Abstract
Background and purpose
Previous studies have revealed a relationship between chronic kidney disease (CKD) and white matter hyperintensities (WMH). However, studies on the WMH and CKD in acute stroke patients are rare, and the conclusion is consistent. Our study aimed to investigate the relationship between the severity of WMH and CKD in acute lacunar infarction patients.
Methods
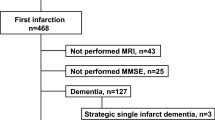
Consecutive acute lacunar infarction patients were recruited in this cross-sectional study. All patients were divided into two groups according to the severity of periventricular WMH (PVWMH) and deep WMH (DWMH). We dichotomized the severity of WMH (PVWMH and DWMH, separately) into mild group (Fazekas scores 0–1) and moderate-severe group (Fazekas scores 2–3). Estimated glomerular filtration rate (eGFR), proteinuria, vascular risk factors, and clinical features were compared between these two groups. Multivariable logistic regression analysis was used to investigate the association between the severity of WMH and risk factors.
Results
A total of 993 acute lacunar infarction patients aged 25–95 years were enrolled. The proportions of participants presenting moderate-severe group PVWMH and DWMH were 46.6% and 38.6%, respectively. Patients with moderate-severe PVWMH had higher age (P < 0.001) and higher incidence of stroke history (P < 0.001) than those in mild group. The level of serum creatinine and the presence of CKD were significantly higher while the eGFR was significantly lower in patients with moderate-severe PVWMH than those with mild PVWMH. Patients with moderate-severe DWMH (n = 383) also had higher age (P < 0.001) and often had a history of stroke (P < 0.001). But the association between the severity of DWMH and eGFR was not found. Multivariable logistic regression analyses showed stage 2 CKD and stage 3 CKD were independently associated with moderate-severe PVWMH, but not DWMH.
Conclusions
Our study demonstrates that CKD was independently associated with moderate-severe PVWMH in patients with acute lacunar infarction, but not DWMH. PVWMH and DWMH may have distinct pathophysiology.
Similar content being viewed by others
References
Wardlaw JM, Smith C, Dichgans M (2019) Small vessel disease: mechanisms and clinical implications. Lancet Neurol 18:684–696
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, Lindley RI, O'Brien JT, Barkhof F, Benavente OR, Black SE, Brayne C, Breteler M, Chabriat H, Decarli C, de Leeuw FE, Doubal F, Duering M, Fox NC, Greenberg S, Hachinski V, Kilimann I, Mok V, Oostenbrugge Rv, Pantoni L, Speck O, Stephan BC, Teipel S, Viswanathan A, Werring D, Chen C, Smith C, van Buchem M, Norrving B, Gorelick PB, Dichgans M, STandards for ReportIng Vascular changes on nEuroimaging (STRIVE v1) (2013) Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 12:822–838
Pantoni L (2010) Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol 9:689–701
Toyoda K (2015) Cerebral small vessel disease and chronic kidney disease. J Stroke 17:31–37
Lau WL, Huisa BN, Fisher M (2017) The cerebrovascular-chronic kidney disease connection: perspectives and mechanisms. Transl Stroke Res 8:67–76
Makin SDJ, Cook FAB, Dennis MS, Wardlaw JM (2015) Cerebral small vessel disease and renal function: systematic review and meta-analysis. Cerebrovasc Dis 39:39–52
Zhang L, Wang F, Wang L, Wang W, Liu B, Liu J, Chen M, He Q, Liao Y, Yu X, Chen N, Zhang JE, Hu Z, Liu F, Hong D, Ma L, Liu H, Zhou X, Chen J, Pan L, Chen W, Wang W, Li X, Wang H (2012) Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet 379:815–822
Ito S, Nagasawa T, Abe M, Mori T (2009) Strain vessel hypothesis: a viewpoint for linkage of albuminuria and cerebro-cardiovascular risk. Hypertens Res 32:115–121
Peng Q, Sun W, Liu W, Liu R, Huang Y (2016) Longitudinal relationship between chronic kidney disease and distribution of cerebral microbleeds in patients with ischemic stroke. J Neurol Sci 362:1–6
Shima H, Ishimura E, Naganuma T, Ichii M, Yamasaki T, Mori K, Nakatani T, Inaba M (2011) Decreased kidney function is a significant factor associated with silent cerebral infarction and periventricular hyperintensities. Kidney Blood Press Res 34:430–438
Oksala NK, Salonen T, Strandberg T, Oksala A, Pohjasvaara T, Kaste M, Karhunen PJ, Erkinjuntti T (2010) Cerebral small vessel disease and kidney function predict long-term survival in patients with acute stroke. Stroke 41:1914–1920
Ikram MA, Vernooij MW, Hofman A, Niessen WJ, van der Lugt A, Breteler MM (2008) Kidney function is related to cerebral small vessel disease. Stroke 39:55–61
Khatri M, Wright CB, Nickolas TL, Yoshita M, Paik MC, Kranwinkel G, Sacco RL, DeCarli C (2007) Chronic kidney disease is associated with white matter hyperintensity volume: the Northern Manhattan Study (NOMAS). Stroke 38:3121–3126
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Abdelrasoul AA, Elsebaie NA, Gamaleldin OA, Khalifa MH, Razek AAKA (2019) Imaging of brain infarctions: beyond the usual territories. J Comput Assist Tomogr 43:443–451
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA (1987) MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol 149:351–356
Zong LX, Yao M, Ni J, Zhou LX, Yuan J et al (2016) Kidney function is associated with severity of white matter hyperintensity in patients with acute ischemic stroke/TIA. BMC Neurol 16:6
Jeon JW, Jeong HS, Choi DE, Ham YR, Na KR et al (2017) Prognostic relationships between microbleed, lacunar infarction, white matter lesion, and renal dysfunction in acute ischemic stroke survivors. J Stroke Cerebrovasc Dis 26:385–392
Markus HS, Lythgoe DJ, Ostegaard L, O’Sullivan M, Williams SC (2000) Reduced cerebral blood flow in white matter in ischaemic leukoaraiosis demonstrated using quantitative exogenous contrast based perfusion MRI. J Neurol Neurosurg Psychiatry 69:48–53
Vernooij MW, van der Lugt A, Ikram MA, Wielopolski PA, Vrooman HA, Hofman A, Krestin GP, Breteler MM (2008) Total cerebral blood flow and total brain perfusion in the general population: the Rotterdam Scan Study. J Cereb Blood Flow Metab 28:412–419
Arba F, Mair G, Carpenter T et al (2017) Cerebral white matter hypoperfusion increases with small-vessel disease burden. Data from the third international stroke trial. J Stroke Cerebrovasc Dis 26:1506–1513
Yang S, Cai J, Lu R, Wu J, Zhang M, Zhou X (2017) Association between serum cystatin C level and total magnetic resonance imaging burden of cerebral small vessel disease in patients with acute lacunar stroke. J Stroke Cerebrovasc Dis 26:186–191
Gao Y, Wei S, Song B, Qin J, Fang H et al (2015) Homocysteine level is associated with white matter hyperintensity locations in patients with acute ischemic stroke. PLoS One 10:e0144431
Xiao L, Lan W, Sun W, Dai Q, Xiong Y et al (2015) Chronic kidney disease in patients with lacunar stroke: association with enlarged perivascular spaces and total magnetic resonance imaging burden of cerebral small vessel disease. Stroke 46:2081–2086
Vilar-Bergua A, Riba-Llena I, Ramos N, Mundet X, Espinel E et al (2016) Microalbuminuria and the combination of MRI markers of cerebral small vessel disease. Cerebrovasc Dis 42:66–72
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The design of this study was approved by the Ethics Committee of Beijing Chao-Yang Hospital, Capital Medical University.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 29 kb).
Rights and permissions
About this article
Cite this article
Yang, L., Yu, L., Kong, Y. et al. Relationship between white matter hyperintensities and chronic kidney disease in patients with acute lacunar stroke. Neurol Sci 41, 3307–3313 (2020). https://doi.org/10.1007/s10072-020-04397-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04397-3