Abstract
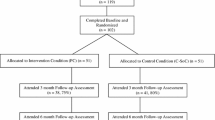
Personalized cognitive counseling (PCC) is an evidence-based intervention designed to modify HIV-related risk behavior. We assessed the impact of PCC on sexual behavior, drinking expectancy, and incidence of sexually transmitted infections (STIs) in a 6-month randomized controlled trial among 153 HIV-uninfected men who have sex with men (MSM) and transgender women (TW) in Peru. Study retention was ≥ 90%, with three HIV infections (3 Control) and 19 cases of GC/CT (10 Control, 9 PCC) at 6 months. There was a decline in condomless receptive anal intercourse in the Control (0.74, 95% CI 0.60–0.91; p < 0.01) and PCC arms (0.72, 0.55–0.94; p = 0.02) at 6-month follow-up. There was a decrease in drinking expectancy at 6 months among participants endorsing alcohol use in the PCC arm (0.89, 0.83–0.96; p < 0.01), versus no change in the Control arm (0.98, 0.92–1.04; p = 0.54). PCC was efficacious in reducing drinking expectancy and HIV risk among MSM and TW in Peru.
Resumen
La consejería cognitiva personalizada (CCP) es una intervención basada en evidencia diseñada para poder modificar el comportamiento asociado con el riesgo de contraer VIH. Evaluamos el impacto de CCP en el compartimiento sexual, el drinking expectancy, y la incidencia de infecciones de transmisión sexual (ITS) a través de un estudio controlado aleatorio que duró seis meses e incluyó 153 hombres sin VIH que tienen relaciones sexuales con hombres (HSH) y mujeres transgéneros (MT) en Perú. La retención en el estudio fue ≥90%, con tres infecciones de VIH (3 Control) y 19 casos de GC/CT (10 Control, 9 CCP) a los seis meses. Hubo una disminución de las relaciones sexuales receptivas sin preservativos dentro del grupo Control (0.74, 95% CI: 0.60-0.91; p<0.01) y el grupo CCP (0.72, 0.55-0.94; p=0.02) a los seis meses. También hubo una disminución en el drinking expectancy a los seis meses dentro de los participantes quienes tomaban alcohol dentro del grupo CCP (0.89, 0.83-0.96; p<0.01), versus ningún cambio dentro del grupo Control (0.98, 0.92-1.04; p=0.54). La CCP fue eficaz en disminuir el drinking expectancy y el riesgo de contraer VIH dentro de HSH y MT en Perú.



Similar content being viewed by others
References
CDC. Compendium of Evidence-Based Interventions and Best Practices for HIV Prevention: Personalized Cognitive Counseling. Centers for Disease Control and Prevention; 2018.
Dilley JW, Woods WJ, Sabatino J, Lihatsh T, Adler B, Casey S, et al. Changing sexual behavior among gay male repeat testers for HIV: a randomized, controlled trial of a single-session intervention. J Acquir Immune Defic Syndr. 2002;30(2):177–86.
Gold RS. AIDS education for gay men: towards a more cognitive approach. AIDS Care. 2000;12(3):267–72.
Nelson KM, Simoni JM, Pearson CR, Walters KL. 'I've had unsafe sex so many times why bother being safe now?': the role of cognitions in sexual risk among American Indian/Alaska Native men who have sex with men. Ann Behav Med. 2011;42(3):370–80.
Shah D, Thornton S, Burgess AP. Sexual Risk Cognitions Questionnaire: a reliability and validity study. AIDS Care. 1997;9(4):471–80.
Coffin PO, Santos GM, Colfax G, Das M, Matheson T, DeMicco E, et al. Adapted personalized cognitive counseling for episodic substance-using men who have sex with men: a randomized controlled trial. AIDS Behav. 2014;18(7):1390–400.
McPhee B, Skinta MD, Paul J, Dilley JW. Single-session personalized cognitive counseling to change HIV risk behavior among HIV-negative men who have sex with men: a two-part case study. Cognit Behav Pract. 2012;19:328–37.
Dilley JW, Woods WJ, Loeb L, Nelson K, Sheon N, Mullan J, et al. Brief cognitive counseling with HIV testing to reduce sexual risk among men who have sex with men: results from a randomized controlled trial using paraprofessional counselors. J Acquir Immune Defic Syndr. 2007;44(5):569–77.
Santos GM, Coffin PO, Vittinghoff E, DeMicco E, Das M, Matheson T, et al. Substance use and drinking outcomes in Personalized Cognitive Counseling randomized trial for episodic substance-using men who have sex with men. Drug Alcohol Depend. 2014;138:234–9.
Knight KR, Das M, DeMicco E, Raiford JL, Matheson T, Shook A, et al. A roadmap for adapting an evidence-based HIV prevention intervention: personal cognitive counseling (PCC) for episodic substance-using men who have sex with men. Prev Sci. 2014;15(3):364–75.
Herbst JH, Raiford JL, Carry MG, Wilkes AL, Ellington RD, Whittier DK. Adaptation and national dissemination of a brief, evidence-based, HIV prevention intervention for high-risk men who have sex with men. MMWR Suppl. 2016;65(1):42–50.
Wiersema JJ, Santella AJ, Canady P, Jordan AO. Self-justifications for unsafe sex among incarcerated young men who have sex with men and are living with HIV: results from a New York City jail-based pilot intervention. J Commun Health. 2019;44:729–39.
Dilley JW, Schwarcz S, Murphy J, Joseph C, Vittinghoff E, Scheer S. Efficacy of personalized cognitive counseling in men of color who have sex with men: secondary data analysis from a controlled intervention trial. AIDS Behav. 2011;15(5):970–5.
Irwin TW, Morgenstern J. Drug-use patterns among men who have sex with men presenting for alcohol treatment: differences in ethnic and sexual identity. J Urban Health. 2005;82(1 Suppl 1):i127–i133133.
Stall R, Wiley J. A comparison of alcohol and drug use patterns of homosexual and heterosexual men: the San Francisco Men's Health Study. Drug Alcohol Depend. 1988;22(1–2):63–73.
Balán IC, Frasca T, Pando MA, Marone RO, Barreda V, Dolezal C, Carballo-Diéguez A, Ávila MM. High substance use and HIV risk behavior among young Argentine men who have sex with men. AIDS Behav. 2018;22(4):1373–82.
Tomkins A, Ahmad S, Cannon L, Higgins SP, Kliner M, Kolyva A, et al. Prevalence of recreational drug use reported by men who have sex with men attending sexual health clinics in Manchester, UK. Int J STD AIDS. 2018;29(4):350–6.
Sabin LL, Beard J, Agyarko-Poku T, DeSilva M, Ashigbie P, Segal T, et al. "Too much sex and alcohol": beliefs, attitudes, and behaviors of male adolescents and young men who have sex with men in Ghana. Open AIDS J. 2018;12:69–80.
Pham QD, Nguyen TV, Nguyen PD, Le SH, Tran AT, Nguyen LT, et al. Men who have sex with men in southern Vietnam report high levels of substance use and sexual risk behaviours but underutilise HIV testing services: a cross-sectional study. Sex Transm Infect. 2015;91(3):178–82.
Hunter LJ, Dargan PI, Benzie A, White JA, Wood DM. Recreational drug use in men who have sex with men (MSM) attending UK sexual health services is significantly higher than in non-MSM. Postgrad Med J. 2014;90(1061):133–8.
Secor AM, Wahome E, Micheni M, Rao D, Simoni JM, Sanders EJ, et al. Depression, substance abuse and stigma among men who have sex with men in coastal Kenya. AIDS (London, England). 2015;29(Suppl 3):S251–S259259.
Drumright LN, Little SJ, Strathdee SA, Slymen DJ, Araneta MR, Malcarne VL, et al. Unprotected anal intercourse and substance use among men who have sex with men with recent HIV infection. J Acquir Immune Defic Syndr. 2006;43(3):344–50.
Colfax G, Coates TJ, Husnik MJ, Huang Y, Buchbinder S, Koblin B, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of san francisco men who have sex with men. J Urban Health. 2005;82(1 Suppl 1):i62–70.
Colfax G, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B, et al. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. Am J Epidemiol. 2004;159(10):1002–12.
Deiss RG, Clark JL, Konda KA, Leon SR, Klausner JD, Caceres CF, et al. Problem drinking is associated with increased prevalence of sexual risk behaviors among men who have sex with men (MSM) in Lima. Peru Drug Alcohol Depend. 2013;132(1–2):134–9.
Herrera MC, Konda KA, Leon SR, Deiss R, Brown B, Calvo GM, et al. Impact of alcohol use on sexual behavior among men who have sex with men and transgender women in Lima, Peru. Drug Alcohol Depend. 2016;161:147–54.
Vagenas P, Lama JR, Ludford KT, Gonzales P, Sanchez J, Altice FL. A systematic review of alcohol use and sexual risk-taking in Latin America. Rev Panam Salud Publica. 2013;34(4):267–74.
Herrera MC, Konda KA, Leon SR, Brown B, Calvo GM, Salvatierra HJ, et al. Do subjective alcohol screening tools correlate with biomarkers among high-risk transgender women and men who have sex with men in Lima, Peru? AIDS Behav. 2017;21(Suppl 2):253–61.
Deiss RG, Clark JL, Konda KA, Leon SR, Klausner JD, Caceres CF, et al. Problem drinking is associated with increased prevalence of sexual risk behaviors among men who have sex with men (MSM) in Lima, Peru. Drug Alcohol Depend. 2013;132(1–2):134–9.
Ludford KT, Vagenas P, Lama JR, Peinado J, Gonzales P, Leiva R, et al. Screening for drug and alcohol use disorders and their association with HIV-related sexual risk behaviors among men who have sex with men in Peru. PLoS ONE. 2013;8(8):e69966.
Vagenas P, Ludford K, Gonzales P. Being unaware of being HIV-infected is associated with alcohol use disorders and high-risk sexual behaviors among men who have sex with men in Peru. AIDS Behav. 2014;18:120–7.
UNAIDS. UNAIDS Data 2017: Peru Joint United Nations Programme on HIV/AIDS 2017.
Vagenas P, Wickersham JA, Calabrese SK, Lama JR, Benites CM, Pun M, et al. Validation of the 'drinking expectancy questionnaire for men who have sex with men' in Peru. Drug Alcohol Rev. 2015;34:759.
Mullens AB, Young RM, Dunne MP, Norton G. The Drinking Expectancy Questionnaire for Men who have Sex with Men (DEQ-MSM): a measure of substance-related beliefs. Drug Alcohol Rev. 2011;30(4):372–80.
Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(3):1–138.
Metcalf CA, Douglas JM Jr, Malotte CK, Cross H, Dillon BA, Paul SM, et al. Relative efficacy of prevention counseling with rapid and standard HIV testing: a randomized, controlled trial (RESPECT-2). Sex Transm Dis. 2005;32(2):130–8.
Berg RC, Ross MW, Tikkanen R. The effectiveness of MI4MSM: how useful is motivational interviewing as an HIV risk prevention program for men who have sex with men? A systematic review. AIDS Edu Prev. 2011;23(6):533–49.
Vagenas P, Wickersham JA, Calabrese SK, Lama JR, Benites CM, Pun M, et al. Validation of the 'drinking expectancy questionnaire for men who have sex with men' in Peru. Drug Alcohol Rev. 2015;34(5):559–66.
Leaity S, Sherr L, Wells H, Evans A, Miller R, Johnson M, et al. Repeat HIV testing: high-risk behaviour or risk reduction strategy? AIDS (London, England). 2000;14(5):547–52.
Deiss RG, Segura ER, Clark JL, Konda KA, Leon SR, Caceres CF, et al. Testing for HIV and sexually transmitted infections among men who have sex with men (MSM) in Lima, Peru: opportunities for treatment and risk modification. San Francisco: APHA; 2012.
Eaton LA, Huedo-Medina TB, Kalichman SC, Pellowski JA, Sagherian MJ, Warren M, et al. Meta-analysis of single-session behavioral interventions to prevent sexually transmitted infections: implications for bundling prevention packages. Am J Public Health. 2012;102(11):e34–44.
Lin JS, Whitlock E, O'Connor E, Bauer V. Behavioral counseling to prevent sexually transmitted infections: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149(7):497–508.
Wells BE, Starks TJ, Parsons JT, Golub S. Conflict and expectancies interact to predict sexual behavior under the influence among gay and bisexual men. J Health Psychol. 2014;19(7):821–35.
Vagenas P, Ludford KT, Gonzales P, Peinado J, Cabezas C, Gonzales F, et al. Being unaware of being HIV-infected is associated with alcohol use disorders and high-risk sexual behaviors among men who have sex with men in Peru. AIDS Behav. 2014;18(1):120–7.
Eaton LA, Kalichman SC, Kalichman MO, Driffin DD, Baldwin R, Zohren L, et al. Randomised controlled trial of a sexual risk reduction intervention for STI prevention among men who have sex with men in the USA. Sex Transm Infect. 2018;94(1):40–5.
Acknowledgements
We would like to thank the study participants and staff who devoted their time and efforts to make this project possible. Funding for this work was provided by the US National Institute of Health Grants NIH R25 MH087222 and NIH R34 MH105272 to JLC.
Funding
Funding for this work was provided by the US National Institute of Health Grants NIH R25 MH087222 and NIH R34 MH 105272 to JLC.
Author information
Authors and Affiliations
Contributions
JLC, ERS, JD, RC, FN and RCP contributed to the conception and design. JLC, ERS, RC, SC-G, AC-H, WG-S and RCP contributed to the acquisition of data. ERS, MRB and RCP contributed to the data analysis. JLC, ERS, MRB and JD contributed to the interpretation of the data and drafting of the manuscript. All authors critically revised the manuscript, agree to be fully accountable for ensuring the integrity and accuracy of the work, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest to disclose.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Boards of the University of California, Los Angeles and the Asociación Civil Via Libre and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards (and registered with www.ClinicalTrials.gov; Protocol Number NCT03010020).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Passaro, R.C., Chávez-Gomez, S., Castañeda-Huaripata, A. et al. Personalized Cognitive Counseling Reduces Drinking Expectancy Among Men Who Have Sex with Men and Transgender Women in Lima, Peru: A Pilot Randomized Controlled Trial. AIDS Behav 24, 3205–3214 (2020). https://doi.org/10.1007/s10461-020-02882-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-020-02882-6