Abstract
Purpose
To examine associations of KRAS mutation with tumor deposit status and overall survival in colorectal cancer (CRC) patients.
Methods
This retrospective cohort study included patients with incidental CRC diagnosed during 2010–2014 and recorded statuses of KRAS and tumor deposit in the National Cancer Database of the USA. Multivariable logistic regression and time-varying Cox regression analyses were used.
Results
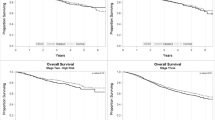
We included 45,761 CRC patients with KRAS status (24,027 [52.5%] men, 24,240 [53.0%] < 65 years old, 17,338 [37.9%] with KRAS mutation). Adjusted for microsatellite instability, age, pathologic stage and tumor grade, KRAS mutation (versus wild type) was associated with tumor deposit presence (odds ratio = 1.11, 95% CI 1.02–1.20). KRAS mutation was also linked to worse overall survival of CRC patients regardless of tumor deposit status (adjusted Hazard ratio [HR] = 1.20, 95% CI 1.07–1.33 for CRC with tumor deposits, and adjusted HR = 1.24, 95% CI 1.14–1.35 or CRC without) or tumor stage (adjusted HR = 1.32, 95% CI 1.14–1.54 for early-stage and adjusted HR = 1.18, 95% CI 1.10–1.27 for late-stage). Microsatellite instability was associated with better overall survival in CRC without tumor deposit (adjusted HR = 0.89, 95% CI 0.79–0.99), but not in CRC with tumor deposit (adjusted HR = 1.12, 95% CI 0.97–1.30).
Conclusion
KRAS mutation is independently associated with tumor deposit presence and a worse overall survival in CRC patients.

Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70:7–30
Andreyev HJ, Norman AR, Cunningham D, Oates JR, Clarke PA (1998) Kirsten ras mutations in patients with colorectal cancer: the multicenter "RASCAL" study. J Natl Cancer Inst 90:675–684
De Roock W, Claes B, Bernasconi D et al (2010) Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol 11:753–762
Finkelstein SD, Sayegh R, Christensen S, Swalsky PA (1993) Genotypic classification of colorectal adenocarcinoma. Biologic behavior correlates with K-ras-2 mutation type. Cancer 71:3827–3838
McDermott U, Longley DB, Johnston PG (2002) Molecular and biochemical markers in colorectal cancer. Ann Oncol 13(Suppl 4):235–245
Nagata Y, Abe M, Kobayashi K et al (1990) Glycine to aspartic acid mutations at codon 13 of the c-Ki-ras gene in human gastrointestinal cancers. Cancer Res 50:480–482
Shaw P, Tardy S, Benito E, Obrador A, Costa J (1991) Occurrence of Ki-ras and p53 mutations in primary colorectal tumors. Oncogene 6:2121–2128
NCCN (2018) NCCN Clinical Practice Guidelines in Oncology: Colon cancer v1.2018. National Comprehensive Cancer Network
Maughan TS, Adams RA, Smith CG et al (2011) Addition of cetuximab to oxaliplatin-based first-line combination chemotherapy for treatment of advanced colorectal cancer: results of the randomised phase 3 MRC COIN trial. Lancet 377:2103–2114
Roth AD, Tejpar S, Delorenzi M et al (2010) Prognostic role of KRAS and BRAF in stage II and III resected colon cancer: results of the translational study on the PETACC-3, EORTC 40993, SAKK 60-00 trial. J Clin Oncol 28:466–474
Ogino S, Meyerhardt JA, Irahara N et al (2009) KRAS mutation in stage III colon cancer and clinical outcome following intergroup trial CALGB 89803. Clin Cancer Res 15:7322–7329
Song JS, Chang HJ, Kim DY et al (2011) Is the N1c category of the new American Joint Committee on cancer staging system applicable to patients with rectal cancer who receive preoperative chemoradiotherapy? Cancer 117:3917–3924
Amin MB, Greene FL, Edge SB et al (2017) The Eighth Edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin 67:93–99
Puppa G, Maisonneuve P, Sonzogni A et al (2007) Pathological assessment of pericolonic tumor deposits in advanced colonic carcinoma: relevance to prognosis and tumor staging. Modern Pathol 20:843–855
Lo DS, Pollett A, Siu LL, Gallinger S, Burkes RL (2008) Prognostic significance of mesenteric tumor nodules in patients with stage III colorectal cancer. Cancer 112:50–54
Mayo E, Llanos AA, Yi X, Duan SZ, Zhang L (2016) Prognostic value of tumor deposit and perineural invasion status in colorectal cancer patients: a SEER-based population study. Histopathology 69:230–238
Chavali LB, Llanos AAM, Yun JP, Hill SM, Tan XL, Zhang L (2017) Radiotherapy for patients with resected tumor deposit-positive colorectal cancer. Arch Pathol Lab Med. Epub ahead of print
Boffa DJ, Rosen JE, Mallin K et al (2017) Using the National Cancer Database for outcomes research: a review. JAMA Oncol 3:1722–1728
Shaikh T, Handorf EA, Meyer JE, Hall MJ, Esnaola NF (2018) Mismatch repair deficiency testing in patients with colorectal cancer and nonadherence to testing guidelines in young adults. JAMA Oncol 4:e173580
Pezzi TA, Schwartz DL, Mohamed ASR et al (2018) Barriers to combined-modality therapy for limited-stage small cell lung cancer. JAMA Oncol 4:e174504
Joshi SS, Handorf E, Strauss D et al (2018) Treatment trends and outcomes for patients with lymph node-positive cancer of the penis. JAMA Oncol 4:643–649
Goodman CR, Seagle BL, Friedl TWP et al (2018) Association of circulating tumor cell status with benefit of radiotherapy and survival in early-stage breast cancer. JAMA Oncol 4:e180163
Adam MA, Turner MC, Sun Z et al (2018) The appropriateness of 30-day mortality as a quality metric in colorectal cancer surgery. Am J Surg 215:66–70
Sargent DJ, Marsoni S, Monges G et al (2010) Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer. J Clin Oncol 28:3219–3226
Prabhudesai A, Arif S, Finlayson CJ, Kumar D (2003) Impact of microscopic extranodal tumor deposits on the outcome of patients with rectal cancer. Dis Colon Rectum 46:1531–1537
Tateishi S, Arima S, Futami K et al (2005) A clinicopathological investigation of "tumor nodules" in colorectal cancer. Surg Today 35:377–384
Yamano T, Semba S, Noda M et al (2015) Prognostic significance of classified extramural tumor deposits and extracapsular lymph node invasion in T3–4 colorectal cancer: a retrospective single-center study. BMC Cancer 15:859
Nagayoshi K, Ueki T, Nishioka Y et al (2014) Tumor deposit is a poor prognostic indicator for patients who have stage II and III colorectal cancer with fewer than 4 lymph node metastases but not for those with 4 or more. Dis Colon Rectum 57:467–474
Simanshu DK, Nissley DV, McCormick F (2017) RAS proteins and their regulators in human disease. Cell 170:17–33
Lockhart AC, Berlin JD (2005) The epidermal growth factor receptor as a target for colorectal cancer therapy. Semin Oncol 32:52–60
Ciardiello F, Tortora G (2001) A novel approach in the treatment of cancer: targeting the epidermal growth factor receptor. Clin Cancer Res 7:2958–2970
Hutchins G, Southward K, Handley K et al (2011) Value of mismatch repair, KRAS, and BRAF mutations in predicting recurrence and benefits from chemotherapy in colorectal cancer. J Clin Oncol 29:1261–1270
Van Cutsem E, Cervantes A, Adam R et al (2016) ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol 27:1386–1422
Jover R, Zapater P, Castells A et al (2006) Mismatch repair status in the prediction of benefit from adjuvant fluorouracil chemotherapy in colorectal cancer. Gut 55:848–855
Zaanan A, Shi Q, Taieb J et al (2018) Role of deficient DNA mismatch repair status in patients with stage iii colon cancer treated with FOLFOX adjuvant chemotherapy: a pooled analysis from 2 randomized clinical trials. JAMA Oncol 4:379–383
Sinicrope FA, Foster NR, Thibodeau SN et al (2011) DNA mismatch repair status and colon cancer recurrence and survival in clinical trials of 5-fluorouracil-based adjuvant therapy. J Natl Cancer Inst 103:863–875
Acknowledgments
The study was in part supported by an Initiative for Multidisciplinary Research Teams (IMRT) award from Rutgers University, Newark, NJ (to N.G. and L.Z.), the U.S. National Institute of Health (R01 AT010243 to N.G.), the National Natural Science Foundation of China (No. 81872387 to M.Z.) and China Scholarship Council (to M.Z.). The funders have no roles in the study design or manuscript preparation.
Author information
Authors and Affiliations
Contributions
MZ, NG, JY, and LZ designed the study, LZ extracted the data, MZ, WH, and LZ analyzed the data, MZ and LZ wrote the first draft of the manuscript. The final draft has been edited and approved by all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
We cannot share the patient-level data which are confidential and were obtained with review and approval from the National Cancer Database and the American College of Surgeons.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The work has been deposited to medRxiv as a preprint, with citation of medRxiv 19003210; https://doi.org/10.1101/19003210.
Rights and permissions
About this article
Cite this article
Zhang, M., Hu, W., Hu, K. et al. Association of KRAS mutation with tumor deposit status and overall survival of colorectal cancer. Cancer Causes Control 31, 683–689 (2020). https://doi.org/10.1007/s10552-020-01313-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-020-01313-0