Abstract
Purpose
To investigate GAP scores in an asymptomatic cohort of adults, including older adults with age-expected changes in spinal alignment.
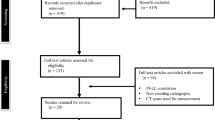
Methods
One hundred and twenty asymptomatic volunteers underwent full-body radiographic scans. Demographics and sagittal radiographic parameters (pelvic incidence, sacral slope, L1-S1 lordosis, L4-S1 lordosis, and global tilt) were measured and GAP scores calculated (www.gapcalculator.com). Mann–Whitney U test compared groups.
Results
Eighty-five individuals (65 female, average age 48 ± 16 years, BMI 27 ± 6 kg/cm2) were analyzed. The median GAP score was that of a proportioned spine (0, range 0–10). 20% were moderately disproportioned and 6% were severely disproportioned. The mean relative pelvic version, relative lumbar lordosis (RLL), lumbar distribution index (LDI), and relative spinopelvic alignment were all considered aligned, although the mean RLL and LDI scores were both greater than 1. When categorized by age (< 60 years, ≥ 60 years), the median GAP score of the younger group was 0 (normal), while the median GAP score of the older cohort was 1 (normal) and different from the younger group (p < 0.001).
Conclusion
Most patients in this asymptomatic, nonoperative cohort were normally proportioned. However, a large percentage of asymptomatic volunteers were moderately or severely disproportioned. Older patients had higher scores, indicating some disproportion. There was also a small number of severely sagittally misaligned and poorly proportioned, yet asymptomatic, volunteers. Further refinement of individualized targets is needed to determine the effect on mechanical complications and quality of life given the divergent recommendations of age-adjusted targets and GAP targets.


Similar content being viewed by others
References
Soroceanu A, Burton DC, Oren JH, Smith JS, Hostin R, Shaffrey CI, Akbarnia BA, Ames CP, Errico TJ, Bess S, Gupta MC, Deviren V, Schwab FJ, Lafage V, International Spine Study G (2016) Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine (Phila Pa 1976) 41(22):1718–1723. https://doi.org/10.1097/BRS.0000000000001636
Smith JS, Klineberg E, Lafage V, Shaffrey CI, Schwab F, Lafage R, Hostin R, Mundis GM Jr, Errico TJ, Kim HJ, Protopsaltis TS, Hamilton DK, Scheer JK, Soroceanu A, Kelly MP, Line B, Gupta M, Deviren V, Hart R, Burton DC, Bess S, Ames CP, International Spine Study G (2016) Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. J Neurosurg Spine 25(1):1–14. https://doi.org/10.3171/2015.11.SPINE151036
Yeramaneni S, Robinson C, Hostin R (2016) Impact of spine surgery complications on costs associated with management of adult spinal deformity. Curr Rev Musculoskelet Med 9(3):327–332. https://doi.org/10.1007/s12178-016-9352-9
Soroceanu A, Diebo BG, Burton D, Smith JS, Deviren V, Shaffrey C, Kim HJ, Mundis G, Ames C, Errico T, Bess S, Hostin R, Hart R, Schwab F, Lafage V, International Spine Study G (2015) Radiographical and Implant-Related Complications in Adult Spinal Deformity Surgery: Incidence, Patient Risk Factors, and Impact on Health-Related Quality of Life. Spine (Phila Pa 1976) 40(18):1414–1421. https://doi.org/10.1097/BRS.0000000000001020
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30(18):2024–2029
Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V, International Spine Study G (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 38(13):E803–812. https://doi.org/10.1097/BRS.0b013e318292b7b9
Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstuck F, Perez-Grueso FJS, Acaroglu E, Haddad S, Mannion AF, Pellise F, Alanay A, European Spine Study G (2017) Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99(19):1661–1672. https://doi.org/10.2106/JBJS.16.01594
Lafage R, Schwab F, Glassman S, Bess S, Harris B, Sheer J, Hart R, Line B, Henry J, Burton D, Kim H, Klineberg E, Ames C, Lafage V, International Spine Study G (2017) Age-adjusted alignment goals have the potential to reduce PJK. Spine (Phila Pa 1976) 42(17):1275–1282. https://doi.org/10.1097/BRS.0000000000002146
Iyer S, Lenke LG, Nemani VM, Albert TJ, Sides BA, Metz LN, Cunningham ME, Kim HJ (2016) Variations in sagittal alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976) 41(23):1826–1836. https://doi.org/10.1097/BRS.0000000000001642
Iyer S, Lenke LG, Nemani VM, Fu M, Shifflett GD, Albert TJ, Sides BA, Metz LN, Cunningham ME, Kim HJ (2016) Variations in occipitocervical and cervicothoracic alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976) 41(23):1837–1844. https://doi.org/10.1097/BRS.0000000000001644
Theologis AA, Iyer S, Lenke LG, Sides BA, Kim HJ, Kelly MP (2018) Cervical and cervicothoracic sagittal alignment according to roussouly's thoracolumbar subtypes. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0000000000002941
Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW (1995) An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976) 20(12):1351–1358
Lafage R, Schwab F, Challier V, Henry JK, Gum J, Smith J, Hostin R, Shaffrey C, Kim HJ, Ames C, Scheer J, Klineberg E, Bess S, Burton D, Lafage V, International Spine Study G (2016) Defining Spino-Pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976) 41(1):62–68. https://doi.org/10.1097/BRS.0000000000001171
Scheer JK, Lafage R, Schwab FJ, Liabaud B, Smith JS, Mundis GM, Hostin R, Shaffrey CI, Burton DC, Hart RA, Kim HJ, Bess S, Gupta M, Lafage V, Ames CP, International Spine Study G (2018) Under correction of sagittal deformities based on age-adjusted alignment thresholds leads to worse health-related quality of life whereas over correction provides no additional benefit. Spine (Phila Pa 1976) 43(6):388–393. https://doi.org/10.1097/BRS.0000000000002435
Bari TJ, Ohrt-Nissen S, Hansen LV, Dahl B, Gehrchen M (2019) Ability of the global alignment and proportion score to predict mechanical failure following adult spinal deformity surgery-validation in 149 patients with two-year follow-up. Spine Deform 7(2):331–337. https://doi.org/10.1016/j.jspd.2018.08.002
Jacobs E, van Royen BJ, van Kuijk SMJ, Merk JMR, Stadhouder A, van Rhijn LW, Willems PC (2019) Prediction of mechanical complications in adult spinal deformity surgery-the GAP score versus the Schwab classification. Spine J 19(5):781–788. https://doi.org/10.1016/j.spinee.2018.11.013
Kelly MP, Lurie JD, Yanik EL, Shaffrey CI, Baldus CR, Boachie-Adjei O, Buchowski JM, Carreon LY, Crawford CH 3rd, Edwards C 2nd, Errico TJ, Glassman SD, Gupta MC, Lenke LG, Lewis SJ, Kim HJ, Koski T, Parent S, Schwab FJ, Smith JS, Zebala LP, Bridwell KH (2019) Operative versus nonoperative treatment for adult symptomatic lumbar scoliosis. J Bone Joint Surg Am 101(4):338–352. https://doi.org/10.2106/JBJS.18.00483
Bassani T, Galbusera F, Luca A, Lovi A, Gallazzi E, Brayda-Bruno M (2019) Physiological variations in the sagittal spine alignment in an asymptomatic elderly population. Spine J 19(11):1840–1849. https://doi.org/10.1016/j.spinee.2019.07.016
Korovessis P, Stamatakis M, Baikousis A (1999) Segmental roentgenographic analysis of vertebral inclination on sagittal plane in asymptomatic versus chronic low back pain patients. J Spinal Disord 12(2):131–137
Stagnara P, De Mauroy JC, Dran G, Gonon GP, Costanzo G, Dimnet J, Pasquet A (1982) Reciprocal angulation of vertebral bodies in a sagittal plane: approach to references for the evaluation of kyphosis and lordosis. Spine (Phila Pa 1976) 7(4):335–342. https://doi.org/10.1097/00007632-198207000-00003
Zhou S, Xu F, Wang W, Zou D, Sun Z, Li W (2019) Age-based normal sagittal alignment in Chinese asymptomatic adults: establishment of the relationships between pelvic incidence and other parameters. Eur Spine J. https://doi.org/10.1007/s00586-019-06178-9
Funding
EOS-Imaging provided direct research support for patient honoraria and staff. No author received payments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Lenke reports being a consultant for Medtronic (money donated to charity); receiving royalties from Medtronic and Quality Medical Publishing; receiving reimbursement for airfare and hotels from Broadwater, the Seattle Science Foundation, Stryker Spine, the Spinal Research Foundation, AOSpine, and the Scoliosis Research Society; receiving grant support from the Scoliosis Research Society (money to his institution), EOS Imaging (money to his institution), and the Setting Scoliosis Straight Foundation (money to his institution); being an expert witness for Fox Rothschild, LLC, in a patent-infringement case; receiving philanthropic research funding from the Evans family; and receiving grant and fellowship support from AOSpine (money to his institution). Dr. Kim acts as a consultant to Zimmer Biomet, K2M/Styrker and receives royalty payments from Zimmer Biomet, K2M/Stryker. Dr. Kelly receives research support paid to his institution from the Setting Scoliosis Straight Foundation and the International Spine Study Group Foundation; honoraria from The Journal of Bone and Joint Surgery.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wegner, A.M., Iyer, S., Lenke, L.G. et al. Global alignment and proportion (GAP) scores in an asymptomatic, nonoperative cohort: a divergence of age-adjusted and pelvic incidence-based alignment targets. Eur Spine J 29, 2362–2367 (2020). https://doi.org/10.1007/s00586-020-06474-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06474-9