Abstract
Purpose
The main purpose is to compare the characteristics and performance of a centrifugal blood pump with and without center post. Furthermore, to propose a center post design guide for the development of centrifugal blood pumps: finding the appropriate height and diameter of the center post.
Methods
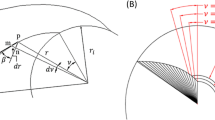
A centrifugal blood pump with different center post configurations is investigated using Computational Fluid Dynamics (CFD) in an extensive parametric approach. Height and diameter of the center post are varied on 4 levels each. Pressure head and hydraulic efficiency curves, pressure and velocity contours and volumetric histograms of scalar shear stress (SSS) distribution are discussed in detail.
Results
The simulation results show uniform pressure distribution around the casing in the baseline design. Although obtaining the minimum Normalized Index of Hemolysis (NIH), average scalar shear stress (ASSS), and volumetric percentage ratios (SSS > 9, 50 and 150 Pa), a stagnation and recirculation zone in the impeller eye above the casing bottom is detected in center post free (H = 0 mm) pump. With the establishment and further increase of the center post height, the stagnation zone disappears gradually. The results also indicate that flow recirculation and stagnation around the circumference of the center post occurs when the center post has a small diameter. As the diameter increases, a reversed flow is formed between the impeller and the center post.
Conclusions
The center post can greatly reduce the stagnation zone occurring in the center post free pump. The diameter of center post makes a difference to the flow field in the gap between the impeller and the center post.















Similar content being viewed by others
References
ANSYS FLUENT Theory Guide, 16th Ed. Canonsburg, PA: Ansys Fluent, Inc., 2014.
ASTM F1841-97. Standard Practice for Assessment of Hemolysis in Continuous Flow Blood Pumps. West Conshohocken: ASTM International, 2017. https://doi.org/10.1520/F1841-97R17.
Benjamin, E. J., S. S. Virani, C. W. Callaway, A. R. Chang, S. Cheng, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation 137(12):67–492, 2018.
Berk, Z. B. K., J. Zhang, Z. Chen, D. Tran, B. P. Griffith, and Z. J. Wu. Evaluation of in vitro hemolysis and platelet activation of a newly developed maglev LVAD and two clinically used LVADs with human blood. Artif. Organs 43:1–10, 2019.
Drazner, M. H. A new left ventricular assist device—better, but still not ideal. N. Engl. J. Med. 378(15):1442–1443, 2018.
Fraser, K. H., T. Zhang, M. E. Taskin, B. P. Griffith, and Z. J. Wu. A quantitative comparison of mechanical blood damage parameters in rotary ventricular assist devices: shear stress, exposure time and hemolysis index. J. Biomech. Eng. 134:081002, 2012.
Fukamachi, K., D. J. Horvath, N. Byram, et al. Advanced ventricular assist device with pulse augmentation and automatic regurgitant-flow shut-off. J. Heart Lung Transplant. 35:1519, 2016.
Garon, A., and M. I. Farinas. Fast three-dimensional numerical hemolysis approximation. Artif. Organs 28:1016–1025, 2004.
Giersiepen, M., L. Wurzinger, R. Opitz, and H. Reul. Estimation of shear stress-related blood damage in heart valve prostheses—in vitro comparison of 25 aortic valves. Int. J. Artif. Organs 13:300–306, 1990.
Giridharan, G. A., C. Lederer, A. Berthe, L. Goubergrits, J. Hutzenlaub, M. S. Slaughter, R. D. Dowling, P. A. Spence, and S. C. Koenig. Flow dynamics of a novel counterpulsation device characterized by CFD and PIV modeling. Med. Eng. Phys. 33(10):1193–1202, 2011.
Legendre, D., P. Antunes, E. Bock, A. Andrade, J. F. Biscegli, and J. P. Ortiz. Computational fluid dynamics investigation of a centrifugal blood pump. Artif. Organs 32(4):342–348, 2007.
Lena, W., T. Bente, D. de Zelicourt, G. Marcus, B. Stefan, S. D. Marianne, S. D. Marianne, M. Mirko, and K. Vartan. Fluid dynamics in the HeartMate 3: influence of the artificial pulse feature and residual cardiac pulsation. Artif. Organs 43:363–376, 2018.
Li, D., Q. Y. Wu, J. J. Ji, S. H. Liu, M. K. Zhang, and Y. Zhang. Hemolysis in a continuous-flow ventricular assist device with/without chamfer. Adv. Mech. Eng. 2017. https://doi.org/10.1177/1687814017697894.
Kido, K., H. Hoshi, N. Watanabe, H. Kataoka, K. Ohuchi, J. Asama, T. Shinshi, M. Yoshikawa, and S. Takatani. Computational fluid dynamics analysis of the pediatric tiny centrifugal blood pump (TinyPump). Artif. Organs 30(5):392–399, 2005.
Mechanical Circulatory and Respiratory Support, Chapter 5: 151–186, 2018.
Mehra, M. R., Y. Naka, N. Uriel, D. J. Goldstein, J. C. Cleveland, P. C. Colombo, et al. A fully magnetically levitated circulatory pump for advanced heart failure. N. Engl. J. Med. 376:440–450, 2017.
Mozafari, S., M. A. Rezaienia, G. M. Paul, et al. The effect of geometry on the efficiency and hemolysis of centrifugal implantable blood pumps. ASAIO J. 63(1):53–59, 2017.
Murashige, T., and W. Hijikata. Mechanical antithrombogenic properties by vibrational excitation of the impeller in a magnetically levitated centrifugal blood pump. Artif. Organs 43:849–859, 2019.
Najjar, S. S., M. S. Slaughter, F. D. Pagani, R. C. Starling, E. C. McGee, P. Eckman, et al. An analysis of pump thrombus events in patients in the HeartWare advance bridge to transplant and continued access protocol trial. J. Heart Lung Transplant. 33:23–34, 2014.
Netuka, I., P. Sood, Y. Pya, D. Zimpfer, T. Krabatsch, J. Garbade, et al. Fully magnetically levitated left ventricular assist system for treating advanced HF. J. Am. Coll. Cardiol. 66:2579–2589, 2015.
Nishida, M., N. Kento, S. Daisuke, K. Ryo, M. Osamu, K. Yasuo, K. Katsuyuki, and Y. Takashi. Effect of impeller geometry on lift-off characteristics and rotational attitude in a monopivot centrifugal blood pump. Artif. Organs 40(6):89–101, 2016.
Rezaienia, M. A., G. Paul, E. Avital, et al. Computational parametric study of the axial and radial clearances in a centrifugal rotary blood pump. ASAIO J. 64(5):643–650, 2018.
Santambrogio, L., T. Bianchi, M. Fuardo, F. Gazzoli, A. Braschi, M. Maurelli, and R. Veronesi. Right ventricular failure after left ventricular assist device insertion: preoperative risk factors. Interact. Cardiovasc. Thorac. Surg. 5:379–382, 2006.
Sawa, Y. Current status of third-generation implantable left ventricular assist devices in Japan, duraheart and heartware. Surg. Today 45(6):672–681, 2015.
Song, X., H. G. Wood, and D. Olsen. Computational fluid dynamics (CFD) study of the 4th generation prototype of a continuous flow ventricular assist device (VAD). J. Biomech. Eng. 126(2):180–187, 2004.
Taskin, M. E., K. H. Fraser, T. Zhang, G. Barry, F. Andi, and K. A. Dasse. Computational characterization of flow and hemolytic performance of the Ultramag blood pump for circulatory support. Artif. Organs 34(12):1099–1113, 2010.
Taskin, M. E., K. H. Fraser, T. Zhang, et al. Evaluation of Eulerian and Lagrangian Models for Hemolysis Estimation. ASAIO J. 58(4):363–372, 2012.
Thamsen, B., B. Blumel, J. Schaller, C. O. Paschereit, K. Affeld, and L. Goubergrits. Numerical analysis of blood damage potential of the HeartMate ii and HeartWare HAVD rotary blood pumps. Artif. Organs 39(8):651–659, 2015.
Thamsen, B., M. Plamondon, M. Granegger, et al. Investigation of the axial gap clearance in a hydrodynamic-passive magnetically levitated rotary blood pump using X-ray radiography. Artif. Organs 42:510, 2018.
van Valen, R., H. M. Zuijdendorp, and O. Birim. Challenges in destination LVAD therapy, management of mediastinitis and device infection, a case report. Heart, Lung Circ. 27:e7, 2015.
Wiegmann, L., S. Boes, et al. Blood pump design variations and their influence on hydraulic performance and indicators of hemocompatibility. Ann. Biomed. Eng. 46(3):417–428, 2017.
Wu, J., B. E. Paden, H. S. Borovetz, and J. F. Antaki. Computational fluid dynamics analysis of blade tip clearances on hemodynamic performance and blood damage in a centrifugal ventricular assist device. Artif. Organs 34:402–411, 2009.
Wu, W. T., F. Yang, J. C. Wu, N. Aubry, M. Massoudi, and J. F. Antaki. High fidelity computational simulation of thrombus formation in Thoratec HeartMate II continuous flow ventricular assist device. Sci. Rep. 6(1):38025, 2016.
Yu, H., S. Engel, G. Janiga, and D. Thevenin. A review of hemolysis prediction models for computational fluid dynamics. Artif. Organs 41(7):603–621, 2017.
Zhang, J., P. Zhang, K. H. Fraser, B. P. Griffith, and Z. J. Wu. Comparison and experimental validation of fluid dynamic numerical models for a clinical ventricular assist device. Artif. Organs 37(4):380–389, 2013.
Acknowledgments
The work described in this paper was supported by the Shenzhen Science and Technology Innovation Foundation (Grant Nos. JCYJ20160427184134564, JCYJ20170811154117143) and the National Natural Science Foundation of China (Grant No. 51675121).
Conflict of interest
The authors have declared no conflicts of interest for this article.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Scott C Corbett oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fang, P., Du, J. & Yu, S. Effect of the Center Post Establishment and Its Design Variations on the Performance of a Centrifugal Rotary Blood Pump. Cardiovasc Eng Tech 11, 337–349 (2020). https://doi.org/10.1007/s13239-020-00464-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-020-00464-0