Abstract
Purpose of Review
In amyotrophic lateral sclerosis (ALS), sleep disruption is frequently present and substantially adds to disease burden. This review aims to summarize current knowledge on causes, pathophysiology, and treatment of sleep disturbances in ALS.
Recent Findings
Motor neuron degeneration and muscle weakness may lead to muscle cramps, pain, spasticity, immobilization, restless legs, sleep-disordered breathing, and difficulties to clear secretions. Furthermore, existential fears and depression may promote insomnia. Sleep-disordered breathing, and nocturnal hypoventilation in particular, requires ventilatory support which meaningfully prolongs survival and improves health-related quality of life albeit respiratory failure is inevitable. Early indication for non-invasive ventilation can be achieved by inclusion of capnometry in diagnostic sleep studies.
Summary
Sleep disruption is extremely common in ALS and may arise from different etiologies. The absence of causative therapeutic options for ALS underlines the importance of symptomatic and palliative treatment strategies that acknowledge sleep-related complaints.
Similar content being viewed by others
Introduction
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disorder characterized by progressive loss of upper and lower motor neurons. Consecutively, both spasticity and hyperreflexia may coexist with fasciculations and muscle atrophy, the latter resulting in skeletal muscle weakness virtually affecting all muscle groups. In bulbar-onset ALS, dysarthria and dysphagia usually predominate throughout the disease course. Spinal-onset subtypes of ALS arise from progressive loss of anterior horn cells which supply trunk and limb muscles [1, 2••]. Prevalence of ALS ranges from 5 to 8 per 100,000, and disease onset peaks between 50 and 70 years of age [3,4,5,6]. Lifetime risk for ALS has been reported to be 1:400 for women and 1:300 for men [7, 8].
Much is known about the molecular pathology of ALS and the genetic background of familial ALS subtypes [9] but no causative therapies have been developed to date. Only two compounds have been approved, including riluzole [10,11,12] and edavarone [13, 14], which both show disease-modifying effects but do not stop disease progression. Thus, muscle weakness is still inevitable and eventually leads to tetraplegia, dysarthria, swallowing dysfunction, and chronic hypercapnic respiratory failure [9, 15••]. Median survival has been reported to be 2.5–3.5 years after symptom onset and 1.5–2.5 years following diagnosis [16,17,18]. Chronic respiratory failure and its sequelae limit life span most and are the major cause of premature death in patients with ALS [19, 20]. ALS severely impacts activities of daily life and health-related quality of life for both patients and caregivers [21,22,23,24]. Since causative therapies are unavailable, symptom control is the hallmark of treatment, and a systematic approach to distinct disease aspects is recommended [15••].
Reduction of sleep quality substantially contributes to physical and mental health in patients with ALS [25,26,27,28,29,30]. Subsequently, sleep disturbances further increase the individual burden of disease. This review article aims to systematically outline sleep characteristics, sleep-related symptoms, and causes of sleep disruption in patients with ALS. Furthermore, it will focus not only on respiratory muscle weakness leading to sleep-related hypoventilation and chronic hypercapnic respiratory failure, but will also discuss “non-fatal” conditions which may also disrupt sleep and considerably impair health-related quality of life.
Motor Symptoms of ALS and Sleep
Virtually, all motor symptoms of ALS may directly affect sleep quality, including fasciculations, muscle cramps, immobilization, and even restless legs syndrome (RLS). Furthermore, impaired swallowing function, if present, puts patients at risk of sialorrhea, recurrent choking, and aspiration of saliva.
Muscle fasciculations have been reported to cause sleep disturbances in some patients with ALS [31]. In addition, recurrent muscle cramps may occur, mainly affecting lower limb muscles and often exacerbating during the night. The International Classification of Sleep Disorders (ICSD-3 [32]) refers to nocturnal leg muscle cramps which are often painful, or inconvenient at least, and have been reported in patients with spinal-onset ALS, in particular [28, 33]. Electrophysiologically, muscle cramps reflect spontaneous discharges of motor units at a much higher frequency (> 300 Hz) than with voluntary contraction [34]. Active stretching may help ending these discharges but may be hampered in patients in whom significant limb weakness is present.
Symptomatic treatment of leg muscle cramps includes sufficient fluid intake, correction of electrolyte imbalances and, if acceptable, cessation of any causative medications. Mexiletine 150 mg twice daily has recently been reported to alleviate ALS-related muscle cramps in a randomized controlled trial [35]. Baclofen and other compounds did not show significant effects on muscle cramps in patients with ALS [36]. Quinidine (200–300 mg once to twice daily) has been evaluated in numerous other neurological conditions, showing reduction of both cramp frequency and intensity [37] but long-term use may be associated with severe thrombocytopenia, cinchonism, and myocardial toxicity [38].
As motor function gets worse, patients may have difficulties to change position in bed. Systematic studies on this issue are lacking, but its potential to severely impair sleep quality is obvious [29]. Furthermore, immobilization renders patients more dependent on caregivers whose intervention is frequently needed for both pain relief and prevention of skin lesions [39, 40].
Diagnostic criteria for RLS include an urge to move the legs (with unpleasant or painful sensations in the lower limbs), symptom onset and exacerbation only during rest or inactivity, circadian occurrence and enhancement of symptoms in the evening or during the night, and symptom relief during voluntary movement such as walking or stretching [32]. Symptom burden may vary inter-individually but profound sleep disturbances are common [41]. Prevalence of RLS in patients with ALS has been investigated in only few studies, all of them showing that RLS is significantly more frequent in ALS patients than in the general population [42,43,44]. Immobilization itself may put ALS patients at a greater risk to experience RLS which is reflected by the observation that RLS severity seems to be associated with overall neurological handicap in affected patients [42]. Mild sensory neuropathy, or even small fiber neuropathy, which have both been described in ALS may also contribute to RLS in this condition [45,46,47].
Symptoms of RLS in patients with ALS should be actively asked for, and pharmacological treatment strategies should follow standard recommendations regarding iron supplementation (if iron deficiency is present according to serum ferritin levels) or the use of dopaminergic agents, α2δ ligands, or opioids [48].
Periodic limb movements in sleep (PLM) have only rarely been evaluated in patients with ALS. Previous reports on PLM prevalence and event counts are inconclusive [49, 50], and it is still unclear whether PLM impact objective sleep in ALS. Own unpublished data suggest that the PLM index is increased in a large subset of patients but does not translate into associated arousals from sleep [51•]. A recent study postulated PLM disorder to be present in almost one-third of ALS patients but ICSD-3 diagnostic criteria were possibly not fully met, and association with sleep arousals was not reported [52]. Pathophysiologically, it may be hypothesized that in ALS, PLM reflect spinal cord disinhibition due to degeneration of descending central pathways [53].
Nocturnal Pain in ALS
Pain and sleep quality are closely related: pain disrupts sleep and impaired sleep is known to worsen pain [54, 55]. Nocturnal pain in patients with ALS may directly result from immobilization and inability to change position in bed. Furthermore, intermittent muscle cramps or spasticity may induce pain, and muscle atrophy may enhance pressure load to bones and joints. A subset of patients with ALS may also experience neuropathic pain which is often not clearly localized [56, 57•] and may be attributable to small fiber neuropathy which has been described in up to 75% [45]. Finally, few patients report a third type of pain which is diffuse, non-neuropathic, independent of clear triggers, and possibly related to central sensitization of nociceptive pathways [58, 59]. Nocturnal pain in patients with ALS has not been specifically investigated in clinical studies [60]. Treatment strategies in patients with ALS usually follow clinical considerations rather than scientific evidence. Clearly nociceptive pain may require adequate preventive measures and non-steroidal anti-inflammatory drugs. Opioids may be added for otherwise refractory pain or if dyspnea is also present. Cannabis compounds may also be prescribed, having also sedating, anxiolytic, and appetite-enhancing effects. For alleviation of neuropathic pain α2δ ligands or antidepressants should be considered, and spasticity may require central muscle relaxants. To conclude, patients with ALS frequently report pain of different origin, potentially disrupting sleep. Since chronic pain co-determines subjective quality of life and suicidality especially in later stages of ALS, it should be considered a major target of symptomatic therapy [61].
Sleep-Related Breathing Disorders
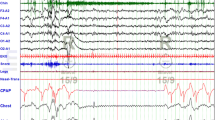
In patients with ALS, sleep-related breathing disorders mainly comprise nocturnal hypoventilation (NH) and obstructive sleep apnea (OSA). Central sleep apnea has only rarely been reported [62, 63]. Prevalence of OSA is particularly increased in male patients and, interestingly, in patients with spinal (or non-bulbar) onset of symptoms [51, 63]. In bulbar-onset ALS, OSA might be less likely to occur because atrophy of the tongue prevents pharyngeal collapse. The presence of OSA prior to initiation of ventilatory support has been related to shorter survival but often coincides with respiratory muscle weakness which mainly determines further disease progression [51•, 64, 65]. Sleep-related hypoventilation mainly results from phrenic nerve degeneration and diaphragm weakness leading to carbon dioxide accumulation during rapid eye movement (REM) sleep first [66]. With disease progression, hypercapnia spreads to non-REM sleep stages, and finally, daytime hypercapnia defines chronic hypercapnic respiratory failure. Associated symptoms include sleep disruption, daytime sleepiness, morning headache, and dyspnea in various situations, i.e., during sleep, when supine, on exertion, or at rest. In order to prevent orthopnea patients with advanced diaphragm weakness may adopt a sitting position in bed. Several studies have shown that sleep-disordered breathing impairs both continuity and composition of sleep in ALS patients. Apneas, hypopneas, and impaired gas exchange are associated with reduced sleep efficiency, frequent sleep stage changes, arousals from sleep, and reduction of N3 or REM sleep [51•, 62, 67,68,69,70,71]. For detection of nocturnal hypoventilation, pulse oximetry has widely been used but transcutaneous capnometry has proven to be superior since peripheral oxygen saturation may be normal in one-third of patients with sleep-related hypercapnia [51•, 72]. Thus, transcutaneous capnometry is indispensable for evaluation of sleep-related breathing in ALS in order to warrant that diagnosis of nocturnal hypoventilation and initiation of non-invasive ventilation (NIV) can be achieved early. Notably, nocturnal hypercapnia may be present long before patients report sleep disturbances or dyspnea [73]. For identification of patients who should be referred for sleep studies, predictors of nocturnal hypoventilation and impending respiratory failure are desirable. Bedside tests of respiratory muscle strength include forced vital capacity (FVC), maximum inspiratory pressure (MIP), and sniff nasal inspiratory pressure (SNIP), all being predictors of survival and disease progression [74,75,76]. For prediction of nocturnal hypoventilation and NIV indication, SNIP might be most suitable in ALS [77•, 78] but FVC and MIP should be regularly monitored because current guidelines for initiation of NIV in patients with neuromuscular disease rely on these measures [79]. In two recent studies, several factors have been found to be associated with early onset and rapid deterioration of respiratory insufficiency, including higher age at diagnosis, longer diagnostic delay, lower FVC and body mass index, bulbar onset of symptoms, and a lower ALS functional rating scale (ALSFRS-R) total score or dyspnea subscore, respectively [80, 81•]. Another study showed that nocturnal oxygen desaturations are also associated with respiratory failure and worse prognosis [82].
A plethora of retrospective studies and one randomized trial confirmed that NIV prolongs survival in patients with ALS [17, 83,84,85,86,87,88,89,90,91,92,93,94,95]. Furthermore, recent work suggests that effects on life expectancy are stronger when NIV is started early, i.e., in patients with only mild FVC reduction [96••]. Long-term NIV has the potential to sustainably improve sleep quality and quality of life although ventilator dependency progressively increases over time [67, 69, 97,98,99]. As prerequisites of these effects, optimal mask fitting, adequate titration of respirator settings, and education of patients and caregivers are all crucial. Treatment adherence is strongly influenced by mask selection and fitting. Nasal interfaces are often less uncomfortable but may be insufficient if mouth leaks occur, and oronasal masks may be preferred [100]. However, the latter may promote treatment-induced upper airway obstruction, most likely by dorsal displacement of the tongue, which requires adjustment of pressure settings and end-expiratory pressure, in particular [101]. Furthermore, upper airway obstruction may occur independently of the type of mask in patients with pseudobulbar palsy, in particular. Upper motor neuron dysfunction at the bulbar level has recently been shown to put affected patients at risk of intermittent glottic closure as well as decreased respiratory drive rendering NIV transiently ineffective when both coincide [102•].
Volume support ventilation has been proven to be especially effective with regard to gas exchange and symptom alleviation but may promote patient-ventilator dyssynchrony as reflected by ineffective or inappropriate triggering, auto-triggering, or flow dyssynchrony [103]. Follow-up sleep studies should comprise poly(somno)graphy and capnometry because prognosis may be worse when normocapnia, normoxia, and normalization of the apnea hypopnea index are not reliably achieved by NIV [104, 105, 106•].
Whereas older studies did not show that NIV specifically prolongs life span in patients with bulbar ALS [88], recent work suggests the opposite [107]. Furthermore, NIV improves quality of life and sleep quality in this subgroup [67, 69]. However, dysphagia and mucus retention have to be taken in account with particular care if bulbar disease is present. In general, management of secretions is highly important for all ALS patients with respiratory muscle weakness, including manually assisted coughing or mechanical cough assistance [108, 109].
Behavioral Abnormalities During Sleep
Behavioral abnormalities during sleep, or parasomnias, include movements or behaviors which either arise from sleep or occur on falling asleep or awakening. Parasomnias are characterized by partial arousals from either non-REM or REM sleep [32]. No evidence is available suggesting that NREM parasomnias (i.e., sleepwalking, pavor nocturnus, or confusional arousals) specifically occur in patients with ALS. REM behavioral disorder (RBD) is characterized by persistent phasic or tonic muscle activation during REM sleep [110]. Patients with manifest RBD show dream-enacting movements and vocalizations possibly leading to injuries, bed falls, or aggressive behaviors involving the bed partner [32]. RBD is mainly associated with neurodegenerative disorders and synucleinopathies in particular [111, 112] but may not exclusively relate to α-synuclein pathology since it has been reported in anti-IgLON5 disease, frontotemporal dementia, and certain rare forms of familial ALS [113,114,115,116]. In sporadic ALS, RBD or REM sleep without atonia may be found in a small number of patients possibly indicating that neurodegeneration involves REM sleep regulatory pathways [50]. Further systematic studies are desirable to elucidate both the pathophysiology and clinical relevance of this observation.
Conclusions and Future Perspectives
Sleep disturbances are common in patients with ALS and significantly add to the individual burden of disease. Major causes comprise sleep-disordered breathing, immobilization, muscle cramps, RLS, and other painful or unpleasant sensations which are mostly attributable to progressive impairment of motor function. Sleep-related symptoms have to be actively asked for, and treatable conditions should be treated in order to improve well-being and quality of life. Apart from clearly physical causes of sleep disruption, psychological aspects such as fear, depression, or recurrent grief and despair have to be acknowledged and may significantly contribute to insomnia in patients with ALS [117, 118]. With regard to disease-specific characteristics of sleep composition and regulation, future research will extend preliminary evidence from recent studies suggesting that motor control during REM sleep [50], sympathovagal balance [119], and central respiratory control [102•] may all be altered in patients with ALS, possibly contributing to sleep disruption already in early stages of the disease.
Abbreviations
- ALS:
-
Amyotrophic lateral sclerosis
- ALS-FRS-R:
-
ALS functional rating scale (revised)
- FVC:
-
Forced vital capacity
- MIP:
-
Maximum inspiratory pressure
- NIV:
-
Non-invasive ventilation
- OSA:
-
Obstructive sleep apnea
- PLM:
-
Periodic leg movements
- RBD:
-
REM sleep behavioral disorder
- REM:
-
Rapid eye movement
- RLS:
-
Restless legs syndrome
- SNIP:
-
Sniff nasal inspiratory pressure
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Grad LI, Rouleau GA, Ravits J, Cashman NR. Clinical spectrum of amyotrophic lateral sclerosis (ALS). Cold Spring Harb Perspect Med. 2017;7:a024117.
•• Hardiman O, Al-Chalabi A, Chio A, Corr EM, Logroscino G, Robberecht W, et al. Amyotrophic lateral sclerosis. Nat Rev Dis Primers. 2017;3:17071. This review article gives a comprehensive overview on ALS and current concepts with regard to pathophysiology, genetics, and treatment.
Nakken O, Lindstrom JC, Tysnes OB, Holmoy T. Assessing amyotrophic lateral sclerosis prevalence in Norway from 2009 to 2015 from compulsory nationwide health registers. Amyotroph Lateral Scler Frontotemporal Degener. 2018;19(3–4):303–10.
Kab S, Moisan F, Preux PM, Marin B, Elbaz A. Nationwide incidence of motor neuron disease using the French health insurance information system database. Amyotroph Lateral Scler Frontotemporal Degener. 2017;18(5–6):426–33.
Rosenbohm A, Peter RS, Erhardt S, Lule D, Rothenbacher D, Ludolph AC, et al. Epidemiology of amyotrophic lateral sclerosis in Southern Germany. J Neurol. 2017;264(4):749–57.
Ragonese P, Cellura E, Aridon P, D'Amelio M, Spataro R, Taiello AC, et al. Incidence of amyotrophic lateral sclerosis in Sicily: a population based study. Amyotroph Lateral Scler. 2012;13(3):284–7.
Chio A, Mora G, Calvo A, Mazzini L, Bottacchi E, Mutani R, et al. Epidemiology of ALS in Italy: a 10-year prospective population-based study. Neurology. 2009;72(8):725–31.
Alonso A, Logroscino G, Jick SS, Hernan MA. Incidence and lifetime risk of motor neuron disease in the United Kingdom: a population-based study. Eur J Neurol. 2009;16(6):745–51.
Foster LA, Salajegheh MK. Motor neuron disease: pathophysiology, diagnosis, and management. Am J Med. 2019;132(1):32–7.
Lacomblez L, Bensimon G, Leigh PN, Guillet P, Powe L, Durrleman S, et al. A confirmatory dose-ranging study of riluzole in ALS. ALS/Riluzole Study Group-II. Neurology. 1996;47(6 Suppl 4):S242–50.
Lacomblez L, Bensimon G, Leigh PN, Guillet P, Meininger V. Dose-ranging study of riluzole in amyotrophic lateral sclerosis. Amyotrophic Lateral Sclerosis/Riluzole Study Group II. Lancet. 1996;347(9013):1425–31.
Bensimon G, Lacomblez L, Meininger V. A controlled trial of riluzole in amyotrophic lateral sclerosis. ALS/Riluzole Study Group. N Engl J Med. 1994;330(9):585–91.
Writing Group On Behalf Of The Edaravone ALS Study Group. Exploratory double-blind, parallel-group, placebo-controlled study of edaravone (MCI-186) in amyotrophic lateral sclerosis (Japan ALS severity classification: grade 3, requiring assistance for eating, excretion or ambulation). Amyotroph Lateral Scler Frontotemporal Degener. 2017;18:40–8.
Takei K, Takahashi F, Liu S, Tsuda K, Palumbo J. Post-hoc analysis of randomised, placebo-controlled, double-blind study (MCI186-19) of edaravone (MCI-186) in amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener. 2017;18(sup1):49–54.
•• Andersen PM, Abrahams S, Borasio GD, de Carvalho M, Chio A, Van Damme P, et al. EFNS guidelines on the clinical management of amyotrophic lateral sclerosis (MALS)--revised report of an EFNS task force. Eur J Neurol. 2012;19(3):360–75. This guideline document outlines all issues that are relevant for pharmacological, symptomatic, and palliative treatment of ALS.
Traxinger K, Kelly C, Johnson BA, Lyles RH, Glass JD. Prognosis and epidemiology of amyotrophic lateral sclerosis: analysis of a clinic population, 1997-2011. Neurol Clin Pract. 2013;3(4):313–20.
Zoccolella S, Beghi E, Palagano G, Fraddosio A, Guerra V, Samarelli V, et al. Analysis of survival and prognostic factors in amyotrophic lateral sclerosis: a population based study. J Neurol Neurosurg Psychiatry. 2008;79(1):33–7.
Calvo A, Moglia C, Lunetta C, Marinou K, Ticozzi N, Ferrante GD, et al. Factors predicting survival in ALS: a multicenter Italian study. J Neurol. 2017;264(1):54–63.
Spataro R, Lo Re M, Piccoli T, Piccoli F, La Bella V. Causes and place of death in Italian patients with amyotrophic lateral sclerosis. Acta Neurol Scand. 2010;122(3):217–23.
Gil J, Funalot B, Verschueren A, Danel-Brunaud V, Camu W, Vandenberghe N, et al. Causes of death amongst French patients with amyotrophic lateral sclerosis: a prospective study. Eur J Neurol. 2008;15(11):1245–51.
Bourke SC, McColl E, Shaw PJ, Gibson GJ. Validation of quality of life instruments in ALS. Amyotroph Lateral Scler Other Motor Neuron Disord. 2004;5(1):55–60.
Bromberg MB. Quality of life in amyotrophic lateral sclerosis. Phys Med Rehabil Clin N Am. 2008;19(3):591–605 x-xi.
Epton J, Harris R, Jenkinson C. Quality of life in amyotrophic lateral sclerosis/motor neuron disease: a structured review. Amyotroph Lateral Scler. 2009;10(1):15–26.
Burke T, Galvin M, Pinto-Grau M, Lonergan K, Madden C, Mays I, et al. Caregivers of patients with amyotrophic lateral sclerosis: investigating quality of life, caregiver burden, service engagement, and patient survival. J Neurol. 2017;264(5):898–904.
Raheja D, Stephens HE, Lehman E, Walsh S, Yang C, Simmons Z. Patient-reported problematic symptoms in an ALS treatment trial. Amyotroph Lateral Scler Frontotemporal Degener. 2016;17(3–4):198–205.
Panda S, Gourie-Devi M, Sharma A. Sleep disorders in amyotrophic lateral sclerosis: a questionnaire-based study from India. Neurol India. 2018;66(3):700–8.
Lo Coco D, La Bella V. Fatigue, sleep, and nocturnal complaints in patients with amyotrophic lateral sclerosis. Eur J Neurol. 2012;19(5):760–3.
Lo Coco D, Mattaliano P, Spataro R, Mattaliano A, La Bella V. Sleep-wake disturbances in patients with amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2011;82(8):839–42.
Diaz-Abad M, Buczyner JR, Venza BR, Scharf SM, Kwan JY, Lubinski B, et al. Poor sleep quality in patients with amyotrophic lateral sclerosis at the time of diagnosis. J Clin Neuromuscul Dis. 2018;20(2):60–8.
Ahmed RM, Newcombe RE, Piper AJ, Lewis SJ, Yee BJ, Kiernan MC, et al. Sleep disorders and respiratory function in amyotrophic lateral sclerosis. Sleep Med Rev. 2016;26:33–42.
Montagna P, Liguori R, Zucconi M, Lugaresi A, Cirignotta F, Lugaresi E. Fasciculations during wakefulness and sleep. Acta Neurol Scand. 1987;76(2):152–4.
American Academy of Sleep Medicine. International classification of sleep disorders: American Academy of Sleep Medicine. 2014.
Caress JB, Ciarlone SL, Sullivan EA, Griffin LP, Cartwright MS. Natural history of muscle cramps in amyotrophic lateral sclerosis. Muscle Nerve. 2016;53(4):513–7.
Baldissera F, Cavallari P, Dworzak F. Motor neuron ‘bistability’. A pathogenetic mechanism for cramps and myokymia. Brain. 1994;117(Pt 5):929–39.
Oskarsson B, Moore D, Mozaffar T, Ravits J, Wiedau-Pazos M, Parziale N, et al. Mexiletine for muscle cramps in amyotrophic lateral sclerosis: a randomized, double-blind crossover trial. Muscle Nerve. 2018;58:42–8.
Baldinger R, Katzberg HD, Weber M. Treatment for cramps in amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst Rev. 2012;4:CD004157.
El-Tawil S, Al Musa T, Valli H, Lunn MP, Brassington R, El-Tawil T, et al. Quinine for muscle cramps. Cochrane Database Syst Rev. 2015;4:CD005044.
Hogan DB. Quinine: not a safe drug for treating nocturnal leg cramps. CMAJ. 2015;187(4):237–8.
Hayashi T, Narita Y, Okugawa N, Hamaguchi E, Shibahara M, Kuzuhara S. Pressure ulcers in ALS patients on admission at a university hospital in Japan. Amyotroph Lateral Scler. 2007;8(5):310–3.
Ono S, Toyokura Y, Mannen T, Ishibashi Y. Increased dermal collagen density in amyotrophic lateral sclerosis. J Neurol Sci. 1988;83(1):81–92.
Abetz L, Allen R, Follet A, Washburn T, Earley C, Kirsch J, et al. Evaluating the quality of life of patients with restless legs syndrome. Clin Ther. 2004;26(6):925–35.
Limousin N, Blasco H, Corcia P, Arnulf I, Praline J. The high frequency of restless legs syndrome in patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2011;12(4):303–6.
Liu S, Shen D, Tai H, Su N, Ding Q, Fu H, et al. Restless legs syndrome in Chinese patients with sporadic amyotrophic lateral sclerosis. Front Neurol. 2018;9:735.
Lo Coco D, Piccoli F, La Bella V. Restless legs syndrome in patients with amyotrophic lateral sclerosis. Mov Disord. 2010;25(15):2658–61.
Dalla Bella E, Lombardi R, Porretta-Serapiglia C, Ciano C, Gellera C, Pensato V, et al. Amyotrophic lateral sclerosis causes small fiber pathology. Eur J Neurol. 2016;23(2):416–20.
Weis J, Katona I, Muller-Newen G, Sommer C, Necula G, Hendrich C, et al. Small-fiber neuropathy in patients with ALS. Neurology. 2011;76(23):2024–9.
Isak B, Tankisi H, Johnsen B, Pugdahl K, Torvin MA, Finnerup NB, et al. Involvement of distal sensory nerves in amyotrophic lateral sclerosis. Muscle Nerve. 2016;54(6):1086–92.
Garcia-Borreguero D, Silber MH, Winkelman JW, Hogl B, Bainbridge J, Buchfuhrer M, et al. Guidelines for the first-line treatment of restless legs syndrome/Willis-Ekbom disease, prevention and treatment of dopaminergic augmentation: a combined task force of the IRLSSG, EURLSSG, and the RLS-foundation. Sleep Med. 2016;21:1–11.
Puligheddu M, Congiu P, Arico D, Rundo F, Borghero G, Marrosu F, et al. Isolated rapid eye movement sleep without atonia in amyotrophic lateral sclerosis. Sleep Med. 2016;26:16–22.
Lo Coco D, Puligheddu M, Mattaliano P, Congiu P, Borghero G, Fantini ML, et al. REM sleep behavior disorder and periodic leg movements during sleep in ALS. Acta Neurol Scand. 2017;135(2):219–24.
• Boentert M, Glatz C, Helmle C, Okegwo A, Young P. Prevalence of sleep apnoea and capnographic detection of nocturnal hypoventilation in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2018;89(4):418–24. This large retrospective study proves that transcutaneous capnometry is superior to pulse oximetry for detection of sleep-related hypoventilation.
Reyhani A, Benbir Senel G, Karadeniz D. Effects of sleep-related disorders on the prognosis of amyotrophic lateral sclerosis. Neurodegener Dis. 2020:1–7.
Bara-Jimenez W, Aksu M, Graham B, Sato S, Hallett M. Periodic limb movements in sleep: state-dependent excitability of the spinal flexor reflex. Neurology. 2000;54(8):1609–16.
Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. J Pain. 2013;14(12):1539–52.
Cheatle MD, Foster S, Pinkett A, Lesneski M, Qu D, Dhingra L. Assessing and managing sleep disturbance in patients with chronic pain. Sleep Med Clin. 2016;11(4):531–41.
Moisset X, Cornut-Chauvinc C, Clavelou P, Pereira B, Dallel R, Guy N. Is there pain with neuropathic characteristics in patients with amyotrophic lateral sclerosis? A cross-sectional study. Palliat Med. 2016;30(5):486–94.
• Wallace VC, Ellis CM, Burman R, Knights C, Shaw CE, Al-Chalabi A. The evaluation of pain in amyotrophic lateral sclerosis: a case controlled observational study. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15(7–8):520–7. This study outlines the epidemiology and clinical determinants of chronic pain in patients with ALS.
Nijs J, Torres-Cueco R, van Wilgen CP, Girbes EL, Struyf F, Roussel N, et al. Applying modern pain neuroscience in clinical practice: criteria for the classification of central sensitization pain. Pain Physician. 2014;17(5):447–57.
Ziegler EA, Magerl W, Meyer RA, Treede RD. Secondary hyperalgesia to punctate mechanical stimuli. Central sensitization to A-fibre nociceptor input. Brain. 1999;122(Pt 12):2245–57.
Chio A, Mora G, Lauria G. Pain in amyotrophic lateral sclerosis. Lancet Neurol. 2017;16(2):144–57.
Ganzini L, Silveira MJ, Johnston WS. Predictors and correlates of interest in assisted suicide in the final month of life among ALS patients in Oregon and Washington. J Pain Symptom Manag. 2002;24(3):312–7.
Ferguson KA, Strong MJ, Ahmad D, George CF. Sleep-disordered breathing in amyotrophic lateral sclerosis. Chest. 1996;110(3):664–9.
Santos C, Braghiroli A, Mazzini L, Pratesi R, Oliveira LV, Mora G. Sleep-related breathing disorders in amyotrophic lateral sclerosis. Monaldi Arch Chest Dis. 2003;59(2):160–5.
Lyall RA, Donaldson N, Polkey MI, Leigh PN, Moxham J. Respiratory muscle strength and ventilatory failure in amyotrophic lateral sclerosis. Brain. 2001;124(Pt 10):2000–13.
Quaranta VN, Carratu P, Damiani MF, Dragonieri S, Capozzolo A, Cassano A, et al. The prognostic role of obstructive sleep apnea at the onset of amyotrophic lateral sclerosis. Neurodegener Dis. 2017;17(1):14–21.
Berger KI, Rapoport DM, Ayappa I, Goldring RM. Pathophysiology of hypoventilation during sleep. Sleep Med Clin. 2014;9:289–300.
Boentert M, Brenscheidt I, Glatz C, Young P. Effects of non-invasive ventilation on objective sleep and nocturnal respiration in patients with amyotrophic lateral sclerosis. J Neurol. 2015;262(9):2073–82.
Katzberg HD, Selegiman A, Guion L, Yuan N, Cho SC, Katz JS, et al. Effects of noninvasive ventilation on sleep outcomes in amyotrophic lateral sclerosis. J Clin Sleep Med. 2013;9(4):345–51.
Vrijsen B, Buyse B, Belge C, Robberecht W, Van Damme P, Decramer M, et al. Noninvasive ventilation improves sleep in amyotrophic lateral sclerosis: a prospective polysomnographic study. J Clin Sleep Med. 2015;11(5):559–66.
David WS, Bundlie SR, Mahdavi Z. Polysomnographic studies in amyotrophic lateral sclerosis. J Neurol Sci. 1997;152(Suppl 1):S29–35.
Arnulf I, Similowski T, Salachas F, Garma L, Mehiri S, Attali V, et al. Sleep disorders and diaphragmatic function in patients with amyotrophic lateral sclerosis. Am J Respir Crit Care Med. 2000;161(3 Pt 1):849–56.
Ogna A, Quera Salva MA, Prigent H, Mroue G, Vaugier I, Annane D, et al. Nocturnal hypoventilation in neuromuscular disease: prevalence according to different definitions issued from the literature. Sleep Breath. 2016;20(2):575–81.
Barthlen GM, Lange DJ. Unexpectedly severe sleep and respiratory pathology in patients with amyotrophic lateral sclerosis. Eur J Neurol. 2000;7(3):299–302.
Fitting JW, Paillex R, Hirt L, Aebischer P, Schluep M. Sniff nasal pressure: a sensitive respiratory test to assess progression of amyotrophic lateral sclerosis. Ann Neurol. 1999;46(6):887–93.
Morgan RK, McNally S, Alexander M, Conroy R, Hardiman O, Costello RW. Use of sniff nasal-inspiratory force to predict survival in amyotrophic lateral sclerosis. Am J Respir Crit Care Med. 2005;171(3):269–74.
Czaplinski A, Yen AA, Appel SH. Forced vital capacity (FVC) as an indicator of survival and disease progression in an ALS clinic population. J Neurol Neurosurg Psychiatry. 2006;77(3):390–2.
• Tilanus TBM, Groothuis JT, Tenbroek-Pastoor JMC, Feuth TB, Heijdra YF, Slenders JPL, et al. The predictive value of respiratory function tests for non-invasive ventilation in amyotrophic lateral sclerosis. Respir Res. 2017;18(1):144. This study nicely investigates which bedside tests of respiratory muscle strength are suitable to predict nocturnal hypoventilation and the need for non-invasive ventilatory support in ALS patients.
Carratu P, Cassano A, Gadaleta F, Tedone M, Dongiovanni S, Fanfulla F, et al. Association between low sniff nasal-inspiratory pressure (SNIP) and sleep disordered breathing in amyotrophic lateral sclerosis: preliminary results. Amyotroph Lateral Scler. 2011;12(6):458–63.
Windisch W, Dreher M, Geiseler J, Siemon K, Brambring J, Dellweg D, et al. Guidelines for non-invasive and invasive home mechanical ventilation for treatment of chronic respiratory failure - update 2017. Pneumologie. 2017;71(11):722–95.
Ackrivo J, Hansen-Flaschen J, Jones BL, Wileyto EP, Schwab RJ, Elman L, et al. Classifying patients with amyotrophic lateral sclerosis by changes in FVC. A group-based trajectory analysis. Am J Respir Crit Care Med. 2019;200(12):1513–21.
• Ackrivo J, Hansen-Flaschen J, Wileyto EP, Schwab RJ, Elman L, Kawut SM. Development of a prognostic model of respiratory insufficiency or death in amyotrophic lateral sclerosis. Eur Respir J. 2019;53(4):1802237. This large study provides an evidence-based approach for prognostication of respiratory insufficiency in ALS.
Bote SM, Martinez NP, Amarilla CE, Ugalde PF, Gonzalez-Bermejo J, Collado NF, et al. Overnight pulse oximetry to determine prognostic factors in subjects with amyotrophic lateral sclerosis. Respir Care. 2020;respcare.07154. https://doi.org/10.4187/respcare.07154.
Aboussouan LS, Khan SU, Banerjee M, Arroliga AC, Mitsumoto H. Objective measures of the efficacy of noninvasive positive-pressure ventilation in amyotrophic lateral sclerosis. Muscle Nerve. 2001;24(3):403–9.
Aboussouan LS, Khan SU, Meeker DP, Stelmach K, Mitsumoto H. Effect of noninvasive positive-pressure ventilation on survival in amyotrophic lateral sclerosis. Ann Intern Med. 1997;127(6):450–3.
Bach JR. Amyotrophic lateral sclerosis: predictors for prolongation of life by noninvasive respiratory aids. Arch Phys Med Rehabil. 1995;76(9):828–32.
Bach JR. Amyotrophic lateral sclerosis: prolongation of life by noninvasive respiratory AIDS. Chest. 2002;122(1):92–8.
Bertella E, Banfi P, Paneroni M, Grilli S, Bianchi L, Volpato E, et al. Early initiation of night-time NIV in an outpatient setting: a randomized non-inferiority study in ALS patients. Eur J Phys Rehabil Med. 2017;53(6):892–9.
Bourke SC, Tomlinson M, Williams TL, Bullock RE, Shaw PJ, Gibson GJ. Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: a randomised controlled trial. The Lancet Neurology. 2006;5(2):140–7.
Burkhardt C, Neuwirth C, Sommacal A, Andersen PM, Weber M. Is survival improved by the use of NIV and PEG in amyotrophic lateral sclerosis (ALS)? A post-mortem study of 80 ALS patients. PLoS One. 2017;12(5):e0177555.
Butz M, Wollinsky KH, Wiedemuth-Catrinescu U, Sperfeld A, Winter S, Mehrkens HH, et al. Longitudinal effects of noninvasive positive-pressure ventilation in patients with amyotrophic lateral sclerosis. Am J Phys Med Rehabil. 2003;82(8):597–604.
Chio A, Calvo A, Moglia C, Gamna F, Mattei A, Mazzini L, et al. Non-invasive ventilation in amyotrophic lateral sclerosis: a 10 year population based study. J Neurol Neurosurg Psychiatry. 2012;83(4):377–81.
Elamin EM, Wilson CS, Sriaroon C, Crudup B, Pothen S, Kang YC, et al. Effects of early introduction of non-invasive positive pressure ventilation based on forced vital capacity rate of change: variation across amyotrophic lateral sclerosis clinical phenotypes. Int J Clin Pract. 2019;73(1):e13257.
Kleopa KA, Sherman M, Neal B, Romano GJ, Heiman-Patterson T. Bipap improves survival and rate of pulmonary function decline in patients with ALS. J Neurol Sci. 1999;164(1):82–8.
Pinto AC, Evangelista T, Carvalho M, Alves MA, Sales Luis ML. Respiratory assistance with a non-invasive ventilator (Bipap) in MND/ALS patients: survival rates in a controlled trial. J Neurol Sci. 1995;129(Suppl):19–26.
Sivori M, Rodriguez GE, Pascansky D, Saenz C, Sica RE. Outcome of sporadic amyotrophic lateral sclerosis treated with non-invasive ventilation and riluzole. Medicina. 2007;67(4):326–30.
•• Vitacca M, Montini A, Lunetta C, Banfi P, Bertella E, De Mattia E, et al. Impact of an early respiratory care programme with non-invasive ventilation adaptation in patients with amyotrophic lateral sclerosis. Eur J Neurol. 2018;25(3):556–e33. This large retrospective study supports the notion that non-invasive ventilation has substantial prognostic impact in ALS patients with both spinal and bulbar onset of disease.
Vandoorne E, Vrijsen B, Belge C, Testelmans D, Buyse B. Noninvasive ventilation in amyotrophic lateral sclerosis: effects on sleep quality and quality of life. Acta Clin Belg. 2016;71(6):389–94.
Mustfa N, Walsh E, Bryant V, Lyall RA, Addington-Hall J, Goldstein LH, et al. The effect of noninvasive ventilation on ALS patients and their caregivers. Neurology. 2006;66(8):1211–7.
Lyall RA, Donaldson N, Fleming T, Wood C, Newsom-Davis I, Polkey MI, et al. A prospective study of quality of life in ALS patients treated with noninvasive ventilation. Neurology. 2001;57(1):153–6.
Teschler H, Stampa J, Ragette R, Konietzko N, Berthon-Jones M. Effect of mouth leak on effectiveness of nasal bilevel ventilatory assistance and sleep architecture. Eur Respir J. 1999;14(6):1251–7.
Schellhas V, Glatz C, Beecken I, Okegwo A, Heidbreder A, Young P, et al. Upper airway obstruction induced by non-invasive ventilation using an oronasal interface. Sleep Breath. 2018;22(3):781–8.
• Sancho J, Bures E, Ferrer S, Ferrando A, Banuls P, Servera E. Unstable control of breathing can lead to ineffective noninvasive ventilation in amyotrophic lateral sclerosis. ERJ Open Res. 2019;5(3):00099-2019. As a novelty, this study shows that central breathing control during sleep may be altered in ALS.
Sancho J, Servera E, Morelot-Panzini C, Salachas F, Similowski T, Gonzalez-Bermejo J. Non-invasive ventilation effectiveness and the effect of ventilatory mode on survival in ALS patients. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15(1–2):55–61.
Georges M, Attali V, Golmard JL, Morelot-Panzini C, Crevier-Buchman L, Collet JM, et al. Reduced survival in patients with ALS with upper airway obstructive events on non-invasive ventilation. J Neurol Neurosurg Psychiatry. 2016;87(10):1045–50.
Gonzalez-Bermejo J, Morelot-Panzini C, Arnol N, Meininger V, Kraoua S, Salachas F, et al. Prognostic value of efficiently correcting nocturnal desaturations after one month of non-invasive ventilation in amyotrophic lateral sclerosis: a retrospective monocentre observational cohort study. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14(5–6):373–9.
• Ogna A, Nardi J, Prigent H, Quera Salva MA, Chaffaut C, Lamothe L, et al. Prognostic value of initial assessment of residual hypoventilation using nocturnal capnography in mechanically ventilated neuromuscular patients: a 5-year follow-up study. Front Med (Lausanne). 2016;3:40. This study is not ALS-specific but provides important evidence that after initiation of non-invasive ventilation in patients with neuromuscular disease residual hypercapnia during sleep is associated with worse prognosis.
Sancho J, Martinez D, Bures E, Diaz JL, Ponz A, Servera E. Bulbar impairment score and survival of stable amyotrophic lateral sclerosis patients after noninvasive ventilation initiation. ERJ Open Res. 2018;4(2):00159-2017.
Vitacca M, Paneroni M, Trainini D, Bianchi L, Assoni G, Saleri M, et al. At home and on demand mechanical cough assistance program for patients with amyotrophic lateral sclerosis. Am J Phys Med Rehabil. 2010;89(5):401–6.
Mustfa N, Aiello M, Lyall RA, Nikoletou D, Olivieri D, Leigh PN, et al. Cough augmentation in amyotrophic lateral sclerosis. Neurology. 2003;61(9):1285–7.
Luppi PH, Clement O, Sapin E, Gervasoni D, Peyron C, Leger L, et al. The neuronal network responsible for paradoxical sleep and its dysfunctions causing narcolepsy and rapid eye movement (REM) behavior disorder. Sleep Med Rev. 2011;15(3):153–63.
Iranzo A, Fernandez-Arcos A, Tolosa E, Serradell M, Molinuevo JL, Valldeoriola F, et al. Neurodegenerative disorder risk in idiopathic REM sleep behavior disorder: study in 174 patients. PLoS One. 2014;9(2):e89741.
Boeve BF, Silber MH, Ferman TJ, Lin SC, Benarroch EE, Schmeichel AM, et al. Clinicopathologic correlations in 172 cases of rapid eye movement sleep behavior disorder with or without a coexisting neurologic disorder. Sleep Med. 2013;14(8):754–62.
Cagnin A, Mariotto S, Fiorini M, Gaule M, Bonetto N, Tagliapietra M, et al. Microglial and neuronal TDP-43 pathology in anti-IgLON5-related tauopathy. J Alzheimers Dis. 2017;59(1):13–20.
Lo Coco D, Caruso G, Mattaliano A. REM sleep behavior disorder in patients with DJ-1 mutations and parkinsonism-dementia-ALS complex. Mov Disord. 2009;24(10):1555–6.
Lo Coco D, Cupidi C, Mattaliano A, Baiamonte V, Realmuto S, Cannizzaro E. REM sleep behavior disorder in a patient with frontotemporal dementia. Neurol Sci. 2012;33(2):371–3.
Ebben MR, Shahbazi M, Lange DJ, Krieger AC. REM behavior disorder associated with familial amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2012;13(5):473–4.
Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135(1–3):10–9.
Skapinakis P, Rai D, Anagnostopoulos F, Harrison S, Araya R, Lewis G. Sleep disturbances and depressive symptoms: an investigation of their longitudinal association in a representative sample of the UK general population. Psychol Med. 2013;43(2):329–39.
Congiu P, Mariani S, Milioli G, Parrino L, Tamburrino L, Borghero G, et al. Sleep cardiac dysautonomia and EEG oscillations in amyotrophic lateral sclerosis. Sleep. 2019;42(11):zsz164.
Funding
Open Access funding provided by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that he has no competing interests in the context of this work.
Human and Animal Rights and Informed Consent
For this review, no ethical approval was required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sleep
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Boentert, M. Sleep and Sleep Disruption in Amyotrophic Lateral Sclerosis. Curr Neurol Neurosci Rep 20, 25 (2020). https://doi.org/10.1007/s11910-020-01047-1
Published:
DOI: https://doi.org/10.1007/s11910-020-01047-1