Abstract
Purpose
Current virtual reality-based (VR) simulators for robot-assisted minimally invasive surgery (RAMIS) training lack effective teaching and coaching. Our objective was to develop an automated teaching framework for VR training in RAMIS. Second, we wanted to study the effect of such real-time teaching cues on surgical technical skill acquisition. Third, we wanted to assess skill in terms of surgical technique in addition to traditional time and motion efficiency metrics.
Methods
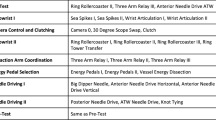
We implemented six teaching cues within a needle passing task on the da Vinci Skills Simulator platform (noncommercial research version). These teaching cues are graphical overlays designed to demonstrate ideal surgical technique, e.g., what path to follow while passing needle through tissue. We created three coaching modes: teach (continuous demonstration), metrics (demonstration triggered by performance metrics), and user (demonstration upon user request). We conducted a randomized controlled trial where the experimental group practiced using automated teaching and the control group practiced in a self-learning manner without automated teaching.
Results
We analyzed data from 30 participants (14 in experimental and 16 in control group). After three practice repetitions, control group showed higher improvement in time and motion efficiency, while experimental group showed higher improvement in surgical technique compared to their baseline measurements. The experimental group showed more improvement than the control group on a surgical technique metric (at what angle is needle grasped by an instrument), and the difference between groups was statistically significant.
Conclusion
In a pilot randomized controlled trial, we observed that automated teaching cues can improve the performance of surgical technique in a VR simulator for RAMIS needle passing. Our study was limited by its recruitment of nonsurgeons and evaluation of a single configuration of coaching modes.



Similar content being viewed by others
Notes
Henceforth, in this paper, surgical skill will refer to technical skill specifically.
https://www.facs.org/education/program/resident-skills; Scott et al. [22].
Illustrations are provided as Electronic Supplementary Material 2, 3, and 4.
References
Becker AJ (2009) It’s not what they do, it’s how they do it: athlete experiences of great coaching. Int J Sports Sci Coach 4(1):93–119. https://doi.org/10.1260/1747-9541.4.1.93
Birkmeyer JD, Finks JF, O’Reilly A, Oerline M, Carlin AM, Nunn AR, Dimick J, Banerjee M, Birkmeyer NJ (2013) Surgical skill and complication rates after bariatric surgery. New Engl J Med 369(15):1434–1442. https://doi.org/10.1056/NEJMsa1300625
Boyle E, Al-Akash M, Gallagher AG, Traynor O, Hill ADK, Neary PC (2011) Optimising surgical training: use of feedback to reduce errors during a simulated surgical procedure. Postgrad Med J. https://doi.org/10.1136/pgmj.2010.109363
Chen Z, Malpani A, Chalasani P, Deguet A, Vedula SS, Kazhanzides P, Taylor RH (2016) Virtual fixture assistance for needle passing and knot tying. In: 2016 IEEE/RSJ international conference on intelligent robots and systems (IROS), pp 2343–2350. https://doi.org/10.1109/IROS.2016.7759365
Cohen J (1977) CHAPTER 2—the t test for means. In: Statistical power analysis for the behavioral sciences, Revised edition. Academic Press, London, pp 19–74. https://doi.org/10.1016/B978-0-12-179060-8.50007-4
Cole SJ, Mackenzie H, Ha J, Hanna GB, Miskovic D (2013) Randomized controlled trial on the effect of coaching in simulated laparoscopic training. Surg Endosc 28(3):979–986. https://doi.org/10.1007/s00464-013-3265-0
Crochet P, Aggarwal R, Dubb SS, Ziprin P, Rajaretnam N, Grantcharov T, Ericsson KA, Darzi A (2011) Deliberate practice on a virtual reality laparoscopic simulator enhances the quality of surgical technical skills. Ann Surg 253(6):1216–1222
Dosis A, Aggarwal A, Bello F, Moorthy K, Munz Y, Gillies D, Darzi A (2005) Synchronized video and motion analysis for the assessment of procedures in the operating theater. Arch Surg 140(3):293–299. https://doi.org/10.1001/archsurg.140.3.293
Fecso AB, Szasz P, Kerezov G, Grantcharov TP (2017) The effect of technical performance on patient outcomes in surgery: a systematic review. Ann Surg 265(3):492–501. https://doi.org/10.1097/SLA.0000000000001959
Gardner AK, Abdelfattah K, Wiersch J, Ahmed RA, Willis RE (2015) Embracing errors in simulation-based training: the effect of error training on retention and transfer of central venous catheter skills. J Surg Educ 72(6):e158–e162. https://doi.org/10.1016/j.jsurg.2015.08.002
Gardner AK, Nepomnayshy D, Reickert C, Gee DW, Brydges R, Korndorffer JR, Scott DJ, Sachdeva AK (2016) The value proposition of simulation. Surgery 160(3):546–551. https://doi.org/10.1016/j.surg.2016.03.028
Greenberg CC, Ghousseini HN, Pavuluri Quamme SR, Beasley HL, Wiegmann DA (2015) Surgical coaching for individual performance improvement. Ann Surg 261(1):32–34. https://doi.org/10.1097/SLA.0000000000000776
Gross ND, Holsinger FC, Magnuson JS, Duvvuri U, Genden EM, Ghanem TA, Yaremchuk KL, Goldenberg D, Miller MC, Moore EJ, Morris LG, Netterville J, Weinstein GS, Richmon J (2016) Robotics in otolaryngology and head and neck surgery: recommendations for training and credentialing: a report of the 2015 AHNS education committee, AAO-HNS robotic task force and AAO-HNS sleep disorders committee. Head Neck 38(S1):E151–E158. https://doi.org/10.1002/hed.24207
Jog A, Itkowitz B, Liu M, DiMaio S, Hager G, Curet M, Kumar R (2011) Towards integrating task information in skills assessment for dexterous tasks in surgery and simulation. In: 2011 IEEE international conference on robotics and automation (ICRA), pp 5273–5278. https://doi.org/10.1109/ICRA.2011.5979967
Lenihan JP (2011) Navigating credentialing, privileging, and learning curves in robotics with an evidence and experienced-based approach. Clin Obstet Gynecol 54(3):382–390. https://doi.org/10.1097/GRF.0b013e31822b47e2
Malpani A (2017) Automated virtual coach for surgical training. Ph.D., Johns Hopkins University, Baltimore, MD
Mazzon G, Sridhar A, Busuttil G, Thompson J, Nathan S, Briggs T, Kelly J, Shaw G (2017) Learning curves for robotic surgery: a review of the recent literature. Curr Urol Rep., p 89. https://doi.org/10.1007/s11934-017-0738-z
Moglia A, Ferrari V, Morelli L, Ferrari M, Mosca F, Cuschieri A (2016) A systematic review of virtual reality simulators for robot-assisted surgery. Eur Urol 69(6):1065–1080. https://doi.org/10.1016/j.eururo.2015.09.021
Pradarelli JC, Campbell DA, Dimick JB (2015) Hospital credentialing and privileging of surgeons: a potential safety blind spot. JAMA 313(13):1313–1314. https://doi.org/10.1001/jama.2015.1943
Pradarelli JC, Thornton JP, Dimick JB (2017) Who is responsible for the safe introduction of new surgical technology? An important legal precedent from the da Vinci surgical system trials. JAMA Surg 152(8):717–718. https://doi.org/10.1001/jamasurg.2017.0841
Satava RM (2019) The future of surgical simulation. In: Stefanidis D, Korndorffer Jr JR, Sweet R (eds) Comprehensive healthcare simulation: surgery and surgical subspecialties, comprehensive healthcare simulation. Springer, Cham, pp 379–387. https://doi.org/10.1007/978-3-319-98276-2_31
Scott DJ, Dunnington GL (2008) The new ACS/APDS skills curriculum: moving the learning curve out of the operating room. J Gastrointest Surg 12(2):213–221. https://doi.org/10.1007/s11605-007-0357-y
Singh P, Aggarwal R, Tahir M, Pucher PH, Darzi A (2015) A randomized controlled study to evaluate the role of video-based coaching in training laparoscopic skills. Ann Surg 261(5):862–869. https://doi.org/10.1097/SLA.0000000000000857
Stefanidis D, Anderson-Montoya B, Higgins RV, Pimentel ME, Rowland P, Scarborough MO, Higgins D (2016) Developing a coaching mechanism for practicing surgeons. Surgery 160(3):536–545. https://doi.org/10.1016/j.surg.2016.03.036
Stefanidis D, Korndorffer JR, Sweet R (eds) (2019) Comprehensive healthcare simulation: surgery and surgical subspecialties. Comprehensive healthcare simulation. Springer, Cham. https://doi.org/10.1007/978-3-319-98276-2
Tam V, Borrebach J, Dunn SA, Bellon J, Zeh HJ, Hogg ME (2019) Proficiency-based training and credentialing can improve patient outcomes and decrease cost to a hospital system. Am J Surg 217(4):591–596. https://doi.org/10.1016/j.amjsurg.2018.07.053
van Dongen KW, van der Wal WA, Rinkes IHMB, Schijven MP, Broeders IAMJ (2008) Virtual reality training for endoscopic surgery: voluntary or obligatory? Surg Endosc 22(3):664–667. https://doi.org/10.1007/s00464-007-9456-9
Woelk JL, Casiano ER, Weaver AL, Gostout BS, Trabuco EC, Gebhart JB (2013) The learning curve of robotic hysterectomy. Obstet Gynecol 121(1):87–95. https://doi.org/10.1097/AOG.0b013e31827a029e
Zapf MAC, Ujiki MB (2015) Surgical resident evaluations of portable laparoscopic box trainers incorporated into a simulation-based minimally invasive surgery curriculum. Surg Innov 22(1):83–87. https://doi.org/10.1177/1553350614535858
Acknowledgements
We thank Anusha Balan, Sina Parastegari, Prasad, and Ashwin from Intuitive Surgical Inc. (ISI, Sunnyvale, California) for their help with the dVSim. We thank Simon DiMaio (ISI) for his feedback and helpful inputs. We thank Anthony Jarc (ISI) for help with the study IRB logistics. We thank Umut and Daniel from SenseGraphics AB (Kista, Sweden) for their support related to the H3DAPI.
Funding
Anand Malpani was supported through a Link Foundation fellowship award for advanced simulation and training.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Anand Malpani was employed as an intern at Intuitive Surgical Inc. (Sunnyvale, California, USA) during part of this work. Henry C. Lin is an employee at Intuitive Surgical Inc. (Sunnyvale, California, USA). Intuitive Surgical Inc. manufactures the da Vinci Skills Simulator that was used as the platform to test the work on. Gregory D. Hager and Russell H. Taylor have received funding from Intuitive Surgical Inc. previously for other research projects. Johns Hopkins University and Intuitive Surgical Inc. have an ongoing partnership to support research on the surgical robots.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Western IRB, Protocol 20121049) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Thanks to the Link Foundation Fellowship for Advanced Simulation and Training awarded to Anand Malpani. This work is part of Anand Malpani’s Ph.D. Thesis [16].
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (mp4 13276 KB)
Rights and permissions
About this article
Cite this article
Malpani, A., Vedula, S.S., Lin, H.C. et al. Effect of real-time virtual reality-based teaching cues on learning needle passing for robot-assisted minimally invasive surgery: a randomized controlled trial. Int J CARS 15, 1187–1194 (2020). https://doi.org/10.1007/s11548-020-02156-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-020-02156-5