Abstract
Purpose
The primary objective of this study was to quantify the variations of the medial posterior tibial slope (MPTS) and the lateral posterior tibial slope (LPTS), as well as of the medial proximal tibial angle (MPTA), and to determine the fraction of patients for which standard techniques including different alignment techniques would result in alteration of the patient’s individual posterior tibial slope (PTS) and MPTA. Furthermore, it was of interest if a positive correlation between PTS and MPTA or between medial and lateral slope exists.
Methods
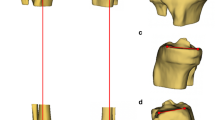
A retrospective study was performed on CT-scans of 234 consecutively selected European patients undergoing individual total knee replacement. All measurements were done on three-dimensional CAD models, which were generated on the basis of individual CT-scans, including the hip, knee, and ankle center. Measurements included the medial and lateral PTS and the MPTA. PTS was measured as the angle between the patient’s articular surface and a plane perpendicular to the mechanical axis of the tibia in the sagittal plane. MPTA was defined as the angle between the tibial mechanical axis and the proximal articular surface of the tibia in the coronal plane.
Results
Analysis revealed a wide variation of the MPTS, LPTS, and MPTA among the patients. MPTS and LPTS varied significantly both interindividually and intraindividually. The range of PTS was up to 20° for MPTS (from − 4.3° to 16.8°) and for LPTS (from − 2.9 to 17.2°). The mean intraindividual difference between MPTS and LPTS in the same knee was 2.6° (SD 2.0) with a maximum of 9.5°. MPTA ranged from 79.8 to 92.1° with a mean of 86.6° (SD ± 2.4). Statistical analysis revealed a weak positive correlation between MPTA and MPTS.
Conclusion
The study demonstrates a huge interindividual variability in PTS and MPTA as well as significant intraindividual differences in MPTS and LPTS. Therefore, the question arises, whether the use of standard techniques, including fixed PTSs and MPTAs, is sufficient to address every single patient’s individual anatomy.
Level of evidence
III.





Similar content being viewed by others
Abbreviations
- PTS:
-
Posterior tibial slope
- MPTS:
-
Medial posterior tibial slope
- LPTS:
-
Lateral posterior tibial slope
- MPTA:
-
Medial proximal tibial angle
- TKA:
-
Total knee arthroplasty
- UKA:
-
Unicondylar knee arthroplasty
References
Bellemans J, Robijns F, Duerinckx J, Banks S, Vandenneucker H (2005) The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 13:193–196
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG (2014) A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Jt J 96:907–913
Haddad B, Konan S, Mannan K, Scott G (2012) Evaluation of the posterior tibial slope on MR images in different population groups using the tibial proximal anatomical axis. Acta Orthop Belg 78:757–763
Hashemi J, Chandrashekar N, Gill B, Beynnon BD, Slauterbeck JR, Schutt RC, Mansouri H, Dabezies E (2008) The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Jt Surg Am 90:2724–2734
Hess S, Moser LB, Amsler F, Behrend H, Hirschmann MT (2019) Highly variable coronal tibial and femoral alignment in osteoarthritic knees: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:1368–1377
Hirschmann MT, Hess S, Behrend H, Amsler F, Leclercq V, Moser LB (2019) Phenotyping of hip-knee-ankle angle in young non-osteoarthritic knees provides better understanding of native alignment variability. Knee Surg Sports Traumatol Arthrosc 27:1378–1384
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402
Innocenti B, Pianigiani S, Ramundo G, Thienpont E (2016) Biomechanical effects of different varus and valgus alignments in medial unicompartmental knee arthroplasty. J Arthroplasty 31:2685–2691
Matsumoto T, Takayama K, Ishida K, Hayashi S, Hashimoto S, Kuroda R (2017) Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Jt J 99:640–646
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Nunley RM, Nam D, Johnson SR, Barnes CL (2014) Extreme variability in posterior slope of the proximal tibia: measurements on 2395 CT scans of patients undergoing UKA? J Arthroplasty 29:1677–1680
Okamoto S, Mizu-uchi H, Okazaki K, Hamai S, Nakahara H, Iwamoto Y (2015) Effect of tibial posterior slope on knee kinematics, quadriceps force, and patellofemoral contact force after posterior-stabilized total knee arthroplasty. J Arthroplasty 30:1439–1443
Parvizi J, Nunley RM, Berend KR, Lombardi AV, Ruh EL, Clohisy JC, Hamilton WG, Della Valle CJ, Barrack RL (2014) High level of residual symptoms in young patients after total knee arthroplasty. Clin Orthop Relat Res 472:133–137
Thienpont E, Bellemans J, Victor J, Becker R (2013) Alignment in total knee arthroplasty, still more questions than answers. Knee Surg Sports Traumatol Arthrosc 21:2191–2193
Thienpont E, Parvizi J (2016) A new classification for the varus knee. J Arthroplasty 31:2156–2160
Walker PS, Garg A (1991) Range of motion in total knee arthroplasty. A computer analysis. Clin Orthop Relat Res 227–235
Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG (1994) Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res 31–43
Yoon J-R, Han S-B, Jee M-K, Shin Y-S (2017) Comparison of kinematic and mechanical alignment techniques in primary total knee arthroplasty. Medicine (Baltimore) 96
Funding
This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FK receives royalties of Königsee and honoraria of ConforMIS, all outside the submitted work. DJ has received compensations covering the living costs in Boston from ConforMIS. JB receives honoraria from DePuy, Smith&Nephew and ConforMIS, all outside the submitted work. ET is a speaker bureau for ComaTec, KCI, Limo, Medacta, and Zimmer Biomet, receives royalties of Zimmer Biomet and is EKS President 2019, all outside the submitted work. RB has no potential conflict of interest. MM has no potential conflict of interest.
Ethical approval
Since the present study is based on analysing anonymised CT data, IRB approval was not required. Any information that could identify patients was not use in the analysis. Investigators dealt with anonymised data only. All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Meier, M., Janssen, D., Koeck, F.X. et al. Variations in medial and lateral slope and medial proximal tibial angle. Knee Surg Sports Traumatol Arthrosc 29, 939–946 (2021). https://doi.org/10.1007/s00167-020-06052-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06052-y