Abstract
Type 1 diabetes (T1D) is characterized by pancreatic beta cell dysfunction and insulin depletion. Over 40% of people with T1D manage their glucose through multiple injections of long-acting basal and short-acting bolus insulin, so-called multiple daily injections (MDI)1,2. Errors in dosing can lead to life-threatening hypoglycaemia events (<70 mg dl−1) and hyperglycaemia (>180 mg dl−1), increasing the risk of retinopathy, neuropathy, and nephropathy. Machine learning (artificial intelligence) approaches are being harnessed to incorporate decision support into many medical specialties. Here, we report an algorithm that provides weekly insulin dosage recommendations to adults with T1D using MDI therapy. We employ a unique virtual platform3 to generate over 50,000 glucose observations to train a k-nearest neighbours4 decision support system (KNN-DSS) to identify causes of hyperglycaemia or hypoglycaemia and determine necessary insulin adjustments from a set of 12 potential recommendations. The KNN-DSS algorithm achieves an overall agreement with board-certified endocrinologists of 67.9% when validated on real-world human data, and delivers safe recommendations, per endocrinologist review. A comparison of inter-physician-recommended adjustments to insulin pump therapy indicates full agreement of 41.2% among endocrinologists, which is consistent with previous measures of inter-physician agreement (41–45%)5. In silico3,6 benchmarking using a platform accepted by the United States Food and Drug Administration for evaluation of artificial pancreas technologies indicates substantial improvement in glycaemic outcomes after 12 weeks of KNN-DSS use. Our data indicate that the KNN-DSS allows for early identification of dangerous insulin regimens and may be used to improve glycaemic outcomes and prevent life-threatening complications in people with T1D.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data generated in silico during this study and the code used for analysis is available from the corresponding author on reasonable request. Access to human participant data was granted for the current study, and further human data usage or sharing is subject to restrictions and is not publicly available. Requests for restricted, de-identified data on human participants can be submitted to the corresponding authors at OHSU. Requests will be assessed on a case-by-case basis, and are subject to a formal Repository Sharing Agreement. Additional reported outcomes of human participants can be found at https://clinicaltrials.gov under registration number NCT03443713.
Code availability
The code used to generate in silico data for this study, the OHSU virtual patient population simulator code, is available at https://github.com/petejacobs/T1D_VPP. Access to the licensed software for the UVA–Padova virtual population was granted for the current study and it can be requested from the developers of this software directly at the University of Padova.
References
Paris, C. A. et al. Predictors of insulin regimens and impact on outcomes in youth with type 1 diabetes: the SEARCH for diabetes in youth study. J. Pediatr. 155, 183–189.e1 (2009).
Miller, K. M. et al. Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care 38, 971–978 (2015).
Resalat, N., El Youssef, J., Tyler, N., Castle, J. & Jacobs, P. G. A statistical virtual patient population for the glucoregulatory system in type 1 diabetes with integrated exercise model. PLoS One 14, e0217301 (2019).
Cover, T. & Hart, P. Nearest neighbor pattern classification. IEEE Trans. Inf. Theor. 13, 21–27 (2006).
Nimri, R. et al. Adjusting insulin doses in patients with type 1 diabetes who use insulin pump and continuous glucose monitoring: Variations among countries and physicians. Diabetes Obes. Metab. 20, 2458–2466 (2018).
Man, C. D. et al. The UVA/PADOVA type 1 diabetes simulator: new features. J. Diabetes Sci. Technol. 8, 26–34 (2014).
The Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular outcomes in type 1 diabetes: the DCCT/EDIC study 30-year follow-up. Diabetes Care 39, 686–693 (2016).
Schwartz, F. L., Guo, A., Marling, C. R. & Shubrook, J. H. Analysis of use of an automated bolus calculator reduces fear of hypoglycemia and improves confidence in dosage accuracy in type 1 diabetes mellitus patients treated with multiple daily insulin injections. J. Diabetes Sci. Technol. 6, 150–152 (2012).
Roze, S. et al. Cost-effectiveness of continuous subcutaneous insulin infusion versus multiple daily injections of insulin in type 1 diabetes: a systematic review. Diabet. Med. 32, 1415–1424 (2015).
McNally, K., Rohan, J., Pendley, J. S., Delamater, A. & Drotar, D. Executive functioning, treatment adherence, and glycemic control in children with type 1 diabetes. Diabetes Care 33, 1159–1162 (2010).
Sarbacker, G. B. & Urteaga, E. M. Adherence to insulin therapy. Diabetes Spectr. 29, 166–170 (2016).
Kirwan, M., Vandelanotte, C., Fenning, A. & Duncan, J. M. Diabetes self-management smartphone application for adults with type 1 diabetes: randomized controlled trial. J. Med. Internet Res. 15, e235 (2013).
Charpentier, G. et al. The Diabeo software enabling individualized insulin dose adjustments combined with telemedicine support improves HbA1c in poorly controlled type 1 diabetic patients: a 6-month, randomized, open-label, parallel-group, multicenter trial (TeleDiab 1 Study). Diabetes Care 34, 533–539 (2011).
Wu, Y. et al. Mobile app-based interventions to support diabetes self-management: a systematic review of randomized controlled trials to identify functions associated with glycemic efficacy. JMIR Mhealth Uhealth 5, e35 (2017).
Veazie, S et al. Rapid evidence review of mobile applications for self-management of diabetes. J. Gen. Intern. Med. 33, 1167–1176 (2018).
Beck, R. W. et al. Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections: the DIAMOND randomized clinical trial. JAMA 317, 371–378 (2017).
Steil, G. M. et al. Use of automated clinical decision support (CDS) to effect glycemic control in elderly patients with T1D. Diabetes 67, 921-P (2018).
Palerm, C. C., Zisser, H., Jovanovic, L. & Doyle, F. J. 3rd A run-to-run control strategy to adjust basal insulin infusion rates in type 1 diabetes. J. Process Control 18, 258–265 (2008).
Herrero, P., Bondia, J., Gimenez, M., Oliver, N. & Georgiou, P. Automatic adaptation of basal insulin using sensor-augmented pump therapy. J. Diabetes Sci. Technol. 12, 282–294 (2018).
Toffanin, C., Messori, M., Cobelli, C. & Magni, L. Automatic adaptation of basal therapy for type 1 diabetic patients: a run-to-run approach. Biomed. Signal Process. Control 31, 539–549 (2017).
Zisser, H., Palerm, C. C., Bevier, W. C., Doyle, F. J. 3rd & Jovanovic, L. Clinical update on optimal prandial insulin dosing using a refined run-to-run control algorithm. J. Diabetes Sci. Technol. 3, 487–491 (2009).
Herrero, P. et al. Advanced insulin bolus advisor based on run-to-run control and case-based reasoning. IEEE J. Biomed. Health Inform. 19, 1087–1096 (2015).
Perez-Gandia, C. et al. Decision support in diabetes care: the challenge of supporting patients in their daily living using a mobile glucose predictor. J. Diabetes Sci. Technol. 12, 243–250 (2018).
Breton, M. D. et al. Continuous glucose monitoring and insulin informed advisory system with automated titration and dosing of insulin reduces glucose variability in type 1 diabetes mellitus. Diabetes Technol. Ther. 20, 531–540 (2018).
Reddy, M. et al. Clinical safety and feasibility of the advanced bolus calculator for type 1 diabetes based on case-based reasoning: a 6-week nonrandomized single-arm pilot study. Diabetes Technol. Ther. 18, 487–493 (2016).
Resalat, N., El Youssef, J., Reddy, R., Castle, J. & Jacobs, P. G. Adaptive tuning of basal and bolus insulin to reduce postprandial hypoglycemia in a hybrid artificial pancreas. J. Process Control 80, 247–254 (2019).
Sørensen, T. J A Method of Establishing Groups of Equal Amplitude in Plant Sociology Based on Similarity of Species Content and its Application to Analyses of the Vegetation on Danish Commons (I kommission hos E. Munksgaard, 1948).
Davidson, M. B., Duran, P., Davidson, S. J. & Lee, M. Comparison of insulin dose adjustments by primary care physicians and endocrinologists. Clin. Diabetes 36, 39–43 (2018).
Bashan, E. & Hodish, I. Frequent insulin dosage adjustments based on glucose readings alone are sufficient for a safe and effective therapy. J. Diabetes Complicat. 26, 230–236 (2012).
Reddy, R. et al. The effect of exercise on sleep in adults with type 1 diabetes. Diabetes Obes. Metab. 20, 443–447 (2018).
Castle, J. R. et al. Randomized outpatient trial of single- and dual-hormone closed-loop systems that adapt to exercise using wearable sensors. Diabetes Care 41, 1471–1477 (2018).
Pettus, J. & Edelman, S. V. Recommendations for using real-time continuous glucose monitoring (rtCGM) data for insulin adjustments in type 1 diabetes. J. Diabetes Sci. Technol. 11, 138–147 (2017).
Whitney, A. W. A direct method of nonparametric measurement selection. IEEE Trans. Comput. 20, 1100–1103 (1971).
Scheiner, G. Practical CGM: Improving Patient Outcomes Through Continuous Glucose Monitoring (American Diabetes Association, 2015).
White, J. W., Rassweiler, A., Samhouri, J. F., Stier, A. C. & White, C. Ecologists should not use statistical significance tests to interpret simulation model results. Oikos 123, 385–388 (2014).
Acknowledgements
The guarantor of this research is Peter G. Jacobs who takes responsibility for the contents of the article. Correspondence and requests for materials can be addressed to Nichole S. Tyler and Peter G. Jacobs. The authors thank Gavin Young for his contributions to algorithm methodology. The authors disclose receipt of the following financial support for the research, authorship, and/or publication of the article: this work was supported by The Leona M. and Harry B. Helmsley Charitable Trust (grant 2018PG-T1D001), the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (grant 1 R01DK120367-01) and a Dexcom grant.
Author information
Authors and Affiliations
Contributions
N.S.T., C.M.M.-L., R.H.D. and P.G.J. contributed to the design of the published decision support engine algorithm. N.S.T. and C.M.M.-L. performed the additional evaluations of decision support engine performance. N.S.T., C.M.M.-L., R.H.D., W.W.H. and P.G.J. designed and discussed strategies for engine evaluation and outcomes metrics. L.M.W., J.R.C. and J.E.Y. served as physicians collecting human clinical trial data, contributed to the design of the quality control algorithm, and performed a safety evaluation of the algorithm. D.L.B., V.B.G. and F.H.G. collected and managed the human data used to evaluate the decision support engine.
Corresponding authors
Ethics declarations
Competing interests
The authors declare the following competing interests regarding research, authorship and publication of this article: J.R.C. and P.G.J. have financial interest in Pacific Diabetes Technologies Inc. (PDT), a company with potential commercial interests in the results and research of this technology. J.R.C. and P.G.J. are founders and shareholders in PDT and P.G.J. is a board member of PDT. Neither J.R.C. nor P.G.J. receive any financial compensation from PDT as consultants or otherwise, beyond shares in the company. J.R.C. and P.G.J. have received honoraria for consulting and research support from Dexcom. Although the methods on the algorithm were disclosed to the OHSU Technology Transfer Office, there has not yet been a patent filed on the algorithm and PDT does not have any rights to any of the technology described in the paper. N.S.T., C.M.M., R.H.D., L.M.W., D.L.B., V.B.G., F.H.G., W.W.H. and J.E.Y. declare no competing interests.
Additional information
Peer review information Primary Handling Editor: Christoph Schmitt.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Quality control algorithm to assess need for insulin titration.
Quality control algorithm to assess need for insulin titration. User data and glycemic outcomes are loaded and compared against metrics for percent time in hypoglycaemia, percent time in target range, and percent time in serious hypoglycaemia. If users meet all metrics, recommendations for insulin titration are not required.
Extended Data Fig. 2 Quality control algorithm to assess increasing basal insulin dosage.
Quality control algorithm to assess increasing basal insulin dosage. User features and glycemic outcomes are loaded by the algorithm and assessed for physician-informed metrics of nocturnal hypoglycaemia, near hypoglycaemia episodes, subject time in target range, subject adherence, and insulin formulation-dependent requirements.
Extended Data Fig. 3 Quality control algorithm to assess decreasing basal insulin dosage.
Quality control algorithm to assess decreasing basal insulin dosage. User features and glycemic outcomes are loaded by the algorithm and assessed for subject adherence, and insulin formulation-dependent requirements.
Extended Data Fig. 4 Quality control algorithm to assess increasing meal bolus insulin dosage.
Quality control algorithm to assess increasing meal bolus insulin dosage. User features and glycemic outcomes are loaded by the algorithm and assessed for physician-informed metrics of postprandial hypoglycaemia, subject adherence, and factors returned by the ALPHA algorithm.
Extended Data Fig. 5 Quality control algorithm to assess decreasing meal bolus insulin dosage.
Quality control algorithm to assess decreasing meal bolus insulin dosage. User features and glycemic outcomes are loaded by the algorithm and assessed for physician-informed metrics of postprandial severe hyperglycaemia, subject adherence, and factors returned by the ALPHA algorithm.
Extended Data Fig. 6 Quality control algorithm to assess increasing correction bolus insulin dosage.
Quality control algorithm to assess increasing correction bolus insulin dosage. User features and glycemic outcomes are loaded by the algorithm and assessed for physician-informed metrics of postprandial and correction-related hypoglycaemia, subject adherence, and factors returned by the ALPHA algorithm.
Extended Data Fig. 7 Quality control algorithm to assess decreasing correction bolus insulin dosage.
Quality control algorithm to assess decreasing correction bolus insulin dosage. User features and glycemic outcomes are loaded by the algorithm and assessed for physician-informed metrics of subject adherence, postprandial and correction-related hypoglycaemia, and factors returned by the ALPHA algorithm.
Extended Data Fig. 8 KNN-DSS engine performance in improving subject outcomes in an independent virtual patient population.
KNN-DSS engine performance in improving subject outcomes in an independent virtual patient population. Glycemic outcomes during a 52-week study of the FDA-approved UVA-Padova virtual patient simulator. Percent time in hypoglycaemia is indicated by the blue circular radius.
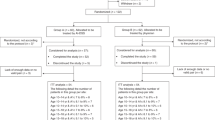
Extended Data Fig. 9 Outcomes of a human pilot study evaluating KNN-DSS augmented decision support.
Outcomes of a human pilot study evaluating KNN-DSS augmented decision support over 4 weeks where the first recommendation is given at the start of week 2. For panels a-f, boxplot limits indicate the first and third quartiles, centerline indicates the median, and whiskers mark the last non-outlier data-point within 1.5xIQR. For panels a-f, participant data collected during week 1 and the final week were compared using a two-tailed Wilcoxon signed-rank test, with significance level of 5%. a, Frequency of hypoglycaemia was nominally reduced on the final week compared with week 1 of the study (0.86 vs 0.64, P = 0.051, n = 16 independent subjects). b Serious hypoglycaemia was nominally reduced on the final week compared with week 1 of the study (0.34% vs. 0.19%, P = 0.56, n = 16 independent subjects). c Postprandial hypoglycaemia events were nominally reduced on the final week compared with week 1 (0.29 vs 0.14, P = 0.08, n = 16 independent subjects). d Frequency of overnight hypoglycaemia was significantly reduced on the final week compared to week 1 (0.50 to 0.29, P= 0.04, n = 16 independent subjects). e Serious hypoglycaemia overnight was significantly reduced on the final week compared to week 1 (0.48% to 0.11%, P = 0.03, n = 16 independent subjects). f Postprandial hypoglycaemia overnight was nominally reduced on the final week compared to week 1 (0.14 to 0. 07, P = 0.06, n = 16 independent subjects).
Supplementary information
Supplementary Information
Supplementary Tables 1–10
Rights and permissions
About this article
Cite this article
Tyler, N.S., Mosquera-Lopez, C.M., Wilson, L.M. et al. An artificial intelligence decision support system for the management of type 1 diabetes. Nat Metab 2, 612–619 (2020). https://doi.org/10.1038/s42255-020-0212-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s42255-020-0212-y
This article is cited by
-
Ethical concerns around privacy and data security in AI health monitoring for Parkinson’s disease: insights from patients, family members, and healthcare professionals
AI & SOCIETY (2024)
-
Recent advances in the precision control strategy of artificial pancreas
Medical & Biological Engineering & Computing (2024)
-
Concordance of randomised controlled trials for artificial intelligence interventions with the CONSORT-AI reporting guidelines
Nature Communications (2024)
-
Application of artificial intelligence to corelate food formulations to disease risk prediction: a comprehensive review
Journal of Food Science and Technology (2023)
-
Real-time artificial intelligence assisted insulin dosage titration system for glucose control in type 2 diabetic patients: a proof of concept study
Current Medicine (2023)