Abstract
Background
Epilepsy might be one of the manifestations in children with leukodystrophies, but the incidence of epilepsy in different types of leukodystrophies is unclear yet.
Methods
A retrospective observational cohort study was performed on children diagnosed with leukodystrophies in Peking University First Hospital from January 2004 to June 2019, and the patients were followed for 5.5 years (0.4–14.2 years) after the first visit.
Results
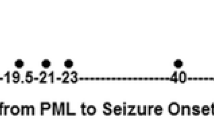
A total of 333 patients were included. The overall incidence of epilepsy was 30.6% (102/333). Alexander disease had the highest incidence (77.3%, 51/66), followed by vanishing white matter disease (41.2%, 21/51), Canavan disease (33.3%, 1/3), megalencephalic leukoencephalopathy with subcortical cysts (32.1%, 9/28), X-linked adrenoleukodystrophy (23.1%, 3/13), Krabbe disease (18.8%, 3/16), metachromatic leukodystrophy (14.3%, 6/42), and Pelizaeus–Merzbacher disease (7.0%, 8/114). The incidence of epilepsy in leukodystrophies classified as astrocytopathies was higher than that in myelin disorders (55.9% vs. 11.2%, P < 0.001). Of the 102 patients with epilepsy, seizures were the chief complaint in 61.8% (63/102) and the initial symptom in 22.5% (23/102). The median age at seizure onset was 20.5 months (1 day–176 months). A total of 63.7% (65/102) of children were treated with antiepileptic drugs (AEDs), and the responder rate was 90.8% (59/65) at the last follow-up, including 71.2% (42/59) of children who were seizure free.
Conclusions
Epilepsy was not uncommon in children with leukodystrophies. Children with Alexander disease had the highest incidence; whereas, children with Pelizaeus–Merzbacher disease had the lowest incidence. Children with leukodystrophies classified as astrocytopathies were more prone to have epilepsy than those classified as myelin disorders. Most children with leukodystrophies who presented with epilepsy showed a good response to antiepileptic drugs.


Similar content being viewed by others
References
Parikh S, Bernard G, Leventer RJ et al (2015) A clinical approach to the diagnosis of patients with leukodystrophies and genetic leukoencephelopathies. Mol Genet Metab 114:501–515
van der Knaap MS, Bugiani M (2017) Leukodystrophies: a proposed classification system based on pathological changes and pathogenetic mechanisms. Acta Neuropathol 134:351–382
Bonkowsky JL, Nelson C, Kingston JL, Filloux FM, Mundorff MB, Srivastava R (2010) The burden of inherited leukodystrophies in children. Neurology 75:718–725
Balslev T, Cortez MA, Blaser SI, Haslam RH (1997) Recurrent seizures in metachromatic leukodystrophy. Pediatr Neurol 17:150–154
Karimzadeh P, Jafari N, Nejad Biglari H et al (2014) The Clinical features and diagnosis of Canavan's disease: a case series of Iranian patients. Iran J Child Neurol 8:66–71
Sakurai K, Ohashi T, Shimozawa N, Joo-Hyun S, Okuyama T, Ida H (2019) Characteristics of Japanese patients with X-linked adrenoleukodystrophy and concerns of their families from the 1st registry system. Brain Dev 41:50–56
Velasco Parra HM, Maradei Anaya SJ, Acosta Guio JC, Arteaga Diaz CE, Prieto Rivera JC (2018) Clinical and mutational spectrum of Colombian patients with Pelizaeus Merzbacher Disease. Colomb Med 49:182–187
Golomb MR, Walsh LE, Carvalho KS, Christensen CK, DeMyer WE (2004) Clinical findings in Pelizaeus–Merzbacher disease. J Child Neurol 19:328–331
Boison D, Steinhauser C (2018) Epilepsy and astrocyte energy metabolism. Glia 66:1235–1243
Zafeiriou DI, Kontopoulos EE, Michelakakis HM, Anastasiou AL, Gombakis NP (1999) Neurophysiology and MRI in late-infantile metachromatic leukodystrophy. Pediatr Neurol 21:843–846
Fukumizu M, Matsui K, Hanaoka S, Sakuragawa N, Kurokawa T (1992) Partial seizures in two cases of metachromatic leukodystrophy: electrophysiologic and neuroradiologic findings. J Child Neurol 7:381–386
Lee JM, Kim AS, Lee SJ et al (2006) A case of infantile Alexander disease accompanied by infantile spasms diagnosed by DNA analysis. J Korean Med Sci 21:954–957
Vembu P, Khaffaji S, Yadav G, Khan RA (2009) Juvenile metachromatic leukodystrophy in a boy with epilepsy. Neurosciences 14:290–291
Hagberg B (1984) Krabbe's disease: clinical presentation of neurological variants. Neuropediatrics 15(Suppl):11–15
Morse LE, Rosman NP (2006) Myoclonic seizures in Krabbe disease: a unique presentation in late-onset type. Pediatr Neurol 35:154–157
Bonthius DJ, Karacay B (2016) Alexander disease: a novel mutation in GFAP leading to epilepsia partialis continua. J Child Neurol 31:869–872
Arvidsson J, Hagberg B, Mansson JE, Svennerholm L (1995) Late onset globoid cell leukodystrophy (Krabbe's disease)—Swedish case with 15 years of follow-up. Acta Paediatr 84:218–221
Wang PJ, Hwu WL, Shen YZ (2001) Epileptic seizures and electroencephalographic evolution in genetic leukodystrophies. J Clin Neurophysiol 18:25–32
Kurlemann G, Palm DG (1991) Vigabatrin in metachromatic leucodystrophy; positive influence on spasticity. Dev Med Child Neurol 33:182
Acknowledgements
This study was supported by the National Science and Technology Major Project of the Ministry of Science and Technology of China (Grant no. 2017ZX09304029-006), National Natural Science Foundation of China (Grant no. 81741053), National Key Research and Development Program of China (Grant nos. 2016YFC0901505 and 2016YFC1306201), Beijing Key Laboratory of Molecular Diagnosis and Study on Pediatric Genetic Diseases (Grant no. BZ0317) and Research Seed Fund of Peking University First Hospital (Grant no. 2019SF14).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no financial or other conflicts of interest.
Ethical standards
The study was approved by the clinical research ethics committee of the Peking University First Hospital. Written informed consents were obtained from the parents.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, J., Ban, T., Zhou, L. et al. Epilepsy in children with leukodystrophies. J Neurol 267, 2612–2618 (2020). https://doi.org/10.1007/s00415-020-09889-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09889-y