Abstract
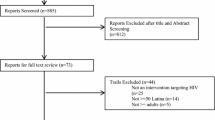
Adolescent girls and young women (AGYW) ages (15–24 years old) in Southern and Eastern Africa account for nearly 30% of all new HIV infections. We conducted a systematic review of studies examining the effectiveness of behavioral, structural, and combined (behavioral + structural) interventions on HIV incidence and risky sexual behaviors among AGYW. Following PRISMA guidelines, we searched PubMed, CINAHL, Web of Science, and Global Health. Twenty-two studies met inclusion criteria conducted in Eastern and Southern Africa and comprised behavioral, structural, or combined (behavioral and structural) interventions. All findings are based on 22 studies. HIV incidence was significantly reduced by one structural intervention. All three types of interventions improved condom use among AGYW. Evidence suggests that structural interventions can reduce HIV incidence, while behavioral and combined interventions require further investigation.
Resumen
Niñas adolescentes y las mujeres jóvenes (15–24 años) en África meridional y oriental representan casi 30% de las nuevas infecciones por VIH. Se realizó una revisión sistemática de estudios que examinan la efectividad de las intervenciones estructurales, de comportamiento, y combinadas (comportamiento + estructurales) sobre la incidencia de VIH y las conductas sexuales de alto riesgo entre niñas adolescentes y las mujeres jóvenes. Siguiendo las pautas de PRISMA, se buscaron estudios en PubMed, CINAHL, Web of Science, y Global Health. Veintidós estudios cumplieron con los criterios de inclusión realizados en África oriental y meridional, e incluyeron intervenciones de comportamiento, estructurales, o combinadas (comportamiento + estructurales). Todos los resultados y conclusiones están basados en los 22 estudios. La incidencia de VIH fue significativamente reducida por una intervención estructural. Los tres tipos de intervenciones mejoraron el uso de condones entre niñas adolescentes y las mujeres jóvenes. Evidencia sugiere que las intervenciones estructurales pueden reducir la incidencia de VIH mientras intervenciones de comportamiento e intervenciones combinadas requieren mayor investigación.



Similar content being viewed by others
References
UNAIDS. UNAIDS Data. Geneva: UNAIDS; 2017. p. 2017.
Harrison A, Colvin CJ, Kuo C, Swartz A, Lurie M. Sustained high HIV incidence in young women in Southern Africa: social, behavioral, and structural factors and emerging intervention approaches. Curr HIV/AIDS Rep. 2015;12(2):207–15.
Dellar RC, Dlamini S, Karim QA. Adolescent girls and young women: key populations for HIV epidemic control. J Int AIDS Soc. 2015;18(2 Suppl 1):19408.
Harrison A, Colvin CJ, Kuo C, Swartz A, Lurie M. Sustained high HIV incidence in young women in Southern Africa: social, behavioral and structural factors and emerging intervention approaches. Curr HIV/AIDS Rep. 2015;12(2):207–15.
Idele P, Gillespie A, Porth T, Suzuki C, Mahy M, Kasedde S, et al. Epidemiology of HIV and AIDS among adolescents: current status, inequities, and data gaps. J Acquir Immune Defic Syndr. 1999;2014(66 Suppl 2):S144–S153153.
Naicker N, Kharsany ABM, Werner L, van Loggerenberg F, Mlisana K, Garrett N, et al. Risk factors for HIV acquisition in high risk women in a generalised epidemic setting. AIDS Behav. 2015;19(7):1305–16.
Padian NS, McCoy SI, Balkus JE, Wasserheit JN. Weighing the gold in the gold standard: challenges in HIV prevention research. AIDS. 2010;24(5):621–35.
Eaton L, Flisher AJ, Aaro LE. Unsafe sexual behaviour in South African youth. Soc Sci Med. 2003;56(1):149–65.
CDC. Compendium of evidence-based interventions and best practices for HIV prevention Atlanta, GA. https://www.cdc.gov/hiv/research/interventionresearch/compendium/index.html (2019). Accessed 7 June 2019.
Bekker LG, Beyrer C, Quinn TC. Behavioral and biomedical combination strategies for HIV prevention. Cold Spring Harbor Perspect Med. 2012;2(8):a007435.
Phillips AF, Pirkle CM. Moving beyond behaviour: advancing HIV risk prevention epistemologies and interventions (a report on the state of the literature). Glob Public Health. 2011;6(6):577–92.
Latkin CA, Knowlton AR. Micro-social structural approaches to HIV prevention: a social ecological perspective. AIDS Care. 2005;17(sup1):102–13.
Van Damme L, Corneli A, Ahmed K, Agot K, Lombaard J, Kapiga S, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367(5):411–22.
Cowan FM, Delany-Moretlwe S, Sanders EJ, Mugo NR, Guedou FA, Alary M, et al. PrEP implementation research in Africa: what is new? J Int AIDS Soc. 2016;19(7 Suppl 6):21101.
Abdul-Quader AS, Collins C. Identification of structural interventions for HIV/AIDS prevention: the concept mapping exercise. Public Health Rep. 2011;126(6):777–88.
Blankenship KM, Friedman SR, Dworkin S, Mantell JE. Structural interventions: concepts, challenges and opportunities for research. J Urban Health. 2006;83(1):59–72.
Auerbach JD, Parkhurst JO, Caceres CF. Addressing social drivers of HIV/AIDS for the long-term response: conceptual and methodological considerations. Glob Public Health. 2011;6(Suppl 3):S293–309.
Gupta GR, Parkhurst J, Ogden J, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372:765–75.
Piot PP. Coming to terms with complexity: a call to action for HIV prevention. Lancet. 2008;372(9641):845–59.
Merson MM. Combination HIV prevention. Lancet. 2008;372(9652):1805–6.
Baxter C, Abdool KS. Combination HIV prevention options for young women in Africa. Afr J AIDS Res AJAR. 2016;15(2):109–21.
Clauser SB, Taplin SH, Foster MK, Fagan P, Kaluzny AD. Multilevel intervention research: lessons learned and pathways forward. J Natl Cancer Inst Monogr. 2012;2012(44):127–33.
Gorin SS, Badr H, Krebs P, Prabhu DI. Multilevel interventions and racial/ethnic health disparities. J Natl Cancer Inst Monogr. 2012;2012(44):100–11.
Breslau ES, Gorin SS, Edwards HM, Schonberg MA, Saiontz N, Walter LC. An individualized approach to cancer screening decisions in older adults: a multilevel framework. J Gen Intern Med. 2016;31(5):539–47.
Scholmerich VL, Kawachi I. Translating the socio-ecological perspective into multilevel interventions: gaps between theory and practice. Health Educ Behav. 2016;43(1):17–20.
Liberati A, Altman GD, Tetzlaff J, Mulrow C, Gøtzsche CP, Ioannidis PAJ, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):1–28.
Moher D, Liberati A, Tetzlaff J, Altman GD, TP Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):1–6.
Auerbach JDJD. Addressing social drivers of HIV/AIDS for the long-term response: conceptual and methodological considerations. Glob Public Health. 2011;6(suppl 3):S293–S309.
Burnette ML, Lucas E, Ilgen M, Frayne SM, Mayo J, Weitlauf JC. Prevalence and health correlates of prostitution among patients entering treatment for substance use disorders. Arch Gen Psychiatry. 2008;65(3):337–44.
Covidence. Systematic review software. Melbourne: Veritas Health Innovation; 2019.
Higgins J, Green S. Cochrane handbook for systematic reviews of interventions. Chichester: Wiley; 2011.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Canadian Intellectual Property Office, assignee. Mixed methods appraisal tool (MMAT), version 2018. Ottawa: Industry Canada; 2018.
Harrison A, Hoffman S, Mantell JE, Smit JA, Leu CS, Exner TM, et al. Gender-focused HIV and pregnancy prevention for school-going adolescents: the Mpondombili pilot intervention in KwaZulu-Natal, South Africa. J HIV-AIDS Soc Serv. 2016;15(1):29–47.
Smith E, Palen LA, Caldwell L, Flisher A, Graham J, Mathews C, et al. Substance use and sexual risk prevention in Cape Town, South Africa: an evaluation of the healthwise program. Prev Sci. 2008;9(4):311–21.
Agha S, Van Rossem R. Impact of a school-based peer sexual health intervention on normative beliefs, risk perceptions, and sexual behavior of Zambian adolescents. J Adolesc Health. 2004;34(5):441–52.
Ybarra ML, Bull SS, Prescott TL, Korchmaros JD, Bangsberg DR, Kiwanuka JP. Adolescent abstinence and unprotected sex in CyberSenga, an Internet-based HIV prevention program: randomized clinical trial of efficacy. PLoS ONE. 2013;8(8):e70083.
Fitzgerald AM, Stanton BF, Terreri N, Shipena H, Li X, Kahihuata J, et al. Use of western-based HIV risk-reduction interventions targeting adolescents in an African setting. J Adolesc Health. 1999;25(1):52–61.
Thurman TR, Kidman R, Carton TW, Chiroro P. Psychological and behavioral interventions to reduce HIV risk: evidence from a randomized control trial among orphaned and vulnerable adolescents in South Africa. AIDS Care. 2016;28(Suppl 1):8–15.
Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Puren A, et al. Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ. 2008;337:a506.
Erulkar AS, Ettyang LI, Onoka C, Nyagah FK, Muyonga A. Behavior change evaluation of a culturally consistent reproductive health program for young Kenyans. Int Fam Plan Perspect. 2004;30(2):58–67.
Wingood GM, Reddy P, Lang DL, Saleh-Onoya D, Braxton N, Sifunda S, et al. Efficacy of SISTA South Africa on sexual behavior and relationship control among isiXhosa women in South Africa: results of a randomized-controlled trial. J Acquir Immune Defic Syndr. 2013;63(Suppl 1):S59–65.
Handa S, Halpern CT, Pettifor A, Thirumurthy H. The government of Kenya's cash transfer program reduces the risk of sexual debut among young people age 15–25. PLoS ONE. 2014;9(1):e85473.
Pettifor A, MacPhail C, Hughes JP, Selin A, Wang J, Gomez-Olive FX, et al. The effect of a conditional cash transfer on HIV incidence in young women in rural South Africa (HPTN 068): a phase 3, randomised controlled trial. Lancet Glob Health. 2016;4(12):e978–e988988.
Hallfors DD, Cho H, Rusakaniko S, Mapfumo J, Iritani B, Zhang L, et al. The impact of school subsidies on HIV-related outcomes among adolescent female orphans. J Adolesc Health. 2015;56(1):79–84.
Baird SJ, Garfein RS, McIntosh CT, Ozler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet. 2012;379(9823):1320–9.
Beauclair R, Dushoff J, Delva W. Partner age differences and associated sexual risk behaviours among adolescent girls and young women in a cash transfer programme for schooling in Malawi. BMC Public Health. 2018;18(1):403.
Agha S. A quasi-experimental study to assess the impact of four adolescent sexual health interventions in sub-Saharan Africa. Int Fam Plan Perspect. 2002;28(2):67.
Ross DA, Changalucha J, Obasi AI, Todd J, Plummer ML, Cleophas-Mazige B, et al. Biological and behavioural impact of an adolescent sexual health intervention in Tanzania: a community-randomized trial. AIDS. 2007;21(14):1943–55.
Cowan FM, Pascoe SJ, Langhaug LF, Mavhu W, Chidiya S, Jaffar S, et al. The Regai Dzive Shiri project: results of a randomized trial of an HIV prevention intervention for youth. AIDS. 2010;24(16):2541–52.
Pronyk PM, Hargreaves JR, Kim JC, Morison LA, Phetla G, Watts C, et al. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet. 2006;368(9551):1973–83.
Dunbar MS, Dufour MSK, Lambdin B, Mudekunye-Mahaka I, Nhamo D, Padian NS. The SHAZ! project: results from a pilot randomized trial of a structural intervention to prevent HIV among adolescent women in Zimbabwe. PLoS ONE. 2014;9(11):e113621.
Jewkes R, Gibbs A, Jama-Shai N, Willan S, Misselhorn A, Mushinga M, et al. Stepping Stones and Creating Futures intervention: shortened interrupted time series evaluation of a behavioural and structural health promotion and violence prevention intervention for young people in informal settlements in Durban, South Africa. BMC Public Health. 2014;14:1325.
Duflo E, Dupas P, Kremer M. Education, HIV, and early fertility: experimental evidence from Kenya. Am Econ Rev. 2015;105(9):2757–97.
Wingood GM, DiClemente RJ, Robinson-Simpson L, Lang DL, Caliendo A, Hardin JW. Efficacy of an HIV intervention in reducing high-risk HPV, Non-viral STIs, and concurrency among African-American women: a randomized controlled trial. J Acquir Immune Defic Syndr. 2013;63(1):S36–S43.
Pettifor A, MacPhail C, Hughes JP, Selin A, Wang J, Gómez-Olivé FX, et al. The effect of a conditional cash transfer on HIV incidence in young women in rural South Africa (HPTN 068): a phase 3, randomised controlled trial. Lancet Glob Health. 2016;4(12):e978–e988988.
Doyle AM, Weiss HA, Maganja K, Kapiga S, McCormack S, Watson-Jones D, et al. The long-term impact of the MEMA kwa Vijana adolescent sexual and reproductive health intervention: effect of dose and time since intervention exposure. PLoS ONE. 2011;6(9):e24866.
Walque DD, Dow WH, Nathan R. Rewarding safer sex: conditional cash transfers for HIV/STI prevention. Policy research working paper, vol. 1. Washington: World Bank; 2014.
Pettifor A, MacPhail C, Nguyen N, Rosenberg M. Can money prevent the spread of HIV? A review of cash payments for HIV prevention. AIDS Behav. 2012;16(7):1729–38.
Pettifor AE, Levandowski BA, Macphail C, Padian NS, Cohen MS, Rees HV. Keep them in school: The importance of education as a protective factor against HIV infection among young South African women. Int J Epidemiol. 2008;37(6):1266–73.
Small E, Nikolova SP, Narendorf SC. Synthesizing gender based HIV interventions in Sub-Sahara Africa: a systematic review of the evidence. AIDS Behav. 2013;17(9):2831–44.
Quigley MA, Kamali A, Kinsman J, Kamulegeya I, Nakiyingi-Miiro J, Kiwuwa S, et al. The impact of attending a behavioural intervention on HIV incidence in Masaka, Uganda. AIDS. 2004;18(15):2055–63.
Fonner VA, Kennedy CE, O’Reilly KR, Sweat MD. Systematic assessment of condom use measurement in evaluation of HIV prevention interventions: need for standardization of measures. AIDS Behav. 2014;18(12):2374–86.
Hewett PC, Mensch BS, Erulkar AS. Consistency in the reporting of sexual behaviour by adolescent girls in Kenya: a comparison of interviewing methods. Sex Transm Infect. 2004;80(Suppl 2):ii43–ii48.
Hewett PC, Mensch BS, Ribeiro MCSDA, Jones HE, Lippman SA, Montgomery MR, et al. Using sexually transmitted infection biomarkers to validate reporting of sexual behavior within a randomized, experimental evaluation of interviewing methods. Am J Epidemiol. 2008;168(2):202–11.
Gallo MF, Steiner MJ, Hobbs MM, Warner L, Jamieson DJ, Macaluso M. Biological markers of sexual activity: tools for improving measurement in HIV/sexually transmitted infection prevention research. Sex Transm Dis. 2013;40(6):447–52.
Kelly CA, Hewett PC, Mensch BS, Rankin JC, Nsobya SL, Kalibala S, et al. Using biomarkers to assess the validity of sexual behavior reporting across interview modes among young women in Kampala, Uganda. Stud Fam Plan. 2014;45(1):43–58.
Luke N, Goldberg RE, Mberu BU, Zulu EM. Social Exchange and Sexual Behavior in Young Women's Premarital Relationships in Kenya. J Marriage Fam. 2011;73(5):1048–64.
Hattori MK, DeRose L. Young women's perceived ability to refuse sex in urban Cameroon. Stud Fam Plan. 2008;39(4):309–20.
Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. Ann Intern Med. 2001;134(8):657–62.
Da-Costa BR, Cevallos M, Altman G, Rutjes AW, Egger M. The Strengthening the reporting of observational studies in epidemiology (STROBE) statement. Bern: Institute of Social & Preventive Medicine (ISPM), University of Bern; 2010.
Collins LM. Optimization of behavioral, biobehavioral, and biomedical interventions : the multiphase optimization strategy (MOST). Cham: Springer; 2018.
Acknowledgements
The authors would like to thank Mark Toles, PhD, RN, FAAN, Suzanne Thoyre, PhD, RN, Jada L. Brooks, PhD, MSPH, RN, and all colleagues of CM for useful critiques, feedback, and discussions that helped shape this manuscript.
Author information
Authors and Affiliations
Contributions
CM developed the idea, developed search terms, extracted data, and wrote the manuscript. SK provided critical feedback on the initial development of the idea, read all manuscripts and provided in depth feedback. MG reviewed articles, extracted data, and provided critical feedback. AP provided initial guidance on HIV intervention research and gaps reviewed and provided critical feedback on manuscript. JW provided feedback on manuscript helped shape the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Muthoni, C.N., Kneipp, S.M., Gichane, M.W. et al. A Systematic Review of HIV Interventions for Young Women in Sub-Saharan Africa. AIDS Behav 24, 3395–3413 (2020). https://doi.org/10.1007/s10461-020-02914-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-020-02914-1