Abstract
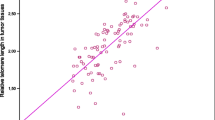
To investigate the diagnostic performance of relative telomere length (RTL) in cell-free DNA (cfDNA) for endometrioid endometrial cancer (EC). We measured RTL in cfDNA of 40 EC patients (65 ± 12 years) and 31 healthy controls (HC) (63 ± 13 years), excluding in both groups other oncologic and severe non-oncologic diseases to limit confounders. Circulating cfDNA was extracted from serum using the QIAamp DNA Blood Mini kit (Qiagen, Hilden, Germany). After the quantitative real-time polymerase chain reaction, telomere repeat copy number to single-gene copy number ratio was calculated. RTL in cfDNA was found to be significantly lower in EC patients than in HC (p < 0.0001). The diagnostic performance of cfDNA RTL was estimated with receiver operating characteristics (ROC) curve analysis, which showed a diagnostic accuracy for EC of 0.87 (95% CI: 0.79–0.95, p < 0.0001). The cutoff cfDNA RTL value of 2.505 (T/S copy ratio) reported a sensitivity of 80.0% (95% CI: 64.35–90.95) and a specificity of 80.65% (95% CI: 62.53–92.55). Significant differences of RTL among EC stages or grades (p = 0.85 and p = 0.89, respectively) were not observed. Our results suggest that cfDNA RTL analysis may be a diagnostic tool for EC detection since the early stage, whilst its diagnostic performance seems unsatisfactory for cancer progression, staging, and grading. However, further studies are needed to confirm these preliminary findings. In particular, future investigations should focus on high-risk patients (such as those with atypical endometrial hyperplasia) that may benefit from this tool, because TL shortening is not specific for EC and is influenced by other oncologic and non-oncologic diseases.




Similar content being viewed by others
References
Colombo N, Creutzberg C, Amant F, Bosse T, González-Martín A, Ledermann J, Marth C, Nout R, Querleu D, Mirza MR, Sessa C, ESMO-ESGO-ESTRO Endometrial Consensus Conference Working Group (2016) ESMO-ESGO-ESTRO consensus conference on endometrial cancer: diagnosis, treatment and follow-up. Int J Gynecol Cancer 26:2–30. https://doi.org/10.1097/IGC.0000000000000609
Yeramian A, Moreno-Bueno G, Dolcet X, Catasus L, Abal M, Colas E, Reventos J, Palacios J, Prat J, Matias-Guiu X (2013) Endometrial carcinoma: molecular alterations involved in tumor development and progression. Oncogene 32:403–413. https://doi.org/10.1038/onc.2012.76
Montagnana M, Lippi G, Ruzzenente O, Bresciani V, Danese E, Scevarolli S, Salvagno GL, Giudici S, Franchi M, Guidi GC (2009) The utility of serum human epididymis protein 4 (HE4) in patients with a pelvic mass. J Clin Lab Anal 23:331–335. https://doi.org/10.1002/jcla.20340
Montagnana M, Benati M, Danese E, Giudici S, Perfranceschi M, Ruzzenenete O, Salvagno GL, Bassi A, Gelati M, Paviati E, Guidi GC, Franchi M, Lippi G (2017) Aberrant MicroRNA expression in patients with endometrial cancer. Int J Gynecol Cancer 27:459–466. https://doi.org/10.1097/IGC.0000000000000913
Benati M, Montagnana M, Danese E, Paviati E, Giudici S, Franchi M, Lippi G (2017) Evaluation of mir-203 expression levels and DNA promoter methylation status in serum of patients with endometrial cancer. Clin Lab 63:1675–1681. https://doi.org/10.7754/Clin.Lab.2017.170421
Benati M, Montagnana M, Danese E, Paviati E, Giudici S, Ruzzenente O, Franchi M, Lippi G (2018) The clinical significance of DJ-1 and HE4 in patients with endometrial cancer. J Clin Lab Anal 32:e22223. https://doi.org/10.1002/jcla.22223
Casarin J, Bogani G, Serati M, Pinelli C, Laganà AS, Garzon S, Raspagliesi F, Ghezzi F (2019) Presence of glandular cells at the preoperative cervical cytology and local recurrence in endometrial cancer. Int J Gynecol Pathol. https://doi.org/10.1097/PGP.0000000000000642
Blackburn EH (1991) Structure and function of telomeres. Nature 350:569–573. https://doi.org/10.1038/350569a0
Moyzis RK, Buckingham JM, Cram LS, Dani M, Deaven LL, Jones MD, Meyne J, Ratliff RL, Wu JR (1988) A highly conserved repetitive DNA sequence, (TTAGGG) n, present at the telomeres of human chromosomes. Proc Natl Acad Sci U S A 85:6622–6626. https://doi.org/10.1073/pnas.85.18.6622
McClintock B (1941) The stability of broken ends of chromosomes in Zea Mays. Genetics 26:234–282
Blasco MA (2005) Telomeres and human disease: ageing, cancer and beyond. Nat Rev Genet 6:611–622. https://doi.org/10.1038/nrg1656
Lo AW, Sabatier L, Fouladi B, Pottier G, Ricoul M, Mumane JP (2002) DNA amplification by breakage/fusion/bridge cycles initiated by spontaneous telomere loss in a human cancer cell line. Neoplasia 4:531–538. https://doi.org/10.1038/sj.neo.7900267
Maser RS (2002) Connecting chromosomes, crisis, and cancer. Science 297:565–569. https://doi.org/10.1126/science.297.5581.565
Bunting SF, Nussenzweig A (2013) End-joining, translocations and cancer. Nat Rev Cancer 13:443–454. https://doi.org/10.1038/nrc3537
Counter CM, Hirte HW, Bacchetti S, Harley CB (1994) Telomerase activity in human ovarian carcinoma. Proc Natl Acad Sci U S A 91:2900–2904. https://doi.org/10.1073/pnas.91.8.2900
Hastie ND, Dempster M, Dunlop MG, Thompson AM, Green DK, Allshire RC (1990) Telomere reduction in human colorectal carcinoma and with ageing. Nature 346:866–868. https://doi.org/10.1038/346866a0
Sieglová Z, Žilovcová S, Čermák J, Řı́hová H, Březinová D, Dvořáková R, Marková M, Maaloufová J, Sajdová J, Březinová J, Zemanová Z, Michalová K (2004) Dynamics of telomere erosion and its association with genome instability in myelodysplastic syndromes (MDS) and acute myelogenous leukemia arising from MDS: a marker of disease prognosis? Leuk Res 28:1013–1021. https://doi.org/10.1016/j.leukres.2003.11.020
McGrath M, Wong JY, Michaud D, Hunter DJ, De Vivo I (2007) Telomere length, cigarette smoking, and bladder cancer risk in men and women. Cancer Epidemiol Biomark Prev 16:815–819. https://doi.org/10.1158/1055-9965.EPI-06-0961
Shao L, Wood CG, Zhang D, Tannir NM, Matin S, Dinney CP, Wu X (2007) Telomere dysfunction in peripheral lymphocytes as a potential predisposition factor for renal cancer. J Urol 178:1492–1496. https://doi.org/10.1016/j.juro.2007.05.112
Wu X, Amos CI, Zhu Y, Zhao H, Grossman BH, Shay JW, Luo S, Hong WK, Spitz MR (2003) Telomere dysfunction: a potential cancer predisposition factor. J Natl Cancer Inst 95:1211–1218. https://doi.org/10.1093/jnci/djg011
Jang JS, Choi YY, Lee WK, Choi JE, Cha SI, Kim YJ, Kim CH, Kam S, Jung TH, Park JY (2008) Telomere length and the risk of lung cancer. Cancer Sci 99:1385–1389. https://doi.org/10.1111/j.1349-7006.2008.00831.x
Willeit P, Willeit J, Mayr A, Weger S, Oberhollenzer F, Brandstätter A, Kronenberg F, Kiechl S (2010) Telomere length and risk of incident cancer and cancer mortality. JAMA 304:69–75. https://doi.org/10.1001/jama.2010.897
Weischer M, Nordestgaard BG, Cawthon RM, Freiberg JJ, Tybjærg-Hansen A, Bojesen SE (2013) Short telomere length, cancer survival, and cancer risk in 47102 individuals. J Natl Cancer Inst 105:459–468. https://doi.org/10.1093/jnci/djt016
Rode L, Nordestgaard BG, Bojesen SE (2015) Peripheral blood leukocyte telomere length and mortality among 64 637 individuals from the general population. J Natl Cancer Inst 107:1–8. https://doi.org/10.1093/jnci/djv074
Wan S, Hann HW, Myers RE, Fu X, Hann RS, Kim SH, Tang H, Xing J, Yang H (2012) Telomere length in circulating serum DNA as a novel non-invasive biomarker for cirrhosis: a nested case-control analysis. Liver Int 32:1233–1241. https://doi.org/10.1111/j.1478-3231.2012.02801.x
Wu X, Tanaka H (2015) Aberrant reduction of telomere repetitive sequences in plasma cell-free DNA for early breast cancer detection. Oncotarget 6:29795–29807. https://doi.org/10.18632/oncotarget.5083
Wan S, Hann HW, Ye Z, Hann RS, Lai Y, Wang C, Li L, Myers RE, Li B, Xing J, Yang H (2017) Prospective and longitudinal evaluations of telomere length of circulating DNA as a risk predictor of hepatocellular carcinoma in HBV patients. Carcinogenesis 38:439–446. https://doi.org/10.1093/carcin/bgx021
Franchi M, Garzon S, Zorzato PC, Laganà AS, Casarin J, Locantore L, Raffaelli R, Ghezzi F (2019) PET-CT scan in the preoperative workup of early stage intermediate- and high-risk endometrial cancer. Minim Invasive Ther Allied Technol. https://doi.org/10.1080/13645706.2019.1624576
Creasman W (2009) Revised FIGO staging for carcinoma of the endometrium. Int J Gynecol Obstet 105:109–109. https://doi.org/10.1016/j.ijgo.2009.02.010
Cawthon RM (2002) Telomere measurement by quantitative PCR. Nucleic Acids Res 30:e47–e51
Montagnana M, Lippi G (2017) Cancer diagnostics: current concepts and future perspectives. Ann Transl Med 5:268–271. https://doi.org/10.21037/atm.2017.06.20
Cerne D, Bajalo JL (2014) Cell-free nucleic acids as a non-invasive route for investigating atherosclerosis. Curr Pharm Des 20:5004–5009. https://doi.org/10.2174/1381612819666131206110317
Siravegna G, Marsoni S, Siena S, Bardelli A (2017) Integrating liquid biopsies into the management of cancer. Nat Rev Clin Oncol 14:531–548. https://doi.org/10.1038/nrclinonc.2017.14
Swarup V, Rajeswari MR (2007) Circulating (cell-free) nucleic acids - a promising, non-invasive tool for early detection of several human diseases. FEBS Lett 581:795–799. https://doi.org/10.1016/j.febslet.2007.01.051
Danese E, Montagnana M, Fava C, Guidi G (2014) Circulating nucleic acids and hemostasis: biological basis behind their relationship and technical issues in assessment. Semin Thromb Hemost 40:766–773 https://doi.org/10.1055/s-0034-1387923
Schwarzenbach H, Müller V, Stahmann N, Pantel K (2004) Detection and characterization of circulating microsatellite-DNA in blood of patients with breast cancer. Ann N Y Acad Sci 1022:25–32. https://doi.org/10.1196/annals.1318.005
Schwarzenbach H, Eichelser C, Kropidlowski J, Janni W, Rack B, Pantel K (2012) Loss of heterozygosity at tumor suppressor genes detectable on fractionated circulating cell-free tumor DNA as indicator of breast cancer progression. Clin Cancer Res 18:5719–5730. https://doi.org/10.1158/1078-0432.CCR-12-0142
Phallen J, Sausen M, Adleff V, Leal A, Hruban C, White J, Anagnostou V, Fiksel J, Cristiano S, Papp E, Speir S, Reinert T, Orntoft MW, Woodward BD, Murphy D, Parpart-Li S, Riley D, Nesselbush M, Sengamalay N, Georgiadis A, Li QK, Madsen MR, Mortensen FV, Huiskens J, Punt C, van Grieken N, Fijneman R, Meijer G, Husain H, Scharpf RB, Diaz Jr LA, Jones S, Angiuoli S, Ørntoft T, Nielsen HJ, Andersen CL, Velculescu VE (2017) Direct detection of early-stage cancers using circulating tumor DNA. Sci Transl med 9:eaan2415. https://doi.org/10.1126/scitranslmed.aan2415
Medford AJ, Gillani RN, Park BH (2018) Detection of cancer DNA in early stage and metastatic breast cancer patients. Methods Mol Biol 1768:209–227. https://doi.org/10.1007/978-1-4939-7778-9_13
Schwarzenbach H, Hoon DS, Pantel K (2011) Cell-free nucleic acids as biomarkers in cancer patients. Nat Rev Cancer 11:426–437. https://doi.org/10.1038/nrc3066
Jahr S, Hentze H, Englisch S, Hardt D, Fackelmayer FO, Hesch RD, Knippers R (2001) DNA fragments in the blood plasma of cancer patients: Quantitations and evidence for their origin from apoptotic and necrotic cells. Cancer Res 61:1659–1665
Heitzer E, Ulz P, Geigl JB (2015) Circulating tumor DNA as a liquid biopsy for cancer. Clin Chem 61:112–123. https://doi.org/10.1373/clinchem.2014.222679
Perakis S, Auer M, Belic J, Heitzer E (2017) Advances in circulating tumor DNA analysis. Adv Clin Chem 80:73–153. https://doi.org/10.1016/bs.acc.2016.11.005
Ulz P, Heitzer E, Geigl JB, Speicher MR (2017) Patient monitoring through liquid biopsies using circulating tumor DNA. Int J Cancer 141:887–896. https://doi.org/10.1002/ijc.30759
Marzese DM, Hirose H, Hoon DS (2013) Diagnostic and prognostic value of circulating tumor-related DNA in cancer patients. Expert Rev Mol Diagn 13:827–844. https://doi.org/10.1586/14737159.2013.845088
Chan KC, Jiang P, Zheng YW, Liao GJ, Sun H, Wong J, Siu SS, Chan WC, Chan SL, Chan AT, Lai PB, Chiu RW, Lo YM (2013) Cancer genome scanning in plasma: detection of tumor-associated copy number aberrations, single-nucleotide variants, and Tumoral heterogeneity by massively parallel sequencing. Clin Chem 59:211–224. https://doi.org/10.1373/clinchem.2012.196014
The Cancer Genome Atlas Research Network (2013) Integrated genomic characterization of endometrial carcinoma. Nature 497:67–73 https://doi.org/10.1038/nature12113
MacKay HJ, Levine DA, Bae-Jump VL, Bell DW, McAlpine JN, Santin A, Fleming GF, Mutch DG, Nephew KP, Wentzensen N, Goodfellow PJ, Dorigo O, Nijman HW, Broaddus R, Kohn EC (2017) Moving forward with actionable therapeutic targets and opportunities in endometrial cancer: NCI clinical trials planning meeting report on identifying key genes and molecular pathways for targeted endometrial cancer trials. Oncotarget 8:84579–84594 https://doi.org/10.18632/oncotarget.19961
Martin-Ruiz CM, Baird D, Roger L, Boukamp P, Krunic D, Cawthon R, Dokter MM, van der Harst P, Bekaert S, de Meyer T, Roos G, Svenson U, Codd V, Samani NJ, McGlynn L, Shiels PG, Pooley KA, Dunning AM, Cooper R, Wong A, Kingston A, von Zglinicki T (2015) Reproducibility of telomere length assessment: an international collaborative study. Int J Epidemiol 44:1673–1683. https://doi.org/10.1093/ije/dyu191
Cicchillitti L, Corrado G, De Angeli M, Mancini E, Baiocco E, Patrizi L, Zampa A, Merola R, Martayan A, Conti L, Piaggio G, Vizza E (2017) Circulating cell-free DNA content as blood based biomarker in endometrial cancer. Oncotarget 8:115230–115243. https://doi.org/10.18632/oncotarget.23247
Vizza E, Corrado G, De Angeli M, Carosi M, Mancini E, Baiocco E, Chiofalo B, Patrizi L, Zampa A, Piaggio G, Cicchillitti L (2018) Serum DNA integrity index as a potential molecular biomarker in endometrial cancer. J Exp Clin Cancer Res 37:16–24. https://doi.org/10.1186/s13046-018-0688-4
Harley CB (1991) Telomere loss: mitotic clock or genetic time bomb? Mutat Res 256:271–282. https://doi.org/10.1016/0921-8734(91)90018-7
Rizvi S, Raza ST, Mahdi F (2014) Telomere length variations in aging and age-related diseases. Curr Aging Sci 7:161–167 https://doi.org/10.2174/1874609808666150122153151
Goya RG, Cónsole GM, Spinelli OM, Carino MH, Riccillo F, Corrons FJ (2003) Glucocorticoid-induced apoptosis in lymphoid organs is associated with a delayed increase in circulating deoxyribonucleic acid. Apoptosis 8:171–177. https://doi.org/10.1023/A:1022922726418
Pérez LM, Amaral MA, Mundstock E, Barbé-Tuana FM, Guma FTCR, Jones MH, Machado DC, Sarria EE, Marques e Marques M, Preto LT, Epifanio M, Meinem Garbin JG, Mattiello R (2017) Effects of diet on telomere length: systematic review and meta-analysis. Public Health Genomics 20:286–292. https://doi.org/10.1159/000486586
Cherepanova AV, Tamkovich SN, Bryzgunova OE, Vlassov VV, Laktionov PP (2008) Deoxyribonuclease activity and circulating DNA concentration in blood plasma of patients with prostate tumors. Ann N Y Acad Sci 1137:218–221. https://doi.org/10.1196/annals.1448.016
Astuti Y, Wardhana A, Watkins J, Wulaningsih W (2017) Cigarette smoking and telomere length: a systematic review of 84 studies and meta-analysis. Environ Res 158:480–489. https://doi.org/10.1016/j.envres.2017.06.038
Haghiac M, Vora NL, Basu S, Johnson KL, Presley L, Bianchi DW, de Mouzon SH (2012) Increased death of adipose cells, a path to release cell free DNA into systemic circulation of obese women. Obesity (Silver Spring) Md 20:2213–2219. https://doi.org/10.1038/oby.2012.138
Needham BL, Adler N, Gregorich S, Rehkopf D, Lin J, Blackburn EH, Epel ES (2013) socioeconomic status, health behavior, and leukocyte telomere length in the National Health and nutrition examination survey, 1999–2002. Soc Sci Med 85:1–8. https://doi.org/10.1016/j.socscimed.2013.02.023
Lu W, Zhang Y, Liu D, Songyang Z, Wan M (2013) Telomeres-structure, function, and regulation. Exp Cell Res 319:133–141 https://doi.org/10.1016/j.yexcr.2012.09.005
Haycock PC, Heydon EE, Kaptoge S, Butterworth AS, Thompson A, Willeit P (2014) Leucocyte telomere length and risk of cardiovascular disease: systematic review and meta-analysis. BMJ 349:g4227. https://doi.org/10.1136/bmj.g4227
Pavanello S, Angelici L, Hoxha M, Cantone L, Campisi M, Tirelli AS, Vigna L, Pesatori AC, Bollati V (2018) Sterol 27-hydroxylase polymorphism significantly associates with shorter telomere, higher cardiovascular and Type-2 diabetes risk in obese subjects. Front Endocrinol 9:309. https://doi.org/10.3389/fendo.2018.00309
Russo P, Prinzi G, Proietti S, Lamonaca P, Frustaci A, Boccia S, Amore R, Lorenzi M, onder G, Marzetti E, Valdiglesias V, Guadagni F, Valente MG, Cascio GL, Fraietta S, Ducci G, Bonassi S (2018) Shorter telomere length in schizophrenia: evidence from a real-world population and meta-analysis of most recent literature. Schizophr Res 202:37–45. https://doi.org/10.1016/j.schres.2018.07.015
Needham BL, Mezuk B, Bareis N, Lin J, Blackburn EH, Epel ES (2015) Depression, anxiety and telomere length in young adults: evidence from the National Health and nutrition examination survey. Mol Psychiatry 20:520–528. https://doi.org/10.1038/mp.2014.89
Yaffe K, Lindquist K, Kluse M, Cawthon R, Harris T, Hsueh WC, Simonsick EM, Kuller L, Li R, Ayonayon HN, Rubin SM, Cummings SR (2011) Telomere length and cognitive function in community-dwelling elders: findings from the health ABC study. Neurobiol Aging 32:2055–2060. https://doi.org/10.1016/j.neurobiolaging.2009.12.006
Sun B, Wang Y, Kota K, Shi Y, Motlak S, Makambi K, Loffredo CA, Shields PG, Yang Q, Harris CC, Zheng YL (2015) Telomere length variation: a potential new telomere biomarker for lung cancer risk. Lung Cancer 88:297–303. https://doi.org/10.1016/j.lungcan.2015.03.011
Latifovic L, Peacock SD, Massey TE, King WD (2016) The influence of alcohol consumption, cigarette smoking, and physical activity on leukocyte telomere length. Cancer Epidemiol Biomarkers Prev 25:374–380. https://doi.org/10.1158/1055-9965.EPI-14-1364
Shammas MA (2011) Telomeres, lifestyle, cancer, and aging. Curr Opin Clin Nutr Metab Care 14:28–34. https://doi.org/10.1097/MCO.0b013e32834121b1
Author information
Authors and Affiliations
Contributions
G Lippi, M Franchi, F Ghezzi, M Benati and M Montagnana: study conceptualization, and protocol planning. M Benati, E Danese, M Mazzon, E Paviati and M Montagnana: laboratory analysis, data extraction, and statistical analysis. S Garzon, AS Laganà, J Casarin, S Giudici and R Raffaelli: clinical evaluation, follow-ups, data collection, and statistical analysis. G Lippi, F Ghezzi, M Franchi and M Montagnana: project administration, methodology validation, and supervision. S Garzon, AS Laganà, M Benati and M Montagnana: Manuscript writing/editing. G Lippi, F Ghezzi, M Franchi: Manuscript revision and final approval. All the authors conform the International Committee of Medical Journal Editors (ICMJE) criteria for authorship, contributed to the intellectual content of the study and gave approval for the final version of the article.
Corresponding author
Ethics declarations
Funding
None.
Conflict of Interest
The authors have no proprietary, financial, professional or other personal interest of any nature in any product, service or company. The authors alone are responsible for the content and writing of the paper.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Benati, M., Montagnana, M., Danese, E. et al. Aberrant Telomere Length in Circulating Cell-Free DNA as Possible Blood Biomarker with High Diagnostic Performance in Endometrial Cancer. Pathol. Oncol. Res. 26, 2281–2289 (2020). https://doi.org/10.1007/s12253-020-00819-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-020-00819-x