Abstract
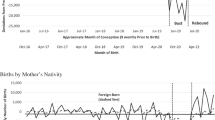
In late 2015, the Brazilian Ministry of Health and the Pan American Health Organization classified the increase in congenital malformations associated with the Zika virus (ZIKV) as a public health emergency. The risk of ZIKV-related congenital syndrome poses a threat to reproductive outcomes that could result in declining numbers of live births and potentially fertility. Using monthly microdata on live births from the Brazilian Information System on Live Births (SINASC), this study examines live births and fertility trends amid the ZIKV epidemic in Brazil. Findings suggest a decline in live births that is stratified across educational and geographic lines, beginning approximately nine months after the link between ZIKV and microcephaly was publicly announced. Although declines in total fertility rates were small, fertility trends estimated by age and maternal education suggest important differences in how Zika might have impacted Brazil’s fertility structure. Further findings confirm the significant declines in live births in mid-2016 even when characteristics of the municipality are controlled for; these results highlight important nuances in the timing and magnitude of the decline. Combined, our findings illustrate the value of understanding how the risk of a health threat directed at fetuses has led to declines in live births and fertility.






Similar content being viewed by others
Notes
The number of Google searches for the word “microcefalia” went from zero to its highest ever in November 2015.
We refer to the concept of social exposure—that is, to changes within one’s social environment that may affect their thinking, behavior, intentions, and/or well-being. In this particular case, we refer to individuals’ social exposure to microcephalic babies and children.
In work in progress, Rangel et al. (forthcoming) have also found evidence of large changes in birth rates in Brazil during the epidemic, using an index of mosquito infestation to leverage the spread of the ZIKV epidemic across Brazil’s microregions.
Abortion is mostly illegal in Brazil, but it is nonetheless frequent (Diniz and Medeiros 2010; Diniz et al. 2017). A 2016 national household survey using ballot box techniques suggests that one in every five women will have had an abortion by age 40, with abortion more commonly occurring among young women up to age 24 (Diniz et al. 2017). The only data available on abortion in Brazil are hospital admittances owing to abortion complications; to estimate abortion, it is necessary to make assumptions that the characteristics of the women seeking hospitalization after the procedure did not change with the Zika epidemic (Singh and Wulf 1991).
Projections of women at childbearing ages by educational levels are not widely available for Brazil, so we apply the educational structure from the nationally representative PNAD (1995 to 1999, 2001 to 2009, and 2011 to 2016) to projections to estimate the number of women by levels of education (IBGE 2019). We interpolate monthly data from the yearly trend using a nonstochastic exponential interpolation method. Then we calculate the proportions for each interpolated number of women at each five-year age group by month-year and education level and use these proportions to obtain the expected numbers using the Cedeplar totals.
Brazil’s Census Bureau does not make municipal projections available. Thus, we use projections estimated by Cedeplar based on 2010 census data. The overall number of women at childbearing ages is estimated using a combination of small-area estimation procedures, multiregional migration tables, and other standard projection techniques adjusted by expert opinion on the future behavior of each demographic component (Cedeplar 2014).
We eliminate five municipalities out of the 5,570 total number of Brazilian municipalities because they were created after 2010 and therefore do not have corresponding population projections data estimated using the 2010 census. We aggregate localities in the outskirts of Brasília as a single entity; this is usual practice regarding the federal district.
Administrative reports and vital statistics information on live births in developing countries typically face data quality issues, including delay in registration, misreporting, and undercounting. For 2014, undercount at the national level was 4% (Ministério da Saúde 2017).
Live birth data sets were transferred directly from the SINASC website as updated information became available (May 5, 2017; July 29, 2017; March 20, 2018; and April 28, 2018, when 2016 data became final). Finally, on March 21, 2019, we retrieved the whole data set once again.
We also estimate fertility rates using as the denominator projections by the Brazilian Census Bureau (IBGE 2013) to assure that results held regardless of the denominator used (not shown but available upon request). We estimate the observed fertility rates using direct methods and the expected fertility rates by indirect methods, using the census.
We use maternal education as a measure of SES for conceptual and methodological reasons. Conceptually, maternal education is the strongest socioeconomic predictor of live births and fertility in Brazil (Cavenaghi and Berquó 2014; Rios-Neto et al. 2018); it is a more stable measure than income and has been used extensively as the major proxy for SES in Brazil (Lam and Duryea 1999; Marteleto and Dondero 2013; Potter et al. 2010). Methodologically, the data set we use offers two variables that reflect SES: maternal education and maternal occupation. Information on income is not collected. Information on maternal occupation is collected but not made available for public use. Maternal education is thus the only proxy available to us. Fortunately, it is missing in only 1.3% to 2.3% of cases, depending on the year.
The GFR is the ratio between the number of live births and the number of person-years lived by females aged 15–49 years (Preston et al. 2001). Because the GFR depends on the proportion of person-years lived by females aged 15–49 years, the rates are sensible to compositional differences in the age structure of reproductive-aged women. As such, the GFR could potentially change over time simply because of changes in the proportion of women at childbearing age, not because of actual changes in birth patterns. This is an undesirable property of the GFR and the main reason it is seldom used. We estimate GFRs as a counterfactual exercise to predict the expected number of births to highlight the very effect that a changing age structure of women at childbearing ages would have been on the number of live births. We use the GFR’s limitation—its sensitivity to the age structure of women ages 15–49—as a resource to compare actual with expected live births. This is a way to tease out whether the change in the number of live births we document could have been the result of a change in age structure. Because the counterfactuals rely on the number of women at childbearing ages from 2010, prior to the ZIKV epidemic, our exercise shows the contribution of changes in age structure only to the GFR. The difference in estimation and the sign of the difference (positive or negative) provide a sense of the magnitude of live births that would have increased/decreased as a result of the aging structure of women at childbearing ages.
This decline in the observed number of live births we examine is not due to compositional effects in the number of females at childbearing ages, suggesting that we cannot infer that the observed decline and the timing of decline in births are attributable to population composition effects.
Fertility levels are slightly similar across educational groups for older age groups in Brazil (Camarano 2014), but fertility might be qualitatively different for low- versus high-educated according to birth order, as the pattern of first births is highly dependent on mother’s education; high-educated women are having the highest first birth intensity around age 32 while low-educated women have their highest first birth intensity around ages 18–21 (Lima et al. 2018).
References
Agadjanian, V., & Prata, N. (2002). War, peace, and fertility in Angola. Demography, 39, 215–231.
Aiken, A. R., Scott, J. G., Gomperts, R., Trussell, J., Worrell, M., & Aiken, C. E. (2016). Requests for abortion in Latin America related to concern about Zika virus exposure. New England Journal of Medicine, 375, 396–398.
Ali, S., Gugliemini, O., Harber, S., Harrison, A., Houle, L., Ivory, J., . . . Mordecai, E. A. (2017). Environmental and social change drive the explosive emergence of Zika virus in the Americas. PLoS Neglected Tropical Diseases, 11, e0005135. https://doi.org/10.1371/journal.pntd.0005135
Amaral, E., Almeida, M., & Gonçalves, G. (2016). Characterization of fertility levels in Brazil, 1970–2010 (SSRN Scholarly Paper No. 2798918). Rochester, NY: Social Science Research Network.
Araújo, T. V., Ximenes, R. A., Miranda-Filho, D. d., Souza, W. V., Montarroyos, U. R., Lopes Melo, A. P., . . . Rodrigues, L. C. (2017). Association between microcephaly, Zika virus infection, and other risk factors in Brazil: Final report of a case-control study. Lancet Infectious Diseases, 18, 328–336.
Baldwin, J., & DeSouza, E. (2001). Modelo de María and machismo: The social construction of gender in Brazil. Revista Interamericana de Psicología, 35(1), 9–29.
Behrman, J. A., & Weitzman, A. (2016). Effects of the 2010 Haiti earthquake on women’s reproductive health. Studies in Family Planning, 47, 3–17.
Bongaarts, J. (1978). A framework for analyzing the proximate determinants of fertility. Population and Development Review, 4, 105–132.
Borges, A. L. V., Fujimori, E., Kuschnir, M. C. C., Chofakian, C. B. do N., Moraes, A. J. P., Azevedo, G. D., . . . Vasconcellos, M. T. L. (2016). ERICA: Sexual initiation and contraception in Brazilian adolescents. Revista de Saúde Pública,50(Suppl. 1), 15s. https://doi.org/10.1590/s01518-8787.2016050006686
Brasil. (2015a, August 26). Febre pelo vírus Zika: Uma revisão narrativa sobre a doença [Zika Virus fever: A narrative review about the disease] (Boletim Epidemiológico Vol. 46, No. 26). Brasilia, Brasil: Ministério da Saúde, Governo Federal. Retrieved from http://portalarquivos2.saude.gov.br/images/pdf/2015/agosto/26/2015-020-publica%2D%2D%2D%2Do.pdf
Brasil. (2015b, November 11). Portaria N° 1.813, de 11 de Novembro de 2015. Declara Emergência em Saúde Pública de importância Nacional (ESPIN) por alteração do padrão de ocorrência de microcefalias no Brasil [Declaration N° 1.813, of November 11th 2015. Declaration of Public Health Emergency of National Concern (PHENC) due to alterations in the pattern of occurrence of microcephaly in Brazil]. Brasília, Brasil: Ministério da Saúde, Governo Federal. Retrieved from http://bvsms.saude.gov.br/bvs/saudelegis/gm/2015/prt1813_11_11_2015.html
Brasil. (2015c, November 28). Ministério da Saúde confirma relação entre virus Zika e casos de microcefalia [Ministry of Health confirms relationship between Zika Virus and cases of microcephaly]. Brasília, Brasil: Ministério da Saúde, Governo Federal. Retrieved from http://www.saude.gov.br/noticias/agencia-saude/21014-ministerio-da-saude-confirma-relacao-entre-virus-zika-e-microcefalia
Brasil. (2016, January 11). Monitoramento dos casos de microcefalia no Brasil até a Semana Epidemiológica 51/2015 [Monitoring of microcephaly cases in Brazil until Epidemiological Week 51/2015] (Boletim Epidemiológico, Vol. 47, No. 1). Brasília, Brasil: Ministério da Saúde, Secretaria de Vigilância em Saúde, Governo Federal. Retrieved from http://portalarquivos2.saude.gov.br/images/pdf/2016/janeiro/11/2015-053-para-substituir-na-p%2D%2Dgina.pdf
Brasil. (2017, February 27). Monitoramento integrado de alterações no crescimento e desenvolvimento relacionadas à infecção pelo vírus Zika e outras etiologias infecciosas, da Semana Epidemiológica 45/2015 até a Semana Epidemiológica 02/2017 [Integrative monitoring of alterations in growth and development associated with infection by Zika Virus and other infectious diseases, from Epidemiological Week 45/2015 to Epidemiological Week 02/2017] (Boletim Epidemiológico, Vol. 48, No. 6). Brasília, Brasil: Ministério da Saúde, Secretaria de Vigilância em Saúde, Governo Federal. Retrieved from http://portalarquivos2.saude.gov.br/images/pdf/2017/fevereiro/27/2017_003.pdf
Brasil. (2019, November). Síndrome congênita associada à infecção pelo vírus Zika. Situação epidemiológica, ações desenvolvidas e desafios de 2015 a 2019 [Congenital Zika Syndrome. Epidemiological situation, actions taken and challenges] (Boletim Epidemiológico. Número Especial). Brasília, Brasil: Ministério da Saúde, Secretaria de Vigilância em Saúde, Governo Federal. Retrieved from http://portalarquivos2.saude.gov.br/images/pdf/2019/dezembro/05/be-sindrome-congenita-vfinal.pdf
Calvet, G., Aguiar, R. S., Melo, A. S. O., Sampaio, S. A., Filippis, I., Fabri, A., . . . Filippis, A. M. B. (2016). Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: A case study. Lancet, 16, 653–660.
Camarano, A. A. (Org.). (2014). Novo regime demográfico: Uma nova relação entre população e desenvolvimento? [New Demographic Regime: A new relationship between population and development?] Rio de Janeiro, Brasil: Instituto de Pesquisa Econômica Aplicada.
Castro, M. C., Han, Q. C., Carvalho, L. R., Victora, C. G., & França, G. V. A. (2018). Implications of the Zika virus and congenital Zika syndrome for the number of live births in Brazil. Proceedings of the National Academy of Sciences, 115, 6177–6182.
Cavenaghi, S., & Alves, J. E. D. (2009, April–May). Fertility and contraception in Latin America: Historical trends, recent patterns. Paper presented at the annual meeting of the Population Association of America, Detroit, MI.
Cavenaghi, S., & Berquó, E. (2014). Perfil socioeconômico e demográfico da fecundidade no Brasil de 2000 a 2010 [Socioeconomic and demographic profile of fertility in Brazil from 2000 to 2010]. In S. Cavenaghi & W. Cabella (Eds.), Comportamiento reproductivo y fecundidad en América Latina: Una agenda inconclusa (pp. 220–240). Rio de Janeiro, Brasil: Associação Latino-Americana de Publicidade.
Cedeplar. (2014). Projeção populacional por sexo e grupo etário até 2050 [Population Projection by sex and age group until 2050]. Belo Horizonte, Brasil: Centro de Desenvolvimento e Planejamento Regional da UFMG.
Coutinho, R. Z. (2016). The transition to low fertility in Brazil (Doctoral dissertation). Department of Sociology, University of North Carolina at Chapel Hill, Chapel Hill, NC. Retrieved from https://www.semanticscholar.org/paper/The-Transition-to-Low-Fertility-in-Brazil-Coutinho/87c08d11ad9d7ded6248627fd072e835c0b05699
Cummings, D. R. (2014). Seasonality updated in 28 European/Mediterranean countries: A continuing enigma. American Journal of Human Biology, 26, 424–426.
de Andrade, L. O., Pellegrini Filho, A., Solar, O., Rígoli, F., de Salazar, L. M., Castell-Florit, P., . . . Atun, R. (2015). Social determinants of health, universal health coverage, and sustainable development: Case studies from Latin American countries. Lancet, 385, 1343–1351.
de Oliveira, W. K., Carmo, E. H., Henriques, C. M., Coelho, G., Vazquez, E., Cortez-Escalante, J., . . . Dye, C. (2017a). Zika virus infection and associated neurologic disorders in Brazil. New England Journal of Medicine, 376, 1591–1593.
de Oliveira, W. K., de França, G. V. A., Carmo, E. H., Duncan, B., Kuchenbecker, R. S., & Schmidt, M. I. (2017b). Infection-related microcephaly after the 2015 and 2016 Zika virus outbreaks in Brazil: A surveillance-based analysis. Lancet, 390, 821–912.
Diniz, D. (2016). Zika: Do sertão nordestino à ameaça global [Zika: From the Brazilian backlands to global threat]. Rio de Janeiro, Brasil: Civilização Brasileira.
Diniz, D., & Medeiros, M. (2010). Aborto no Brasil: Uma pesquisa domiciliar com técnica de urna [Abortion in Brazil: A household survey using the ballot box technique]. Ciência & Saúde Coletiva, 15, 959–966.
Diniz, D., Medeiros, M., & Madeiro, A. (2017). Pesquisa nacional de aborto 2016 [National Survey of Abortion 2016]. Ciência & Saúde Coletiva, 22, 653–660.
Dip, A. (2013, September 17). A cada dois dias, uma brasileira morre por aborto [Every two days, one Brazilian dies due to abortion]. Retrieved from https://istoe.com.br/324829_A+CADA+DOIS+DIAS+UMA+BRASILEIRA+MORRE+POR+ABORTO/
Farias, M. R., Leite, S. N., Tavares, N. U. L., & Oliveira, M. A., Arrais, P. S. D., Bertoldi, A. D., Mengue, S.S. (2016). Utilização e acesso a contraceptivos orais e injetáveis no Brasil [Utilization and access to oral contraceptives and injectables in Brazil]. Revista de Saúde Pública, 50(Suppl. 2), 14s. https://doi.org/10.1590/s1518-8787.2016050006176
Ferreira, F. H. G., Lanjouw, P., & Neri, M. (2003). A robust poverty profile for Brazil using multiple data sources. Revista Brasileira de Economía, 57(1), 59–92.
Finlay, J. E. (2009). Fertility response to natural disasters: The case of three high mortality earthquakes (Policy Research Working Paper No. 4883). Washington, DC: World Bank. Retrieved from http://documents.worldbank.org/curated/en/118031468284119109/Fertility-response-to-natural-disasters-the-case-of-three-high-mortality-earthquakes
Guedes, G. R., Coutinho, R. Z., Marteleto, L. J., Pereira, W. H. S. P., & Duarte, D. (2018). Signifying Zika: Heterogeneity in the representations of the virus by history of infection. Cadernos de Saúde Pública, 34, e0000321. https://doi.org/10.1590/0102-311x00003217
Hoen, B., Schaub, B., Funk, A. L., & Ardillon, V., Boullard, M., Cabié, A., . . . Fontanet, A. (2018). Pregnancy outcomes after ZIKV infection in French territories in the Americas. New England Journal of Medicine, 378, 985–994.
Instituto Brasileiro de Geografia e Estatística (IBGE). (2012). Censo demográfico 2010: Nupcialidade, fecundidade e migração [Demographic Census 2010: Nupciality, fertility and migration]. Rio de Janeiro, Brasil: Instituto Brasileiro de Geografia e Estatística.
Instituto Brasileiro de Geografia e Estatística (IBGE). (2013). Projeção da população do Brasil por sexo e idade para o período 2000–2060 [Brazilian population projection by sex and age for the period between 2000 and 2060]. Rio de Janeiro, Brasil: Instituto Brasileiro de Geografia e Estatística. Retrieved from https://ww2.ibge.gov.br/home/estatistica/populacao/projecao_da_populacao/2013/default.shtm
Instituto Brasileiro de Geografia e Estatística (IBGE). (2019). Pesquisa Nacional por Amostra de Domicílios Contínua (PNAD Contínua) [Brazilian National Longitudinal Household Sample Survey (PNAD Contínua)]. Rio de Janeiro, Brasil: Instituto Brasileiro de Geografia e Estatística. Retrieved from https://ww2.ibge.gov.br/home/estatistica/populacao/trabalhoerendimento/pnad2015/default.shtm
Itaborai, N. R. (2015). Las desigualdades de clase en el comportamiento reproductivo en el Brasil: Democratización incompleta y paradojas de la fecundidad juvenil [Social class disparities in reproductive behavior in Brazil: Incomplete democrarization and paradox of youth fertility]. Notas de Población, 42, 61–89. Retrieved from https://repositorio.cepal.org/bitstream/handle/11362/38523/1/03_Reis_100A.pdf
Johnson-Hanks, J. (2004). Uncertainty and the second space: Modern birth timing and the dilemma of education. European Journal of Population/Revue européenne de Démographie, 20, 351–373.
Johnson-Hanks, J. (2006). Uncertain honor: Modern motherhood in an African crisis. Chicago, IL: University of Chicago Press.
Joventino, E. S., Ximenes, L. B., Almeida, P. C., & Oria, M. O. B. (2013). The maternal self-efficacy scale for preventing early childhood diarrhea: Validity and reliability. Public Health Nursing, 30, 150–158.
Lam, D., & Duryea, S. (1999). Effects of schooling on fertility, labor supply, and investments in children, with evidence from Brazil. Journal of Human Resources, 34, 160–192.
Le, H. H., Connolly, M. P., Bahamondes, L., Cecatti, J. G., Yu, J., & Hu, H. X. (2014). The burden of unintended pregnancies in Brazil: A social and public health system cost analysis. International Journal of Women’s Health, 6, 663–670. https://doi.org/10.2147/IJWH.S61543
Lima, E. E. C., Zeman, K., Sobotka, T., Nathan, M., & Castro, R. (2018). The emergence of bimodal fertility profiles in Latin America. Population and Development Review, 44, 723–743.
Lin, H. Z., Tambyah, P. A., Yong, E. L., Biswas, A., & Chan, S.-Y. (2017). A review of Zika virus infections in pregnancy and implications for antenatal care in Singapore. Singapore Medical Journal, 58, 171–178.
Marteleto, L., & Dondero, M. (2013). Maternal age at first birth and adolescent education in Brazil. Demographic Research, 28, 793–820. https://doi.org/10.4054/DemRes.2013.28.28
Marteleto, L., & Souza, L. R. (2012). The changing impact of family size on adolescents’ schooling: Assessing the exogenous variation in fertility using twins in Brazil. Demography, 49, 1453–1477.
Marteleto, L., Weitzman, A., Coutinho, R., & Alves, S. (2017). Women’s reproductive intentions and behaviors during the Zika epidemic in Brazil. Population and Development Review, 43, 199–227.
Martine, G. (1996). Brazil’s fertility decline, 1965–95: A fresh look at key factors. Population and Development Review, 22, 47–75.
Martins-Melo, F. R., da Silveira Lima, M., Alencar, C. H., Ramos, A. N., Carvalho, F. H. C., Machado, M. M. T., Heukelbach, J. (2014). Temporal trends and spatial distribution of unsafe abortion in Brazil, 1996–2012. Revista de Saúde Pública, 48, 508–520.
McNeil, D. G., Jr. (2015, December 28). Zika virus, a mosquito-borne infection, may threaten Brazil’s newborns. The New York Times. Retrieved from https://www.nytimes.com/2015/12/29/health/zika-virus-brazil-mosquito-brain-damage.html
Menezes, G., & Aquino, E. M. L. (2009). Research on abortion in Brazil: Gaps and challenges for the public health field. Cadernos de Saúde Pública, 25(Suppl. 2), s193–s204.
Mier-y-Teran-Romero, L., Delorey, M. J., Sejvar, J. J., & Johansson, M. A. (2018). Guillain–Barré syndrome risk among individuals infected with Zika virus: A multi-country assessment. BMC Medicine, 16(67). https://doi.org/10.1186/s12916-018-1052-4
Ministério da Saúde. (2017). Saúde Brasil 2015/2016: Uma análise da situação de saúde e da epidemia pelo vírus Zika e por outras doenças transmitidas pelo Aedes aegypti. Brasília, DF, Brasil: Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Vigilância de Doenças e Agravos Não Transmissíveis e Promoção da Saúde. Retrieved from http://bvsms.saude.gov.br/bvs/publicacoes/saude_brasil_2015_2016_analise_zika.pdf
Ministério da Saúde. (2019). Portal da saúde, sistema de informações de nascidos vivos [Dataset]. Brasília, Brasil: Ministério da Saúde, DATASUS, Departamento de Informática do SUS. Retrieved from http://www2.datasus.gov.br/DATASUS/index.php?area=0205&id=6936&VObj=http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sinasc/cnv/nv
Ministry of Health confirms the relation between microcephaly and ZIKV. (2015, November 28) G1. Retrieved from http://g1.globo.com/bemestar/noticia/2015/11/ministerio-da-saude-confirma-relacao-entre-microcefalia-e-virus-zika.html
Mlakar, J., Korva, M., Tul, N., Popović, M., Poljšak-Prijatelj, M., Mraz, J., . . . Avšič Županc, T. (2016). Zika virus associated with microcephaly. New England Journal of Medicine, 374, 951–958.
Moreira, M. (2013, September–October). Sazonalidade dos nascimentos no Brasil—2000–2010 [Seasonality of births in Brazil—2000–2010]. Paper presented at the XXIX Congreso de la Asociacion Latinoamericana de Sociologia, Santiago, Chile. https://www.researchgate.net/publication/308296347_Sazonalidade_dos_nascimentos_no_Brasil_-_2000-2010
Nascimento, E., Cavalcanti, M. A. F., & Alchieri, J. C. (2017). Adesão ao uso da camisinha: A realidade comportamental no interior do nordeste do Brasil [Condom use adherence: the reality of the behavior in the interior of the Brazilian northeast]. Revista de Salud Pública, 19, 39–44. Retrieved from http://www.redalyc.org/articulo.oa?id=42250687007
Nobles, J., Frankenberg, E., & Thomas, D. (2015). The effects of mortality on fertility: Population dynamics after a natural disaster. Demography, 52, 15–38.
On Saturday, the Brazilian health ministry said the link between Zika and birth defects was unprecedented anywhere in the world. (2015, December 1). Retrieved from https://www.bbc.com/news/world-latin-america-34960818
Oriá, M. O. B., Ximenes, L. B., de Almeida, P. C., Glick, D. F., & Dennis, C. L. (2009). Psychometric assessment of the Brazilian version of the Breastfeeding Self-Efficacy Scale. Public Health Nursing, 26, 574–583.
Pan American Health Organization (PAHO)/World Health Organization (WHO). (2015a, May 14). Confirmada a circulação do vírus Zika no Brasil [Circulation of the Zika virus is confirmed in Brazil]. Brasília, DF, Brasil: PAHO/WHO. Retrieved from https://www.paho.org/bra/index.php?option=com_content&view=article&id=4838:confirmada-a-circulacao-do-zika-virus-no-brasil&Itemid=812
Pan American Health Organization (PAHO)/World Health Organization (WHO). (2015b, May 7). Epidemiological alert: Zika virus infection. Washington, DC: PAHO/WHO. Retrieved from https://www.paho.org/hq/dmdocuments/2015/2015-may-7-cha-zika-virus-epi-alert.pdf
Pan American Health Organization (PAHO)/World Health Organization (WHO). (2015c, November 17). Epidemiological alert: Increase of microcephaly in the northeast of Brazil. Washington, DC: PAHO/WHO. Retrieved from https://www.paho.org/hq/dmdocuments/2015/2015-nov-17-cha-microcephaly-epi-alert.pdf
Pan American Health Organization (PAHO)/World Health Organization (WHO). (2016, February 1). WHO announces a public health emergency of international concern. Washington, DC: PAHO/WHO. Retrieved from https://www.paho.org/hq/index.php?option=com_content&view=article&id=11640:2016-who-statement-on-1st-meeting-ihr-2005-emergency-committee-on-zika-virus&Itemid=135&lang=en
Potter, J., Schmertmann, C., Assunção, R., & Cavenaghi, S. (2010). Mapping the timing, pace, and scale of the fertility transition in Brazil. Population and Development Review, 36, 283–307.
Preston, S. H., Heuveline, P., & Guillot, M. (2001). Demography: Measuring and modeling population processes. Malden, MA: Blackwell.
Pulerwitz, J., & Barker, G. (2008). Measuring attitudes toward gender norms among young men in Brazil: Development and psychometric evaluation of the GEM Scale. Men and Masculinities, 10, 322–338.
Rabe-Hesketh, S., & Skrondal, A. (2012). Multilevel and longitudinal modeling using Stata (Vol. II, Categorical responses, counts and survival, 3rd ed.). College Station, TX: Stata Press.
Rangel, M. A., Nobles, J., & Hamoudi, A. (Forthcoming). Brazil’s missing infants: Zika risk changes reproductive behavior. Demography.
Rios-Neto, E., Miranda-Ribeiro, A., & Miranda-Ribeiro, P. (2018). Fertility differentials by education in Brazil: From the conclusion of fertility to the onset of postponement transition. Population and Development Review, 44, 489–517.
Rodriguez, J., & Cavenaghi, S. (2017, October–November). Unintended fertility among Latin American adolescents: A growing trend across all socioeconomic groups. Paper presented at the International Population Conference, Cape Town, South Africa. Retrieved from https://iussp.confex.com/iussp/ipc2017/meetingapp.cgi/Paper/1845
Schuck-Paim, C., López, D., Simonsen, L., & Alonso, W. (2016). Unintended pregnancies in Brazil: A challenge for the recommendation to delay pregnancy due to Zika. PLoS Currents, 16(8). https://doi.org/10.1371/currents.outbreaks.7038a6813f734c1db547240c2a0ba291
Silva, K. C., Rosa, M. L. G., Moyses, N., Afonso, L. A., Oliveira, L. H. S., & Cavalcanti, S. M. B. (2009). Risk factors associated with human papillomavirus infection in two populations from Rio de Janeiro, Brazil. Memórias do Instituto Oswaldo Cruz, 104, 885–891.
Sims, A. (2015, November 19). Zika virus: Health alerts in South America and Caribbean following fears illness may cause birth deformities: Doctors believe the illness may be linked to a rise in cases of microcephaly in infants. The Independent. Retrieved from https://www.independent.co.uk/news/world/americas/health-alerts-in-south-america-and-caribbean-following-fears-spreading-zika-virus-may-cause-birth-a6740301.html
Singh, S., & Wulf, D. (1991). Estimating abortion levels in Brazil, Colombia and Peru, using hospital admissions and fertility survey data. International Family Planning Perspectives, 17, 8–13, 24.
Siqueira, J., Martelli, C. M., Maciel, I. J., & Oliveira, R., Ribeiro, M. G., Amorim, F. P., . . . Andrade, A. L. (2004). Household survey of dengue infection in central Brazil: Spatial point pattern analysis and risk factors assessment. American Journal of Tropical Medicine and Hygiene, 71, 646–651.
Sobotka, T., Skirbekk, V., & Philipov, D. (2011). Economic recession and fertility in the developed world. Population and Development Review, 37, 267–306.
Szwarcwald, C. L., Barbosa-Júnior, A., Pascom, A. R., & de Souza-Júnior, P. R. (2005). Knowledge, practices and behaviours related to HIV transmission among the Brazilian population in the 15–54 years age group, 2004. AIDS, 19(Suppl. 4), S51–S58.
Szwarcwald, C. L., de Frias, P. G., Júnior, P. R., da Silva de Almeida, W., & Neto, O. L. (2014). Correction of vital statistics based on a proactive search of deaths and live births: Evidence from a study of the North and Northeast regions of Brazil. Population Health Metrics, 12, 16. https://doi.org/10.1186/1478-7954-12-16
Trinitapoli, J., & Yeatman, S. (2011). Uncertainty and fertility in a generalized AIDS epidemic. American Sociological Review, 76, 935–954.
Vrachnis, N., Vlachadis, N., Iliodromiti, Z., Vlachadi, M., & Creatsas, G. (2014). Greece’s birth rates and the economic crisis. Lancet, 383, 692–693.
World Bank. (2018). Data: Brazil [Dataset]. Washington DC: World Bank. Retrieved from https://data.worldbank.org/country/Brazil
World Health Organization (WHO). (2019). Zika epidemiological update. Geneva, Switzerland: WHO. Retrieved from https://www.who.int/emergencies/diseases/zika/zika-epidemiology-update-july-2019.pdf?ua=1
Zanluca, C., de Melo, V. C. A., Mosimann, A. L. P., dos Santos, G. I. V., dos Santos, C. N. D., & Luz, K. (2015). First report of autochthonous transmission of Zika virus in Brazil. Memórias do Instituto Oswaldo Cruz, 110, 569–572.
Acknowledgments
This research was funded by grant R01HD091257, Reproductive Responses to the Zika Virus Epidemic in Brazil, awarded to PI L. J. Marteleto by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. This research was also supported by grant P2CHD042849, Population Research Center, awarded to the PRC at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and Grants 431872/2016-3, 314392/2018-1, and CSA-APQ-01553-16 awarded to Gilvan Guedes by the Brazilian Technological and Scientific Development Council (CNPq) and by the Minas Gerais Research Foundation (FAPEMIG). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the CNPq. Raquel Z. Coutinho gratefully acknowledges support from the Universidade Federal de Minas Gerais (Edital 11/2017 - ADRC - Programa Institucional de Auxílio à Pesquisa de Docentes Recém-Contratados ou Recém-Doutorados da UFMG). The authors thank Júlia Almeida Calazans, John Casterline, Suzana Cavenaghi, Diane Coffey, Samantha Haussmann, Ana Maria Hermeto C. De Oliveira, Kristine Hopkins, Bernardo Lanza, Vanessa di Lego, Sandra Valongueiro, Joe Potter, Laura Wong, the anonymous reviewers, and Editors for their helpful comments at different stages of this research. We also thank Márcia Castro for discussions on the ZIKV epidemic early on in this research. We also thank the participants of the PRC (UTexas), CCPR (UCLA), and CPC (UNC) brown bags for their helpful suggestions.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 286 kb)
Rights and permissions
About this article
Cite this article
Marteleto, L.J., Guedes, G., Coutinho, R.Z. et al. Live Births and Fertility Amid the Zika Epidemic in Brazil. Demography 57, 843–872 (2020). https://doi.org/10.1007/s13524-020-00871-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13524-020-00871-x