Abstract
The objective of this study was to explore different internal flow passages in the patient interface region of a new air-jet–based dry powder inhaler (DPI) in order to minimize device and extrathoracic aerosol depositional losses using computational fluid dynamics (CFD) simulations. The best-performing flow passages were used for oral and nose-to-lung (N2L) aerosol delivery in pediatric extrathoracic airway geometries consistent with a 5-year-old child. Aerosol delivery conditions were based on a previously developed and tested air-jet DPI device and included a base flow rate of 13.3 LPM (delivered from a small ventilation bag) and an inhaled air volume of 750 mL. Initial CFD models of the system clearly established that deposition on either the back of the throat or nasal cannula bifurcation was strongly correlated with the maximum velocity exiting the flow passage. Of all designs tested, the combination of a 3D rod array and rapid expansion of the flow passage side walls was found to dramatically reduce interface and device deposition and improve lung delivery of the aerosol. For oral aerosol administration, the optimal flow passage compared with a base case reduced device, mouthpiece, and mouth-throat deposition efficiencies by factors of 8-, 3-, and 2-fold, respectively. For N2L aerosol administration, the optimal flow pathway compared with a base case reduced device, nasal cannula, and nose-throat deposition by 16-, 6-, and 1.3-fold, respectively. In conclusion, a new patient interface design including a 3D rod array and rapid expansion dramatically improved transmission efficiency of a dry powder aerosol.












Similar content being viewed by others
References
Somayaji R, Parkins MD. Tobramycin inhalation powder: an efficient and efficacious therapy for the treatment of Pseudomonas aeruginosa infection in cystic fibrosis. Ther Deliv. 2015;6(2):121–37.
Below A, Bickmann D, Breitkreutz J. Assessing the performance of two dry powder inhalers in preschool children using an idealized pediatric upper airway model. Int J Pharm. 2013;444(1–2):169–74.
Lindert S, Below A, Breitkreutz J. Performance of dry powder inhalers with single dosed capsules in preschool children and adults using improved upper airway models. Pharmaceutics. 2014;6:36–51.
Lexmond AJ, Hagedoorn P, Frijlink HW, Rottier BL, de Boer AH. Prerequisites for a dry powder inhaler for children with cystic fibrosis. PLoS One. 2017;12(8):e0183130.
Lexmond AJ, Kruizinga TJ, Hagedoorn P, Rottier BL, Frijlink HW, De Boer AH. Effect of inhaler design variables on paediatric use of dry powder inhalers. PLoS One. 2014;9(6):e99304.
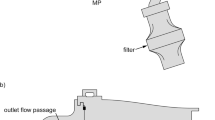
Farkas D, Hindle M, Bass K, Longest PW. Development of an inline dry powder inhaler for oral or trans-nasal aerosol administration to children. J Aerosol Med Pulm Drug Deliv. 2019.
Longest PW, Farkas D. Development of a new inhaler for high-efficiency dispersion of spray-dried powders using computational fluid dynamics (CFD) modeling. AAPS J. 2018. https://doi.org/10.1208/s12248-018-0281-y.
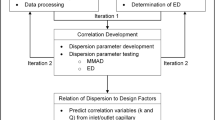
Longest PW, Farkas D, Bass K, Hindle M. Use of computational fluid dynamics (CFD) dispersion parameters in the development of a new DPI actuated with low air volumes. Pharm Res. 2019;36(8).
Bass K, Farkas D, Longest PW. Optimizing aerosolization using computational fluid dynamics in a pediatric air-jet dry powder inhaler. AAPS PharmSciTech. 2019;20(8).
Hindle M, Longest PW. Quantitative analysis and design of a spray aerosol inhaler. Part 2: improvements in mouthpiece performance. JAerosol Med Pulm Drug Deliv. 2013;26(5):237–47.
Farkas D, Hindle M, Longest PW. Application of an inline dry powder inhaler to deliver high dose pharmaceutical aerosols during low flow nasal cannula therapy. Int J Pharm. 2018;546(1–2):1–9.
Farkas D, Hindle M, Longest PW. Efficient nose-to-lung aerosol delivery with an inline dpi requiring low actuation air volume. Pharm Res. 2018;35(10).
Coates MS, Chan H-K, Fletcher DF, Chiou H. Influence of mouthpiece geometry on the aerosol delivery performance of a dry powder inhalation. Pharm Res. 2007;24(8):1450–6.
Coates MS, Fletcher DF, Chan H-K, Raper JA. Effect of design on the performance of a dry powder inhaler using computational fluid dynamics. Part 1: grid structure and mouthpiece length. J Pharm Sci-Us. 2004;93(11):2863–76.
Behara SRB, Longest PW, Farkas DR, Hindle M. Development of high efficiency ventilation bag actuated dry powder inhalers. Int J Pharm. 2014;465(1–2):52–62.
Behara SRB, Longest PW, Farkas DR, Hindle M. Development and comparison of new high-efficiency dry powder inhalers for carrier-free formulations. J Pharm Sci-US. 2014;103(2):465–77.
Longest PW, Golshahi L, Behara SRB, Tian G, Farkas DR, Hindle M. Efficient nose-to-lung (N2L) aerosol delivery with a dry powder inhaler. J Aerosol Med Pulm Drug Deliv. 2015;28(3):189–201.
Longest PW, Son Y-J, Holbrook LT, Hindle M. Aerodynamic factors responsible for the deaggregation of carrier-free drug powders to form micrometer and submicrometer aerosols. Pharm Res. 2013;30:1608–27.
Bass K, Boc S, Hindle M, Dodson K, Longest PW. High-efficiency nose-to-lung aerosol delivery in an infant: development of a validated computational fluid dynamics method. J Aerosol Med Pulm Drug Deliv. 2019. https://doi.org/10.1089/jamp.2018.1490.
Bass K, Longest PW. Recommendations for simulating microparticle deposition at conditions similar to the upper airways with two-equation turbulence models. J Aerosol Sci. 2018.
Longest PW, Vinchurkar S. Validating CFD predictions of respiratory aerosol deposition: effects of upstream transition and turbulence. J Biomech. 2007;40(2):305–16.
Delvadia R, Longest PW, Byron PR. In vitro tests for aerosol deposition. I. Scaling a physical model of the upper airways to predict drug deposition variation in normal humans. J Aerosol Med. 2012;25(1):32–40.
Wei X, Hindle M, Kaviratna A, Huynh BK, Delvadia RR, Sandell D, et al. In vitro tests for aerosol deposition. VI: realistic testing with different mouth–throat models and in vitro—in vivo correlations for a dry powder inhaler, metered dose inhaler, and soft mist inhaler. J Aerosol Med Pulm Drug Deliv. 2018.
Roache PJ. Perspective: a method for uniform reporting of grid refinement studies. J Fluid Eng Trans ASME. 1994;116(3):405–13.
Longest PW, Hindle M, Das Choudhuri S, Byron PR. Numerical simulations of capillary aerosol generation: CFD model development and comparisons with experimental data. Aerosol Sci Technol. 2007;41(10):952–73.
Longest PW, Vinchurkar S, Martonen TB. Transport and deposition of respiratory aerosols in models of childhood asthma. J Aerosol Sci. 2006;37:1234–57.
Longest PW, Xi J. Effectiveness of direct Lagrangian tracking models for simulating nanoparticle deposition in the upper airways. Aerosol Sci Technol. 2007;41(4):380–97.
Walenga RL, Longest PW. Current inhalers deliver very small doses to the lower tracheobronchial airways: assessment of healthy and constricted lungs. J Pharm Sci. 2016;105:147–59.
Matida EA, Finlay WH, Grgic LB. Improved numerical simulation of aerosol deposition in an idealized mouth-throat. J Aerosol Sci. 2004;35:1–19.
Wang Y, James PW. On the effect of anisotropy on the turbulent dispersion and deposition of small particles. Int J Multiphase Flow. 1999;22:551–8.
Tian G, Hindle M, Lee S, Longest PW. Validating CFD predictions of pharmaceutical aerosol deposition with in vivo data. Pharm Res. 2015;32:3170–87.
White FM. Viscous fluid flow. 3rd ed. New York: McGraw-Hill Higher Education; 2006. xxi, 629 pages p
Longest PW, Vinchurkar S. Effects of mesh style and grid convergence on particle deposition in bifurcating airway models with comparisons to experimental data. Med Eng Phys. 2007;29(3):350–66.
Golshahi L, Noga ML, Thompson RB, Finlay WH. In vitro deposition measurement of inhaled micrometer-sized particle in extrathoracic airways of children and adolescents during nose breathing. J Aerosol Sci. 2011;42:474–88.
Javaheri E, Golshahi L, Finlay W. An idealized geometry that mimics average infant nasal airway deposition. J Aerosol Sci. 2013;55:137–48.
Storey-Bishoff J, Noga M, Finlay WH. Deposition of micrometer-sized aerosol particles in infant nasal airway replicas. Aerosol Sci. 2008;39:1055–65.
Tavernini S, Church TK, Lewis DA, Noga M, Martin AR, Finlay WH. Deposition of micrometer-sized aerosol particles in neonatal nasal airway replicas. Aerosol Sci Technol. 2018;52(4):407–19.
Hansen SK, Rau MH, Johansen HK, Ciofu O, Jelsbak L, Yang L, et al. Evolution and diversification of Pseudomonas aeruginosa in the paranasal sinuses of cystic fibrosis children have implications for chronic lung infection. ISME J. 2012;6(1):31–45.
Linnane B, Kearse L, O'Connell NH, Fenton J, Kiernan MG, Dunne CP. A case of failed eradication of cystic fibrosis-related sinus colonisation by Pseudomonas aeruginosa. BMC Pulm Med. 2015;15.
Moller ME, Alanin MC, Gronhoj C, Aanaes K, Hoiby N, von Buchwald C. Sinus bacteriology in patients with cystic fibrosis or primary ciliary dyskinesia: a systematic review. Am J Rhinol Allergy. 2017;31(5):293–8.
Walenga RL, Tian G, Hindle M, Yelverton J, Dodson K, Longest PW. Variability in nose-to-lung aerosol delivery. J Aerosol Sci. 2014;78:11–29.
Acknowledgments
Dr. Dale Farkas is gratefully acknowledged for helpful discussions and input related to the development of the air-jet DPI, patient interface devices, and pediatric airway models. Spray-dried powder from the VCU Department of Pharmaceutics (Hindle Lab) generated by Serena Bonasera and experimental lab access are also gratefully acknowledged. Finally, the authors wish to thank Dr. Michael Hindle for helpful insights and guidance in support of this work.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R01HD087339 and by the National Heart, Lung and Blood Institute of the National Institutes of Health under Award Number R01HL139673.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Virginia Commonwealth University is currently pursuing patent protection of EEG aerosol delivery, DPI aerosol generation devices and patient interfaces, which if licensed, may provide a future financial interest to the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bass, K., Longest, W. Development of Dry Powder Inhaler Patient Interfaces for Improved Aerosol Delivery to Children. AAPS PharmSciTech 21, 157 (2020). https://doi.org/10.1208/s12249-020-01667-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-020-01667-3