and carrying method on the balance of adolescent idiopathic scoliosis subjects. Spine J 13:1835–1842. https://doi.org/10.1016/j.spinee.2013.06.023
Jung JY, Cha EJ, Kim KA, Won Y, Bok SK, Kim BO, Kim JJ (2015) Influence of pelvic asymmetry and idiopathic scoliosis in adolescents on postural balance during sitting. Biomed Mater Eng 26(Suppl 1):S601–610. https://doi.org/10.3233/BME-151351
Lumley MA, Cohen JL, Borszcz GS, Cano A, Radcliffe AM, Porter LS, Schubiner H, Keefe FJ (2011) Pain and emotion: a biopsychosocial review of recent research. J Clin Psychol 67:942–968. https://doi.org/10.1002/jclp.20816
Caes L, Vervoort T, Eccleston C, Goubert L (2012) Parents who catastrophize about their child's pain prioritize attempts to control pain. Pain 153:1695–1701. https://doi.org/10.1016/j.pain.2012.04.028
Caes L, Vervoort T, Eccleston C, Vandenhende M, Goubert L (2011) Parental catastrophizing about child's pain and its relationship with activity restriction: the mediating role of parental distress. Pain 152:212–222. https://doi.org/10.1016/j.pain.2010.10.037
Vardeh D, Mannion RJ, Woolf CJ (2016) Toward a mechanism-based approach to pain diagnosis. J Pain 17:T50–69. https://doi.org/10.1016/j.jpain.2016.03.001
Misterska E, Glowacki J, Okret A, Laurentowska M, Glowacki M (2017) Back and neck pain and function in females with adolescent idiopathic scoliosis: a follow-up at least 23 years after conservative treatment with a Milwaukee brace. PLoS ONE 12:e0189358. https://doi.org/10.1371/journal.pone.0189358
Smorgick Y, Mirovsky Y, Baker KC, Gelfer Y, Avisar E, Anekstein Y (2013) Predictors of back pain in adolescent idiopathic scoliosis surgical candidates. J Pediatr Orthop 33:289–292. https://doi.org/10.1097/BPO.0b013e31827d0b43
Joncas J, Labelle H, Poitras B, Duhaime M, Rivard CH, Le Blanc R (1996) Dorso-lumbal pain and idiopathic scoliosis in adolescence. Ann Chir 50:637–640
Deceuninck J, Bernard JC (2012) Quality of life and brace-treated idiopathic scoliosis: a cross-sectional study performed at the Centre des Massues on a population of 120 children and adolescents. Ann Phys Rehabil Med 55:93–102. https://doi.org/10.1016/j.rehab.2011.12.003
Holley AL, Wilson AC, Palermo TM (2017) Predictors of the transition from acute to persistent musculoskeletal pain in children and adolescents: a prospective study. Pain 158:794–801. https://doi.org/10.1097/j.pain.0000000000000817
Simons LE, Claar RL, Logan DL (2008) Chronic pain in adolescence: parental responses, adolescent coping, and their impact on adolescent's pain behaviors. J Pediatr Psychol 33:894–904. https://doi.org/10.1093/jpepsy/jsn029
Claar RL, Baber KF, Simons LE, Logan DE, Walker LS (2008) Pain coping profiles in adolescents with chronic pain. Pain 140:368–375. https://doi.org/10.1016/j.pain.2008.09.007
Al-Aubaidi Z, Lebel D, Oudjhane K, Zeller R (2013) Three-dimensional imaging of the spine using the EOS system: is it reliable? A comparative study using computed tomography imaging. J Pediatr Orthop B 22:409–412. https://doi.org/10.1097/BPB.0b013e328361ae5b
Gille O, Champain N, Benchikh-El-Fegoun A, Vital JM, Skalli W (2007) Reliability of 3D reconstruction of the spine of mild scoliotic patients. Spine 32:568–573. https://doi.org/10.1097/01.brs.0000256866.25747.b3
Ilharreborde B, Steffen JS, Nectoux E, Vital JM, Mazda K, Skalli W, Obeid I (2011) Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine 36:E1306–1313. https://doi.org/10.1097/BRS.0b013e3182293548
Glaser DA, Doan J, Newton PO (2012) Comparison of 3-dimensional spinal reconstruction accuracy: biplanar radiographs with EOS versus computed tomography. Spine 37:1391–1397. https://doi.org/10.1097/BRS.0b013e3182518a15
Quartana PJ, Campbell CM, Edwards RR (2009) Pain catastrophizing: a critical review. Expert Rev Neurother 9:745–758. https://doi.org/10.1586/ern.09.34
Acknowledgements
The study was financially supported by AOTK (CEF, JAO and MSG) and the Shriners Hospitals (CEF and JAO).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest related to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Teles, A.R., St-Georges, M., Abduljabbar, F. et al. Back pain in adolescents with idiopathic scoliosis: the contribution of morphological and psychological factors. Eur Spine J 29, 1959–1971 (2020). https://doi.org/10.1007/s00586-020-06489-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06489-2