Abstract
Purpose of Review
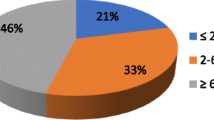
One of the consequences of the opioid epidemic is an increase in the number of opioid-tolerant patients. These patients are at higher risk for readmission and longer hospital stays following surgery. Enhanced recovery after surgery (ERAS) pathways can be used as a framework for providing high-quality comprehensive care to patient population. It is estimated that as many as 15% of all surgery patients in the USA are receiving opioids going into surgery. The number of patients on medication maintenance therapy with long-acting opioids such as methadone or partial mu receptor agonists like buprenorphine is rising, which poses a challenge for perioperative healthcare providers.
Recent Findings
Preoperative opioid tolerance is an independent predictor for increased length of hospital stays, high costs, and increased readmission rates following surgery. Given the recent trends, it is likely that more opioid-tolerant patients will require surgery in near future. Enhanced recovery programs can be used to provide a framework for high-quality care to opioid-tolerant patients throughout all phases of the perioperative process. To improve the quality of care of opioid-tolerant patients, we present five general recommendations for clinicians to consider and possibly incorporate into ERAS programs and care protocols.
Summary
Recommendations include the following: opioid-tolerant patients should not be excluded from ERAS programs; opioid-tolerant patients should be identified preoperatively; programs should establish standard practices for patients on medication maintenance therapy and buprenorphine; opioid-tolerant patients should receive multimodal analgesia perioperatively; and opioid-tolerant patients should receive coordinated follow up after surgery.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths--United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;64:1378–82.
Manchikanti L, Fellows B, Ailinani H, Pampati V. Therapeutic use, abuse, and nonmedical use of opioids: a ten-year perspective. Pain Physician. 2010;13:401–35.
• Ahrnsbrak R, Bose J, Hedden S, Lipari R, Park-Lee E. Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health [Internet]. Substance Abuse and Mental Health Services Administration (SAMHSA); 2017. Available from: https://www.samhsa.gov/data/. Accessed 15 April 2020. Important national survey of drug use and health.
Waljee JF, Cron DC, Steiger RM, Zhong L, Englesbe MJ, Brummett CM. Effect of preoperative opioid exposure on healthcare utilization and expenditures following elective abdominal surgery. Ann Surg. 2017;265:715–21.
•• Jonan AB, Kaye AD, Urman RD. Buprenorphine formulations: Clinical best practice strategies recommendations for perioperative management of patients undergoing surgical or interventional pain procedures. Pain Physician. 2018;21:E1–12. Best practice strategies for patients undergoing surgery or interventional procedures on buprenorphine.
Gulur P, Williams L, Chaudhary S, Koury K, Jaff M. Opioid tolerance--a predictor of increased length of stay and higher readmission rates. Pain Physician. 2014;17:E503–7.
Cron DC, Englesbe MJ, Bolton CJ, Joseph MT, Carrier KL, Moser SE, et al. Preoperative opioid use is independently associated with increased costs and worse outcomes after major abdominal surgery. Ann Surg. 2017;265:695–701.
Urman RD, Seger DL, Fiskio JM, Neville BA, Harry EM, Weiner SG, et al. The burden of opioid-related adverse drug events on hospitalized previously opioid-free surgical patients. J Patient Saf. 2019. https://doi.org/10.1097/PTS.0000000000000566.
Stone AB, Jones MR, Rao N, Urman RD. A dashboard for monitoring opioid-related adverse drug events following surgery using a National Administrative Database. Am J Med Qual. 2019;34:45–52. https://doi.org/10.1177/1062860618782646.
Kaye AD, Helander EM, Vadivelu N, Lumermann L, Suchy T, Rose M, et al. Consensus statement for clinical pathway development for perioperative pain management and care transitions. Pain Ther. 2017;6:129–41. https://doi.org/10.1007/s40122-017-0079-0.
Kaye AD, Jones MR, Kaye AM, Ripoll JG, Jones DE, Galan V, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse (Part 2). Pain Physician. 2017;20:S111–S133.
Kaye AD, Jones MR, Kaye AM, Ripoll JG, Galan V, Beakley BD, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: Part 1. Pain Physician. 2017;20:S93–S109. (Review).
Katz J, Weinrib A, Fashler SR, Katznelzon R, Shah BR, Ladak SS, et al. The Toronto general hospital transitional pain service: development and implementation of a multidisciplinary program to prevent chronic postsurgical pain. J Pain Res. 2015;8:695–702.
Aronson S, Westover J, Guinn N, Setji T, Wischmeyer P, Gulur P, et al. A perioperative medicine model for population health: an integrated approach for an evolving clinical science. Anesth Analg. 2018;126:682–90.
Helander EM, Webb MP, Bias M, Whang EE, Kaye AD, Urman RD. Use of regional anesthesia techniques: analysis of institutional enhanced recovery after surgery protocols for colorectal surgery. J Laparoendosc Adv Surg Tech A. 2017;27:898–902. https://doi.org/10.1089/lap.2017.0339.
Helander EM, Webb MP, Bias M, Whang EE, Kaye AD, Urman RD. A comparison of multimodal analgesic approaches in institutional enhanced recovery after surgery protocols for colorectal surgery: pharmacological agents. J Laparoendosc Adv Surg Tech A. 2017;27:903–8. https://doi.org/10.1089/lap.2017.0338.
•• Soffin EM, Lee BH, Kumar KK, Wu CL. The prescription opioid crisis: role of the anaesthesiologist in reducing opioid use and misuse. Br J Anaesth. 2019;122:e198–e208. https://doi.org/10.1016/j.bja.2018.11.019. Interesting article on the role of the anesthesiologist in reducing opioid use and misuse.
Pirrera B, Lucchi A, Gabbianelli C, Alagna V, Martorelli G, Berti P, et al. E.R.A.S. pathway in colorectal surgery in elderly: Our experience: A retrospective cohort study. Int J Surg Lond Engl. 2017;43:101–6.
Day RW, Fielder S, Calhoun J, Kehlet H, Gottumukkala V, Aloia TA. Incomplete reporting of enhanced recovery elements and its impact on achieving quality improvement. Br J Surg. 2015;102:1594–602.
Labgaa I, Jarrar G, Joliat GR, Allemann P, Gander S, Blanc C, et al. Implementation of enhanced recovery (ERAS) in colorectal surgery has a positive impact on Non-ERAS liver surgery patients. World J Surg. 2016;40:1082–91. https://doi.org/10.1007/s00268-015-3363-3.
Simpson G, Jackson M. Perioperative management of opioid-tolerant patients. BJA Educ. 2017;17:124–8.
Anderson TA, Quaye ANA, Ward EN, Wilens TE, Hilliard PE, Brummett CM. To stop or not, that is the question: acute pain management for the patient on chronic buprenorphine. Anesthesiology. 2017;126:1180–6.
Ward EN, Quaye AN-A, Wilens TE. Opioid use disorders: perioperative management of a special population. Anesth Analg. 2018;127:539–47.
Goel A, Azargive S, Weissman JS, Shanthanna H, Hanlon JG, Samman B, et al. Perioperative pain and addiction interdisciplinary network (PAIN) clinical practice advisory for perioperative management of buprenorphine: results of a modified Delphi process. Br J Anaesth [Internet]. 2019 [cited 2019 Jun 27]; Available from: https://linkinghub.elsevier.com/retrieve/pii/S0007091219303253. Accessed 15 April 2020.
Wick EC, Galante DJ, Hobson DB, Benson AR, Lee KK, Berenholtz SM, et al. Organizational culture changes result in improvement in patient-centered outcomes: implementation of an integrated recovery pathway for surgical patients. J Am Coll Surg. 2015;221:669–77.
McEvoy MD, Scott MJ, Gordon DB, Grant SA, Thacker JKM, Wu CL, et al. American Society for Enhanced Recovery (ASER) and perioperative quality initiative (POQI) joint consensus statement on optimal analgesia within an enhanced recovery pathway for colorectal surgery: part 1-from the preoperative period to PACU. Perioper Med Lond Engl. 2017;6:8.
Malik OS, Kaye AD, Urman RD. Perioperative Hyperalgesia and associated clinical factors. Curr Pain Headache Rep. 2017;21:4.
Doverty M, Somogyi AA, White JM, Bochner F, Beare CH, Menelaou A, et al. Methadone maintenance patients are cross-tolerant to the antinociceptive effects of morphine. Pain. 2001;93:155–63.
Grant MC, Pio Roda CM, Canner JK, Sommer P, Galante D, Hobson D, et al. The impact of anesthesia-influenced process measure compliance on length of stay: results from an enhanced recovery after surgery for colorectal surgeryCohort. Anesth Analg. 2019;128:68–74. https://doi.org/10.1213/ANE.0000000000003458.
Levy N, Lobo DN, Fawcett WJ, Ljungqvist O, Scott MJ. Opioid stewardship: a need for opioid discharge guidance. Comment on Br J Anaesth 2019; 122. Br J Anaesth. 2019;
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
RU has received research funding from Medtronic, Mallinckrodt, Merck, and honorarium from 3 M. WJF reports honoraria from Merck, Baxter, Grunethal, and Smiths for lecturing and travel expenses. Alexander Stone, Antonia Roberts, Hans D. de Boer, William J. Fawcett, and Richard D. Urman declare no conflict of interest. Alan Kaye is a Section Editor for Current Pain and Headache Reports. He has not been involved in the review process for the manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Other Pain
Rights and permissions
About this article
Cite this article
Stone, A., Roberts, A., de Boer, H.D. et al. Recommendations for Managing Opioid-Tolerant Surgical Patients within Enhanced Recovery Pathways. Curr Pain Headache Rep 24, 28 (2020). https://doi.org/10.1007/s11916-020-00856-w
Published:
DOI: https://doi.org/10.1007/s11916-020-00856-w