Abstract
As the main component of the natural cornea, collagen (COL) has been widely applied to the construction of corneal repair materials. However, the applications of collagen are limited due to its poor mechanical properties. Cellulose nanocrystals (CNCs) possess excellent mechanical properties, optical transparency and good biocompatibility. Therefore, in this study, we attempted to introduce cellulose nanocrystals into collagen-based films to obtain corneal repair materials with a high strength. CNCs were incorporated at 1, 3, 5, 7 and 10 wt%. The physical properties of these composite films were characterized, and in vitro cell-based analyses were also performed. The COL/CNC films possessed better mechanic properties, and the introduction of CNCs did not affect the water content and light transmittance. The COL/CNC films demonstrated good biocompatibility toward rabbit corneal epithelial cells and keratocytes in vitro. Moreover, the collagen films with appropriate ration of CNCs effectively induced the migration of corneal epithelial cells and inhibited the myofibroblast differentiation of keratocytes. A collagen film with 7 wt% CNCs displayed the best combination of physical properties and biological performance in vitro among all the films. This study describes a nonchemical cross-linking method to enhance the mechanical properties of collagen for use in corneal repair materials and highlights potential application in corneal tissue engineering.









Similar content being viewed by others
References
DelMonte DW, Kim T. Anatomy and physiology of the cornea. J Cataract Refractive Surg. 2011;37:588–98.
Eghrari AO, Riazuddin SA, Gottsch JD. Overview of the cornea: structure, function, and development. Pro. Mol Biol Transl. Sci. 2015;134:7–23.
Mergler S, Pleyer U. The human corneal endothelium: new insights into electrophysiology and ion channels. Prog Retinal Eye Res. 2007;26:359–78.
Oliva MS, Schottman T, Gulati M. Turning the tide of corneal blindness. Indian J Ophthalmol. 2012;60:423–7.
Lamm V, Hara H, Mammen A, Dhaliwal D, Cooper DK. Corneal blindness and xenotransplantation. Xenotransplantation. 2014;21:99–114.
Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614–8.
Palchesko RN, Carrasquilla SD, Feinberg AW. Natural biomaterials for corneal tissue engineering, repair, and regeneration. Adv Healthcare Mater. 2018;7:1701434.
Chen Z, You J, Liu X, Cooper S, Hodge C, Sutton G, et al. Biomaterials for corneal bioengineering. Biomed Mater. 2018;13:032002.
Avadhanam VS, Liu CS. A brief review of Boston type-1 and osteo-odonto keratoprostheses. Br J Ophthalmol. 2015;99:878–87.
Li L, Lu C, Wang L, Chen M, White J, Hao X, et al. Gelatin-based photocurable hydrogels for corneal wound repair. ACS Appl Mater Interfaces. 2018;10:13283–92.
Sani ES, Kheirkhah A, Rana D, Sun Z, Foulsham W, Sheikhi A, et al. Sutureless repair of corneal injuries using naturally derived bioadhesive hydrogels. Sci Adc. 2019;5:eaav1281.
Aghaei-Ghareh-Bolagh B, Guan J, Wang YW, Martin AD, Dawson R, Mithieux SM, et al. Optically robust, highly permeable and elastic protein films that support dual cornea cell types. Biomaterials. 2019;188:50–62.
Liu Y, Gan L, Carlsson DJ, Fagerholm P, Lagali N, Watsky MA, et al. A simple, cross-linked collagen tissue substitute for corneal implantation. Investig Ophthalmol Visual Sci. 2006;47:1869–75.
Merrett K, Fagerholm P, McLaughlin CR, Dravida S, Lagali N, Shinozaki N, et al. Tissue-engineered recombinant human collagen-based corneal substitutes for implantation: performance of type I versus type III collagen. Investig Ophthalmol Visual Sci. 2008;49:3887–94.
Cui Z, Zeng Q, Liu S, Zhang Y, Zhu D, Guo Y, et al. Cell-laden and orthogonal-multilayer tissue-engineered corneal stroma induced by a mechanical collagen microenvironment and transplantation in a rabbit model. Acta Biomater. 2018;75:183–99.
Kishore V, Iyer R, Frandsen A, Nguyen T-U. In vitrocharacterization of electrochemically compacted collagen matrices for corneal applications. Biomed Mater. 2016;11:055008.
Tanaka Y, Baba K, Duncan TJ, Kubota A, Asahi T, Quantock AJ, et al. Transparent, tough collagen laminates prepared by oriented flow casting, multi-cyclic vitrification and chemical cross-linking. Biomaterials. 2011;32:3358–66.
Tanaka Y, Kubota A, Matsusaki M, Duncan T, Hatakeyama Y, Fukuyama K, et al. Anisotropic mechanical properties of collagen hydrogels induced by uniaxial-flow for ocular applications. J Biomater Sci Polym. Ed. 2012;22:1427–42.
Lee HJ, Fernandes-Cunha GM, Na KS, Hull SM, Myung D. Bio-orthogonally crosslinked, in situ forming corneal stromal tissue substitute. Adv Healthcare Mater. 2018;7:1800560.
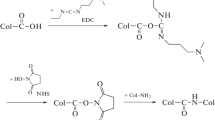
Ahn JI, Kuffova L, Merrett K, Mitra D, Forrester JV, Li F, et al. Crosslinked collagen hydrogels as corneal implants: effects of sterically bulky vs. non-bulky carbodiimides as crosslinkers. Acta Biomater. 2013;9:7796–805.
Choi S, Shin JH, Cheong Y, Jin KH, Park HK. Structural and biomechanical effects of photooxidative collagen cross-linking with photosensitizer riboflavin and 370 nm UVA light on human corneoscleral tissues. Microsc Microanal. 2013;19:1334–40.
Koulikovska M, Rafat M, Petrovski G, Veréb Z, Akhtar S, Fagerholm P, et al. Enhanced regeneration of corneal tissue via a bioengineered collagen construct implanted by a nondisruptive surgical technique. Tissue Eng Part A. 2015;21:1116–30.
Goodarzi H, Jadidi K, Pourmotabed S, Sharifi E, Aghamollaei H. Preparation and in vitro characterization of cross-linked collagen–gelatin hydrogel using EDC/NHS for corneal tissue engineering applications. Int J Biol Macromol. 2019;126:620–32.
Amruthwar SS, Puckett AD, Janorkar AV. Preparation and characterization of novel elastin-like polypeptide-collagen composites. J Biomed Mater Res Part A. 2013;101:2383–91.
Duan X, Sheardown H. Dendrimer crosslinked collagen as a corneal tissue engineering scaffold: mechanical properties and corneal epithelial cell interactions. Biomaterials. 2006;27:4608–17.
Liu D, Chen X, Yue Y, Chen M, Wu Q. Structure and rheology of nanocrystalline cellulose. Carbohydr Polym. 2011;84:316–22.
Mariano M, El Kissi N, Dufresne A. Cellulose nanocrystals and related nanocomposites: Review of some properties and challenges. J Polym Sci, Part B. 2014;52:791–806.
Trache D, Hussin MH, Haafiz MKM, Thakur VK. Recent progress in cellulose nanocrystals: sources and production. Nanoscale. 2017;9:1763–86.
Li W, Guo R, Lan Y, Zhang Y, Xue W, Zhang Y. Preparation and properties of cellulose nanocrystals reinforced collagen composite films. J Biomed Mater Res, Part A. 2014;102:1131–9.
Kashani Rahimi S, Aeinehvand R, Kim K, Otaigbe JU. Structure and biocompatibility of bioabsorbable nanocomposites of aliphatic-aromatic copolyester and cellulose nanocrystals. Biomacromolecules. 2017;18:2179–94.
Liu Y, Ren L, Long K, Wang L, Wang Y. Preparation and characterization of a novel tobramycin-containing antibacterial collagen film for corneal tissue engineering. Acta Biomater. 2014;10:289–99.
Favier V, Cavaille J, Canova G, Shrivastava S. Mechanical percolation in cellulose whisker nanocomposites. Polym Eng Sci. 1997;37:1732–9.
Pooyan P, Tannenbaum R, Garmestani H. Mechanical behavior of a cellulose-reinforced scaffold in vascular tissue engineering. J Mech Behav Biomed Mater. 2012;7:50–9.
Shin MK, Spinks GM, Shin SR, Kim SI, Kim SJ. Nanocomposite hydrogel with high toughness for bioactuators. Adv Mater. 2009;21:1712–5.
Lewis PN, White TL, Young RD, Bell JS, Winlove CP, Meek KM. Three-dimensional arrangement of elastic fibers in the human corneal stroma. Exp Eye Res. 2016;146:43–53.
von Burkersroda F, Schedl L, Göpferich A. Why degradable polymers undergo surface erosion or bulk erosion. Biomaterials. 2002;23:4221–31.
Liliensiek SJ, Campbell S, Nealey PF, Murphy CJ. The scale of substratum topographic features modulates proliferation of corneal epithelial cells and corneal fibroblasts. J Biomed Mater Res Part A. 2006;79:185–92.
Chi C, Trinkaus-Randall V. New insights in wound response and repair of epithelium. J Cell Physiol. 2013;228:925–9.
Crosson C, Klyce S, Beuerman R. Epithelial wound closure in the rabbit cornea. A biphasic process. Investig Ophthalmol Visual Sci. 1986;27:464–73.
Liu CY, Kao WW. Corneal Epithelial Wound Healing. Prog Mol Biol Transl Sci. 2015;134:61–71.
Lu L, Reinach PS, Kao WW-Y. Corneal epithelial wound healing. Exp Biol Med. 2001;226:653–64.
Hadjipanayi E, Mudera V, Brown RA. Close dependence of fibroblast proliferation on collagen scaffold matrix stiffness. J Tissue Eng Regener Med. 2009;3:77–84.
Wong JY, Leach JB, Brown XQ. Balance of chemistry, topography, and mechanics at the cell–biomaterial interface: Issues and challenges for assessing the role of substrate mechanics on cell response. Surf Sci. 2004;570:119–33.
Torricelli AAM, Santhanam A, Wu JH, Singh V, Wilson SE. The corneal fibrosis response to epithelial-stromal injury. Exp Eye Res. 2016;142:110–8.
Baldwin HC, Marshall J. Growth factors in corneal wound healing following refractive surgery: a review. Acta Ophthalmol Scand. 2002;80:238–47.
Nakamura K. Interaction between injured corneal epithelial cells and stromal cells. Cornea. 2003;22:S35–47.
Hinz B. Myofibroblasts. Exp Eye Res. 2016;142:56–70.
Myrna KE, Pot SA, Murphy CJ. Meet the corneal myofibroblast: the role of myofibroblast transformation in corneal wound healing and pathology. Vet Ophthalmol. 2009;12:25–7.
Xiong S, Gao H, Qin L, Jia Y, Gao M, Ren L. Microgrooved collagen-based corneal scaffold for promoting collective cell migration and antifibrosis. RSC Adv. 2019;9:29463–73.
Acknowledgements
This work was supported by the National Key Research and Development Program of China (grant number 2017YFC1105004), the National Natural Science Foundation of China (grant number 31971261, 51603074), the Guangdong Basic and Applied Basic Research Foundation (grant number 2020A1515010668), the Guangdong Province Key R & D Program Project (grant number 2020B1111150002), the Natural Science Foundation of Guangdong Province (grant number 2017A030313294), the Guangdong Scientific and Technological Project (grant numbers 2014B090907004, 201508020123, 2018A050506018), the Medical Scientific Research Foundation of Guangdong Province (grant number A2018169), the Frontier Research Program of Guangzhou Regenerative Medicine and Health Guangdong Laboratory (grant number 2018GZR110105008) and the Fundamental Research Funds for the Central Universities (grant number D2192170).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Qin, L., Gao, H., Xiong, S. et al. Preparation of collagen/cellulose nanocrystals composite films and their potential applications in corneal repair. J Mater Sci: Mater Med 31, 55 (2020). https://doi.org/10.1007/s10856-020-06386-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-020-06386-6