Abstract
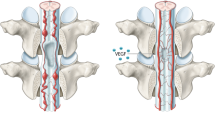
The therapeutic effect of deferoxamine (DFO) for spinal cord injury (SCI) has been demonstrated in previous studies; however, the exact mechanism of action is still unclear. Here, we hypothesized that DFO ameliorates spinal cord compression by promoting neovascularization. Using an SCI model of moderate compression, rats were intraperitoneally injected with 30 mg/kg or 100 mg/kg DFO for 1–2 weeks, and significant neovascularization was found in the injured spinal cord, showing overexpression of hypoxia inducible factor-1α (HIF-1α) and vascular endothelial growth factor (VEGF), and an increase in the number of new blood vessels. In addition, SCI in rats was significantly ameliorated after treatment with DFO, with less motor dysfunction, increased spared neural tissue, and improved electrophysiological conduction. By contrast, the ameliorative effect of DFO on SCI was suppressed when DFO-induced neovascularization was blocked by lenvatinib, a vascular endothelial growth factor receptor inhibitor, further suggesting that the primary pharmacological effect of DFO in SCI is the promotion of neovascularization. Therefore, we concluded that DFO effectively alleviated SCI by promoting neovascularization in the injured spinal cord. Considering that DFO is an FDA-approved free radical scavenger and iron chelator, it may represent a promising alternative strategy for SCI therapy in the future.





Similar content being viewed by others
Availability of Data and Material
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Basso DM, Beattie MS, Bresnahan JC (1995) A sensitive and reliable locomotor rating scale for open field testing in rats. J Neurotrauma 12:1–21. https://doi.org/10.1089/neu.1995.12.1
Borgens RB, Bohnert D (2001) Rapid recovery from spinal cord injury after subcutaneously administered polyethylene glycol. J Neurosci Res 66:1179–1186. https://doi.org/10.1002/jnr.1254
Borgens RB, Shi R (2000) Immediate recovery from spinal cord injury through molecular repair of nerve membranes with polyethylene glycol. FASEB J : Off Publ Fed Am Soc Exp Biol 14:27–35
Brambilla R, Hurtado A, Persaud T, Esham K, Pearse D, Oudega M, Bethea J (2009) Transgenic inhibition of astroglial NF-kappa B leads to increased axonal sparing and sprouting following spinal cord injury. J Neurochem 110:765–778
Casella GT, Marcillo A, Bunge MB, Wood PM (2002) New vascular tissue rapidly replaces neural parenchyma and vessels destroyed by a contusion injury to the rat spinal cord. Exp Neurol 173:63–76. https://doi.org/10.1006/exnr.2001.7827
Chen Z et al (2016) Mitigation of sensory and motor deficits by acrolein scavenger phenelzine in a rat model of spinal cord contusive injury. J Neurochem 138:328–338. https://doi.org/10.1111/jnc.13639
Dinc C, Iplikcioglu AC, Atabey C, Eroglu A, Topuz K, Ipcioglu O, Demirel D (2013) Comparison of deferoxamine and methylprednisolone: protective effect of pharmacological agents on lipid peroxidation in spinal cord injury in rats. Spine 38:E1649–E1655. https://doi.org/10.1097/BRS.0000000000000055
Dukes EM, Kirshblum S, Aimetti AA, Qin SS, Bornheimer RK, Oster G (2017) Relationship of American Spinal Injury Association Impairment Scale grade to post-injury hospitalization and costs in thoracic spinal cord. Inj Neurosurg. https://doi.org/10.1093/neuros/nyx425
Graumann U, Ritz MF, Hausmann O (2011) Necessity for re-vascularization after spinal cord injury and the search for potential therapeutic options. Curr Neurovascular Res 8:334–341
Herrera JJ, Sundberg LM, Zentilin L, Giacca M, Narayana PA (2010) Sustained expression of vascular endothelial growth factor and angiopoietin-1 improves blood-spinal cord barrier integrity and functional recovery after spinal cord injury. J Neurotrauma 27:2067–2076. https://doi.org/10.1089/neu.2010.1403
Holtz A, Nystrom B, Gerdin B (1990) Effect of methylprednisolone on motor function and spinal cord blood flow after spinal cord compression in rats. Acta Neurol Scandinavica 82:68–73
Ito Y, Sugimoto Y, Tomioka M, Kai N, Tanaka M (2009) Does high dose methylprednisolone sodium succinate really improve neurological status in patient with acute cervical cord injury?: a prospective study about neurological recovery and early complications. Spine 34:2121–2124. https://doi.org/10.1097/BRS.0b013e3181b613c7
Lee BB, Cripps RA, Fitzharris M, Wing PC (2014) The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord 52:110–116. https://doi.org/10.1038/sc.2012.158
Liu J, Tang T, Yang H (2011) Protective effect of deferoxamine on experimental spinal cord injury in rat. Injury 42:742–745. https://doi.org/10.1016/j.injury.2010.08.028
Luo J, Borgens R, Shi R (2002) Polyethylene glycol immediately repairs neuronal membranes and inhibits free radical production after acute spinal cord injury. J Neurochem 83:471–480
Luo J, Uchida K, Shi R (2005) Accumulation of acrolein-protein adducts after traumatic spinal cord injury. Neurochem Res 30:291–295
Masoud G, Li W (2015) HIF-1α pathway: role, regulation and intervention for cancer therapy. Acta Pharm Sin B 5:378–389
Nowicki M, Kosacka J, Spanel-Borowski K, Borlak J (2009) Deferoxamine-induced neurite outgrowth and synapse formation in postnatal rat dorsal root ganglion (DRG) cell cultures. Eur J Cell Biol 88:551–562. https://doi.org/10.1016/j.ejcb.2009.05.003
Paterniti I, Mazzon E, Emanuela E, Paola RD, Galuppo M, Bramanti P, Cuzzocrea S (2010) Modulation of inflammatory response after spinal cord trauma with deferoxamine, an iron chelator. Free Rad Res 44:694–709. https://doi.org/10.3109/10715761003742993
Santiago J, Rosas O, Torrado A, González M, Kalyan-Masih P, Miranda J (2009) Molecular, anatomical, physiological, and behavioral studies of rats treated with buprenorphine after spinal cord injury. J Neurotrauma 26:1783–1793
Thangarajah H et al (2009) The molecular basis for impaired hypoxia-induced VEGF expression in diabetic tissues. Proc Natl Acad Sci USA 106:13505–13510
Vissapragada R et al (2014) Bidirectional crosstalk between periventricular endothelial cells and neural progenitor cells promotes the formation of a neurovascular unit. Brain Res 1565:8–17
Walters BC et al (2013) Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurg 60(Suppl 1):82–91. https://doi.org/10.1227/01.neu.0000430319.32247.7f
Wang C, Cai Y, Zhang Y, Xiong Z, Li G, Cui L (2014) Local injection of deferoxamine improves neovascularization in ischemic diabetic random flap by increasing HIF-1alpha and VEGF expression. PloS One 9:e100818. https://doi.org/10.1371/journal.pone.0100818
Wang L, Shi Q, Dai J, Gu Y, Feng Y, Chen L (2018) Increased vascularization promotes functional recovery in the transected spinal cord rats by implanted vascular endothelial growth factor-targeting collagen scaffold. J Orthopaedic Res : Off Publ Orthopaedic Res Soc 36:1024–1034. https://doi.org/10.1002/jor.23678
Wei X et al (2018) Efficacy of lenvatinib, a multitargeted tyrosine kinase inhibitor, on laser-induced CNV mouse model of neovascular AMD. Exp Eye Res 168:2–11. https://doi.org/10.1016/j.exer.2017.12.009
Weng R, Li Q, Li H, Yang M, Sheng L (2010) Mimic hypoxia improves angiogenesis in ischaemic random flaps. J Plast Reconstr Aesthet Surg 63:2152–2159
Widenfalk J, Lipson A, Jubran M, Hofstetter C, Ebendal T, Cao Y, Olson L (2003) Vascular endothelial growth factor improves functional outcome and decreases secondary degeneration in experimental spinal cord contusion injury. Neuroscience 120:951–960
Yu S, Yao S, Wen Y, Wang Y, Wang H, Xu Q (2016) Angiogenic microspheres promote neural regeneration and motor function recovery after spinal cord injury in rats Scientific Rep 6:33428. https://doi.org/10.1038/srep33428
Acknowledgments
This work was supported by the Natural Science Foundation of Jiangsu Province (No. BK20161274), the Natural Science Foundation of Suzhou (No. kjxw2015056) and the Science and Technology Bureau of Kunshan (No. KS1547). We would also like to thank LetPub for providing linguistic assistance during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
All experimental procedures were performed in accordance with protocols approved by the Animal Ethics Committee of Soochow University, Suzhou, China.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PNG 3082 kb)
Rights and permissions
About this article
Cite this article
Tang, G., Chen, Y., Chen, J. et al. Deferoxamine Ameliorates Compressed Spinal Cord Injury by Promoting Neovascularization in Rats. J Mol Neurosci 70, 1437–1444 (2020). https://doi.org/10.1007/s12031-020-01564-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-020-01564-1