Abstract
Inappropriate sleep duration and poor sleep quality are associated with risk of stroke, but their interactive effect on stroke is unknown. We explored the interactive effect of sleep quality and duration on stroke risk. A prospective cohort study was conducted with 41,786 adults. Sleep quality was assessed using the Pittsburgh Sleep Quality Index. Sleep duration was measured by average hours of sleep per night. Cox regression models were used to calculate the association of sleep duration and quality with stroke. The delta method and a non-conditional logistic regression model were used and the relative excess risk due to interaction (RERI), the attributable proportion (AP), and the synergy index (S) were calculated. Compared with sleep duration 6–8 h/day, the risk ratio of stroke was 1.63 (1.23–2.11) times for sleep duration <6 h/day and 1.40 (1.08–1.75) times for >8 h/day. The stroke risk ratio was 2.37 (1.52–3.41) times in subjects with poor sleep quality compared with those with good sleep quality. Women who slept <6 h/day had higher stroke risk than men who slept <6 h/day. Men who slept >8 h/day had higher stroke risk than women who slept >8 h/day. Men with poor sleep quality had higher stroke risk than women with poor sleep quality. Stroke was associated with short/long sleep duration and poor sleep quality in subjects aged >46 years, compared with those aged 18–45 years. Stroke occurred more frequently in subjects with poor sleep quality combined with short sleep duration (odds ratio: 6.75; 95% confidence interval (CI): 2.45–14.12). RERI, AP, and S values (and their 95% CIs) were 5.54 (3.75–8.12), 0.72 (0.56–0.80), and 5.69 (4.23–9.90) for the poor sleep quality interact with short sleep duration. In persons with poor sleep quality accompanied by long sleep duration, RERI, AP, and S (95% CI) were 1.12 (1.01–1.27), 0.35 (0.26–0.51), and 2.05 (1.57–2.96), respectively. Subjective sleep disturbances are related with risk of stroke in Chinese adults. There are additive interactions between short/long sleep duration and poor sleep quality that affect risk of stroke.
Similar content being viewed by others
Introduction
As the top cause of death and disability and the second leading cause of years of potential life lost, stroke killed over 6 million deaths in 2015 worldwide, and the number will be doubled by 2030, with over 200 million disability-adjusted life years each year1,2. The burden is the biggest in China: 1,114.8/100,000 of the age-standardized prevalence rate in 20133 and annual increase of 11.9% for the first-ever stroke morbidity during 1992-20154. With respect to the traditional risk factors of stroke in China, hypertension, smoking, alcohol use, diabetes, and hypercholesterolemia are prevalent and could also be modified3,5. Some studies have shown that stroke is associated with poor sleep quality and sleep duration6,7,8, while others have insistent results9,10, which might partly due to different races11. Therefore, sleep quality in relation with stroke should be further investigated to determine whether stroke prevention programs should incorporate efforts to reduce sleep disturbances in different races.
Sleep disturbances and insufficient sleep quantity are very common in Chinese adults12,13. However, few studies report the relationship between sleep quality and stroke14,15. Therefore, identifying and describing the relationship, and implementing early intervention measures to are extremely important in modifying the risk factor and in further slowing the progression of the disease in China. To this end, the current study aims to examine the effects and the interactive effect of sleep quality and sleep duration on stroke, respectively, in Chinese adults.
Methods
Study protocol and population
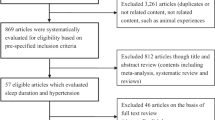
The baseline survey with a sample selected from all of the eleven regions of Xuzhou city, Jiangsu province, China, was conducted in, during May to November 2009. A two-stage sampling probability proportional to size (PPS) was used, and each region was considered a stratum, yielding a total of 11 strata. Five subdistricts/townships in urban/rural areas were firstly selected randomly from each stratum using PPS based on the population data. Then five communities/villages were randomly selected from each subdistrict/township using PPS and a total of 275 villages or communities, as clusters, were selected. In each selected village or community, a list of households containing adults aged ≥18 years and living their current residence for at least 5 years was generated. Finally, a Kish selection table was used to select one person from each household. The exclusion criteria included: (1) previous diagnosis of neuropathy, psychosis, or difficulty in communication, or (2) the floating population or temporary residents, or (3) obstructive sleep apnea. At least 13,500 people should be recruited assuming an estimation incidence of stroke of 2.0%15 with 90% power, α level of 0.05, and allowing for a dropout rate of 15%. Overall 41,786 permanent residents aged ≥18 years participated in the survey, with a response rate of 91.6% (41,786/45,618). All participants were rechecked from May to November 2017. A total of 672 participants had stroke, and 1,585 participants were excluded owing to missing information about sleep duration or sleep quality; diagnosis of neuropathy or psychosis; use of any kind of psychotropic medication; severe heart, liver, or kidney disease, and/or cancer, producing a total of 39,533 participants in this prospective observational study. The interval of follow-up duration was the time between the baseline assessment and the diagnosis of stroke, death, or the date on which the 2017 questionnaire was finished. Those who developed strokes or died from strokes in the follow-up, and those who fulfilled the final research, were included in the present study. The main reasons for participant loss were death, migration, or other personal reasons at follow-up. All participants were of Han nationality.
Key measures
Sleep quality and disturbance over a 1-month length was estimated by a Chinese version of the Pittsburgh Sleep Quality Index (PSQI)16. This version has seven components and a total score from 0 to 21 points with reliability coefficient of 0.82–0.83 and acceptable test–retest reliability of 0.77–0.8517. PSQI score of ≤5 and >5 was correspondingly differentiated as good and poor sleep quality, respectively. The diagnostic sensitivity and specificity in differentiating poor from good sleepers were 89.6% and 86.5%, respectively. Sleep quantity was calculated on self-reported average total hours of per night sleep in the previous year, and was categorized as <6, 6–8, and >8 h per night, following previous studies6,7,12.
In the follow-up, data on strokes were collected using self-reports and medical record questionnaires. Self-reported stroke should meet the criteria of an acute disorder of focal areas in the brain continuing for ≥24 h caused by intracranial hemorrhage or ischemia18 with a diagnosis of computed tomography and magnetic resonance imaging scans. By definition, asymptomatic stroke and transient ischemic attack were excluded.
Variables
Participants were interviewed face-to-face and privately by trained interviewers using a standard questionnaire that assessed age, gender, marriage, occupation, educational level, cigarette use, alcohol use, physical activity, history of disease (type 2 diabetes mellitus (T2DM), obstructive sleep apnea, dyslipidemia, hypertension, heart disease, and cancer), and family history of disease (T2DM, hypertension, and stroke). Occupation was defined as manual, non-manual, unemployed, and retired. Educational level was classified as below high school, high school, and above high school level. Marriage was categorized as single, divorced, widowed, or separated; living conditions were sorted out as living alone or with someone else. Those who have smoked at least 100 cigarettes over the lifetime were defined as smokers. A drinker was defined as the consumption of no less than 30 g alcohol per week lasting 1 year or more. Physical activity was defined as joining moderate or vigorous activity for at least 30 min per day no less than 3 days a week. Weight in kilograms divided by height in meters squared was defined as body mass index (BMI) with categorized as underweight (≤18.5 kg/m2), normal weight (18.5–24.0 kg/m2), and overweight/obese (≥24.0 kg/m2); Women with waist circumference of >85 cm and men with that of >90 cm were defined as abdominal obesity19. T2DM was defined as fasting blood glucose of ≥7.0 mmol/L, or the use of any antidiabetic drugs, or self-reported history of T2DM20. Hypertension was characterized as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg, or the use of any antihypertensive drugs, or self-reported history of hypertension21. Dyslipidemia was defined as any lipid-lowering medication use or self-reported history of dyslipidemia. History of cardiovascular disease was defined as previous diagnosed ischemic heart disease and/or cerebrovascular events. A score of ≥3 on the STOP-Bang questionnaire indicated the presence of obstructive sleep apnea22.
Statistical analysis
Epidata 3.1 was used to build a database. Data were input separately by two people and a conformance test was performed. All statistical analyses were conducted by SPSS 16.0 (SPSS Inc., Chicago, USA).
Categorical variables were presented as frequencies and proportions or means (±standard deviation) and medians (interquartile range). Baseline characteristics of participants and non-participants in the follow-up examination were compared using the chi-square test, Student’s t-test, and the Mann–Whitney U test, as appropriate. The Mann–Whitney U test and Fisher’s exact test were used to compare the characteristics and sleep duration/qualities of participants who developed stroke with those who did not develop stroke. Risk ratios (RRs) and corresponding 95% confidence intervals (CI) were calculated using Cox regression models with reference to the risk of 7–8 h/day of sleep duration or good sleep quality, adjusting for age, gender, marital status, current employment status, educational level, BMI, cigarette use, alcohol intake, physical activity, DM2, fasting plasma sugar, lipids, dyslipidemia, hypertension, heart disease, family history of DM2, family history of hypertension, and family history of stroke. The observed prevalence of stroke was plotted and stratified by sleep quality and sleep duration. RRs and 95% CIs were also calculated for sleep duration and sleep quality in relation with age, adjusted by potential confounding factors, (gender, marital status, current employment status, educational level, BMI, cigarette use, alcohol intake, physical activity, DM2, fasting plasma sugar, lipids, dyslipidemia, hypertension, heart disease, family history of DM2, family history of hypertension, family history of stroke, and sleep quality and duration).
The Excel table compiled by Anderss et al.23 was introduced into the database using the delta method and relevant indicators of interaction were computed. The value obtained from the logistic regression model was taken as the estimated additive interaction between sleep quality and sleep duration. The following measures of interaction were examined to estimate biological interactions: the relative excess risk due to interaction (RERI), the attributable proportion due to interaction (AP), and the synergy index (S)24,25. The RERI is the excess risk attributed to the interaction relative to the risk without exposure. AP refers to the attributable proportion of disease caused by the interaction in subjects with both exposures. S is the excess risk from both exposures when there is a biological interaction relative to the risk from both exposures without interaction. In the absence of additive interactions, RERI and AP are equal to 025. Indicative biological interactions would be considered when RERI > 0, AP > 0, or S > 1. A P value <0.05 (two-tailed) was considered statistically significant.
Results
General characteristics of participants
A total of 39,533 participants (males, 48.1%) who did not have stroke at baseline and 27,712 out of them completed the follow-up in 2017, of whom 617 developed stroke The median follow-up duration was 7 years. At baseline, the mean age and the average sleep duration per night were 45.7 ± 15.1 years and 7.16 ± 1.07 h in 2009, respectively. The non-responder group was older (50.7 ± 16.8 vs 44.6 ± 15.1 years, P < 0.001), with more short- sleepers [(2,098/11,821) vs. (5,368/27,712), P < 0.01], more long-sleepers [(2,021/11,821) vs (5,232/27,712), P < 0.01], and more individuals with poor sleep quality [(1,053/11,821) vs (1,989/27,712), P < 0.01]. There were no significant between-group differences in other risk factors. With respective of the 27,712 participants, those with stroke tended to be older, smokers and drinkers and have a higher BMI. There were no significant gender differences in the other risk factors (Table 1).
Sleep quality and sleep duration in relation with stroke
The cumulative incidence of stroke was 2.22% in participants who completed the study. Individuals with short sleep duration (<6 h/day) significantly increased risk of stroke compared with those with sleep duration 6–8 h/day (for all, RR: 1.63, 95% CI: 1.23–2.11, P < 0.001; for men, RR: 1.45, 95% CI: 1.19–1.73, P < 0.001; for women, RR: 1.77, (95% CI: 1.41–2.37, P < 0.00), after adjusting for confounding factors. Women had a slightly stronger relationship than men. Individuals with long sleep duration also increased risk of stroke compared with those with sleep duration 6–8 h (for all, RR: 1.40, 95% CI: 1.08–1.75, P < 0.01; for men, RR: 1.48, 95% CI: 1.02–1.57, P < 0.01; for women, RR; 1.23, 95% CI: 1.12–1.79, P < 0.01), after adjusting for confounding factors (Table 2). males had a slightly stronger relationship than females. The population-attributable risk of short and long sleep duration on risk of stroke was 0.35 and 0.23, respectively. Subjects with poor sleep quality greatly raised risk of stroke compared with those with good sleep quality (RR: 2.37, 95% CI: 1.52–3.41, P < 0.001). The subgroup analysis classified by gender found a similar association between men and women. The RRs were 2.65 (95% CI: 1.72–4.57, P < 0.01) for men and 2.13 (95% CI: 1.45–2.77, P < 0.01) for women after adjustment, the association was stronger in males than that in females. The population-attributable risk of poor sleep quality on risk of stroke was 0.39. There was no significant association between good sleep quality and stroke with normal sleep quality as reference (RR: 1.10, 95% CI: 0.95–1.40, P = 0.336) (see Table 2). Subgroup analysis classified by age showed only a significant association between sleep duration, sleep quality and stroke for participants aged >46 years (Tables 3 and 4).
Sleep quality interacted with sleep duration on risk of stroke
The results from the multiple logistic regression models were showed in Table 5. Individuals with poor sleep quality combined short sleep duration significantly increased risk of stroke compared with those with good sleep quality combined sleep duration 6–8 h (RR: 1.39, 95% CI: 1.13–1.70 and RR: 1.35, 95% CI: 1.09–1.67, respectively, P < 0.001).
The risk of stroke was greatest in those with poor sleep quality combined short sleep duration (RR: 6.75, 95% CI: 2.45–14.12, P < 0.001). In addition, subjects with long sleep duration and good sleep quality had no increased risk of stroke compared with those who had good sleep quality and sleep duration of 6–8 h (RR: 1.23, 95% CI: 0.95–1.34, P = 0. 257). Those with both poor sleep quality and long sleep duration had higher risk of being stroke (RR: 2.77, 95% CI: 1.41–7.99, P < 0.001) compared with those with sleep duration of 6–8 h.
Sensitivity analysis
There was a strong additive interaction between sleep quality and sleep duration on stroke, with 72% of stroke events attributed to the interaction between poor sleep quality and short sleep duration and 35% attributed to the interaction between poor sleep quality and long sleep duration(Table 6).
Discussion
Our study showed that poor sleep quality and sleep duration (<6 h/d or >8 h/d) increased the risk of being stroke independent of the potential confounders in a Chinese population. This association was only found in participants aged >45 years, not in those aged 18–45 years. Sex differences showed that women had a slightly stronger relationship between sleep duration of <6 h/d and stroke than men, while men had a slightly stronger relationship between. In addition, there was also an interactive effect of long sleep duration and poor sleep quality on stroke. The findings suggest that sleep quality and quantity should be included in the evaluation of stroke risks and development of prevention methods and interventions.
Many studies indicated that both short and long sleep duration increased risk of stroke7,26,27,28,29, consistent with our study. Eguchi et al. conducted a multivariable Cox regression analysis with 1,268 hypertensive patients and found that sleep duration less than 7.5 h/d was independently associated with stroke risk (hazard ratio = 2.21; P = 0.003)26. One systematic review analyzed with 474,684 participants from 15 studies (24 cohort samples) and suggested that short sleep duration was positively related with risk of developing stroke (relative risk: 1.15, 95% CI: 1.00–1.31, P = 0.047)27. A 8-year cohort study including 23,620 participants found that risk of stroke increased 2.06 times (95% CI: 1.18–3.59) in those with sleep duration <6 h/d compared with those with duration 7-8 h/d28. A meta-analysis by Ge and Guo with 12 cohort studies reported a hazard ratio for stroke risk of 1.13 (95% CI: 1.02–1.25) in individuals having short sleep duration7. Results from a meta-analysis included six cross-sectional studies showed an pooled odds ratio of 1.71 (95% CI: 1.39–2.02) for individuals with short sleep duration developing stroke7. Li et al. reported a pooled relative risks by 7% per hour of sleep reduction for stroke events were among individuals having sleep duration <7 h/d29. Furthermore, our findings showed a U- shaped association between sleep duration and risk of stroke, consistent with previous report30. However, there was difference by sex and age. The risk of being stroke seemed slightly higher in female with short sleep duration, and in male with long sleep duration. Both short and long sleep duration were associated with stroke in participants aged 46-80 years, while this association was not found younger ones, consistent with a 10-year cohort study report31. The results suggest that flexibility to insufficient sleep or vulnerability to prolonged sleep as risk factors for stroke may differ by age.
Our study also found risk of stroke in relation with poor sleep quality, and men had a slightly stronger relationship than women. Zhang et al. Reported14 an odds ratio of 1.811 (95% CI: 1.116–2.939) for being stroke among poor-quality sleepers aged 18–45 years compared with good-quality sleepers. Conversely we found the association only occurring in the age over 46 years, which may be partly due to higher risk of carotid intima-media thickness in relation with poor sleep quality in stroke-free individuals aged ≥40 years32.
Short sleep duration may increase cortisol levels via activation of sympathetic activity and hypothalamic–pituitary–adrenal axis33,34, which can further result in hypertension and harm brain tissue, and accelerate the development of stroke. Short sleep duration also results in insulin resistance, which alters vascular endothelial function, causes abnormal fibrinolysis and systemic inflammation, and elevates high-sensitivity C-reactive protein levelsand hypercoagulability35,36,37,38, which tends to promote atherosclerosis and subsequent stroke35,39,40.
Poor sleep quality is related to impaired glucose tolerance and insulin sensitivity, and increased interleukin 6 level, and plasma concentration41,42,43, which increases the risk of stroke.
Consistent with previous reports, the current study showed an association between stroke and long sleep duration. Cappuccio and colleagues systematically analyzed 15 studies including 474,684 participants and had a result of positive relationship between long sleep durationand risk of stroke with odds ratio of 1.65 (95% CI: 1.45–1.87, P < 0.0001)26. A 10-year cohort study including 7,844 adults showed a greater risk of stroke in persons with sleep duration >8 h per night than those with duration of 6–8 h per night (relative risk: 1.5, 95% CI: 1.1–2.0)31 A 7.5-year prospective study found a positive association between long sleep duration and ischemic stroke in 93,175 women aged 50–79 years44. Similar results were also reported by a prospective study including 9,692 stroke-free participants aged 42–81 years long sleep duration was significantly associated with an increased risk of stroke with a hazard ratio of 1.46(95% CI: 1.08–1.98) for being stroke in long-time sleepers45. Meta-analyzed results from the 12 cohort and 6 cross-sectional studies showed t a hazard ratio of 1·40(95% CI: 1.16–1.64) and odds ratio of 2.12 (95% CI: 1.51–2.73), respectively, for risk of stroke in individuals with long sleep duration7. Another meta-analysis of 11 studies showed a pooled relative risk of increased 17% per hour of sleep increment in those having sleep duration >7 h/d compared with those with 7 h/d29.
Sleep duration more than 8 hour is reported association with elevated blood C-reactive protein, interleukin 6, fibrinogen, and total leukocyte numbers, and decreased albumin levels, compared with sleep duration of 6–8 h46,47,48,49. Increases in inflammatory markers can damage blood sugar stability and β-cell function, leading to insulin resistance and the development of stroke. Taken together, the evidence shows that long sleep duration increases inflammatory cytokines and insulin resistance, and poor sleep quality also increases inflammatory cytokines and decreases insulin sensitivity; these factors all increase stroke risk.
Some main traditional modifiable risk factors are prevalent in China. For example, the incidence of hypertension is as high as 32.5%50, the incidence of diabetes is 11.6%51, and the prevalence of smoking is 28.3%52. As a relatively new modifiable risk factor, the prevalence of sleep disorders is 41.5%33. Therefore, the government and general practitioners should seriously consider both traditional and new modifiable risk factors in the development of stroke prevention methods and interventions. Given the difficulties of screening and treating stroke patients, recommendations to improve sleep quality and sleep duration are inexpensive and practical means of decreasing risk of stroke.
Our study has some limitations. Firstly, information on sleep quality and duration was self-reported, information bias may be inevitable. Secondly, we did not include clinical diagnoses for sleep disorders. Thirdly, other confounders associated with sleep disorders, such as depression and general health53, were not measured. Fourthly, our findings were derived from Chinese subjects which may not be generalized to other ethnic populations. Fifthly, lost-to-follow-up participants were older, and had poor sleep quality and short or long sleep duration, which may reduce the strength of the associations. Sixth, recreational drug use was not collected, which might be small affect on the relationship of sleep quality and stroke.
In summary, poor sleep quality and short/long sleep duration increase the risk of being stroke. Moreover, there is an interactive effect of poor sleep quality and short sleep duration on increased risk of stroke. As inappropriate sleep duration and poor sleep quality are common in Chinese adults, appropriate identification and treatment of sleep disturbances is very important to prevent the development of stroke. In the further, We would analyze the association between the specific sleep disorders, sleep patterns, environmental, behavioral and medical comorbid risk factors and stroke, and added the evidence of the relationship between sleep and stroke.
Ethics approval and consent to participate
The study protocol was approved by the Xuzhou Center for Disease Control and Prevention, and conducted in accordance with the principles of the Declaration of Helsinki (1975, revised 2000). All participants provided written informed consent.
Data availability
All data relevant to the given manuscript have been stored in a separate file that can be made freely available to external investigators upon request.
References
GBD. 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388(10053), 1459–1544 (2016).
Feigin, V. L. et al. Global Burden of Diseases, Injuries, and Risk Factors Study 2010 (GBD 2010) and the GBD Stroke Experts Group.Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 383(9913), 245–54 (2014).
Wang, W. et al. Prevalence, Incidence and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480,687 Adults. Circulation 135(8), 759–771 (2017).
Ning, X. et al. Increased Stroke Burdens Among the Low-Income Young and Middle Aged in Rural China. Stroke 48(1), 77–83 (2017).
Kim, Y. D., Jung, Y. H. & Saposnik, G. Traditional Risk Factors for Stroke in East Asia. J. Stroke 18(3), 273–285 (2016).
Patyar, S. & Patyar, R. R. Correlation between Sleep Duration and Risk of Stroke. J. Stroke Cerebrovasc. Dis. 24(5), 905–11 (2015).
Ge, B. & Guo, X. Short and long sleep durations are both associated with increased risk of stroke: a meta-analysis of observational studies. Int. J. Stroke 10(2), 177–84 (2015).
Mims, K. N. & Kirsch, D. Sleep and Stroke. Sleep. Med. Clin. 11(1), 39–51 (2016).
Ruiter Petrov, M. E., Letter, A. J., Howard, V. J. & Kleindorfer, D. Self-reported sleep duration in relation to incident stroke symptoms: nuances by body mass and race from the REGARDS study. J. Stroke Cerebrovasc. Dis. 23, e123–32 (2014).
Westerlund, A. et al. Sleep characteristics and cardiovascular events in a large Swedish cohort. Eur. J. Epidemiol. 28, 463–73 (2013).
Petrov, M. E. et al. Sleep duration and risk of incident stroke by age, sex, and race: The REGARDS study. Neurology 91(18), e1702–e1709 (2018).
Zhang, H. S. et al. Sleep quality and health service utilization in Chinese general population: a cross-sectional study in Dongguan, China. Sleep. Med. 27-28, 9–14 (2016).
Huang, W. S. et al. Nonapnea sleep disorders are associated with subsequent ischemic stroke risk: a nationwide, population-based, retrospective cohort study. Sleep. Med. 14(12), 1341–7 (2013).
Zhang, S. et al. Correlation analysis of sleep quality and youth ischemic stroke. Behav. Neurol. 2014, 246841 (2014).
Liu, M. et al. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol. 6(5), 456–64 (2007).
Buysse, D. J., Reynolds, C. F. III, Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 28(2), 193–213 (1989).
Tsai, P. S. et al. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual. Life Res. 14(8), 1943–52 (2005).
Sacco, R. L. et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44, 2064–89 (2013).
Zhou, B. F. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Env. Sci. 15, 83–96 (2002).
Chinese Diabetes Society. Chinese guidelines for the prevention and treatment of type 2 diabetes mellitus Chinese Journal of Diabetes, 2012;20(1): 1-36 (2010 Edition).
China hypertension prevention guidelines revision committee. Guidelines for prevention and treatment of hypertension in China[2010 Edition]. Chin. J. hypertension 1919(8), 701–743 (2011).
Chung, F. et al. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br. J. Anaesth. 108(5), 768–775 (2012).
Anderss, T., Alfredss, L., Källberg, H., Zdravkovic, S. & Ahlbom, A. Calculating measures of biological interaction. Eur. J. Epidemiol. 20, 575–579 (2005).
Knol, M. J., van der Tweel, I., Grobbee, D. E., Numans, M. E. & Geerlings, M. I. Estimating interaction on an additive scale between continuous determinants in a logistic regression model. Int. J. Epidemiol. 36(5), 1111–8 (2007).
Knol, M. J. et al. Estimating measures of interaction on an additive scale for preventive exposures. Eur. J. Epidemiol. 26(6), 433–438 (2011).
Eguchi, K., Hoshide, S., Ishikawa, S., Shimada, K. & Kario, K. Short sleep duration is an independent predictor of stroke events in elderly hypertensive patients. J. Am. Soc. Hypertens. 4, 255–62 (2010).
Cappuccio, F. P., Cooper, D., D’Elia, L., Strazzullo, P. & Miller, M. A. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur. Heart J. 32(12), 1484–92 (2011).
von Ruesten, A., Weikert, C., Fietze, I. & Boeing, H. Association of sleep duration with chronic diseases in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam study. PLoS One 7(1), e30972 (2012).
Li, W. et al. Sleep duration and risk of stroke events and stroke mortality: A systematic review and meta-analysis of prospective cohort studies. Int. J. Cardiol. 223, 870–876 (2016).
Yin, J. et al. Relationship of Sleep Duration With All-Cause Mortality and Cardiovascular Events: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. J. Am. Heart Assoc. 6(9), e005947 (2017).
Qureshi, A. I., Giles, W. H., Croft, J. B. & Bliwise, D. L. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10-year follow-up from NHANES I. Neurology 48(4), 904–11 (1997).
Del Brutto, O. H. et al. Sleep quality correlates with the carotid intima-media thickness in stroke-free community-dwelling adults living in rural Ecuador. The Atahualpa Project. Sleep. Med. 55, 22–25 (2019).
Vgontzas, A. N., Liao, D., Bixler, E. O., Chrousos, G. P. & Vela-Bueno, A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep 32, 491–7 (2009).
Spiegel, K., Leproult, R. & Van Cauter, E. Impact of sleep debt on metabolic and endocrine function. Lancet 354(9188), 1435–9 (1999).
Kernan, W. N. et al. Insulin resistance and risk for stroke. Neurology. 59, 809–815 (2002).
Mercurio, V., Carlomagno, G., Fazio, V. & Fazio, S. Insulin resistance: is it time for primary prevention? World J. Cardiol. 4, 1–7 (2012).
Sourij, H. et al. Insulin resistance as a risk factor for carotid atherosclerosis: a comparison of the Homeostasis Model Assessment and the short insulin tolerance test. Stroke 39, 1349–1351 (2008).
Chiang, J. K. Short Duration of Sleep Is Associated with Elevated High-Sensitivity C-Reactive Protein Level in Taiwanese Adults: A Cross-Sectional Study. J. Clin. Sleep. Med. 10(7), 743–9 (2014).
Howard, G. et al. Racial differences in the association of insulin resistance with stroke risk: the Reasons for Geographic And Racial Differences in Stroke (REGARDS) study. Stroke 45, 2257–2262 (2014).
Thacker, E. L. et al. Fasting and post-glucose load measures of insulin resistance and risk of ischemic stroke in older adults. Stroke 42, 3347–3351 (2011).
Depner, C. M., Stothard, E. R. & Wright, K. P. Jr Metabolic consequences of sleep and circadian disorders. Curr. Diab Rep. 14(7), 507 (2014).
Stamatakis, K. A. & Punjabi, N. M. Effects of sleep fragmentation on glucose metabolism in normal subjects. Chest 137, 95–101 (2010).
Friedman, E. M. Sleep quality, social well-being, gender, and inflammation: an integrative analysis in a national sample. Ann. N. Y. Acad. Sci. 1231, 23–34 (2011).
Chen, J. C. et al. Sleep duration and risk of ischemic stroke in postmenopausal women. Stroke 39(12), 3185–92 (2008).
Leng, Y. et al. Sleep duration and risk of fatal and nonfatal stroke: a prospective study and meta-analysis. Neurology 84(11), 1072–9 (2015).
Dowd, B., Goldman, N. & Weinstein, M. Sleep duration, sleep quality, and biomarkers of inflammation in a Taiwanese population. Ann. Epidemiol. 21, 799–806 (2011).
Grandner, M. A., Sands-Lincoln, M. R., Pak, V. M. & Garland, S. N. Sleep duration, cardiovascular disease, and proinflammatory biomarkers. Nat. Sci. Sleep. 5, 93–107 (2013).
Patel, S. R. et al. Sleep duration and biomarkers of inflammation. Sleep 32(2), 200–4 (2009).
Grandner, M. A. et al. Extreme sleep durations and increased C-reactive protein: effects of sex and ethnoracial group. Sleep 36(5), 769–779E (2013).
Lewington, S. et al. The Burden of Hypertension and Associated Risk for Cardiovascular Mortality in China. JAMA Intern. Med. 176(4), 524–32 (2016).
Xu, Y. et al. Prevalence and Control of Diabetes in Chinese Adults. JAMA 310(9), 948–59 (2013).
Ding, L. et al. Smoking and Its Relation to Metabolic Status among Chinese Adults: Analysis of a Nationwide Survey. Biomed. Env. Sci. 29(9), 619–627 (2016).
Stranges, S. et al. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am. J. Epidemiol. 168(12), 1353–64 (2008).
Acknowledgements
We thank all the participants involved in the survey. We thank the Regional Centers for Disease Control and Prevention as well as the clinics in Xuzhou city for their collaboration. We thank Diane Williams, PhD, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript. This research was funded by the Science and Technology projects of Xuzhou city in 2015 (KC15SM046). The study funders had no influence on the study design, data collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
A.L.J. wrote/edited the manuscript and created the tables. H.Q.L., P.A.L., C.X., P.Z., C.Q. and Q.Y. contributed to the discussion and reviewed/edited the manuscript. A.L.J. conceptualized the study. P.A.L. is the guarantor of this work and, as such, had full access to all the study data and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ji, A., Lou, H., Lou, P. et al. Interactive effect of sleep duration and sleep quality on risk of stroke: An 8-year follow-up study in China. Sci Rep 10, 8690 (2020). https://doi.org/10.1038/s41598-020-65611-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-65611-y
This article is cited by
-
Prevalence and determinants of depressive symptoms among community-dwelling older adults in China based on differences in living arrangements: a cross-sectional study
BMC Geriatrics (2023)
-
The independent and combined association of napping and night sleep duration with stroke in Chinese rural adults
Sleep and Breathing (2023)
-
Sleep and Stroke: Opening Our Eyes to Current Knowledge of a Key Relationship
Current Neurology and Neuroscience Reports (2022)
-
Factors associated with stroke among patients with type 2 diabetes mellitus in China: a propensity score matched study
Acta Diabetologica (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.