Abstract
Background
Increasing numbers of reproductive-aged women are using attention-deficit/hyperactivity disorder (ADHD) medications. Findings from studies exploring the safety of these medications during pregnancy are mixed, and it is unclear whether associations reflect causal effects or could be partially or fully explained by other factors that differ between exposed and unexposed offspring.
Objectives
The aim of this systematic review was to evaluate the adverse pregnancy-related and offspring outcomes associated with exposure to prescribed ADHD medication during pregnancy with a focus on how studies to date have handled the influence of confounding.
Methods
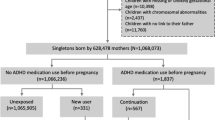
We searched PubMed, Embase, PsycINFO, and Web of Science up to 1 July 2019 without any restrictions on language or date of publication. We included all observational studies (e.g., cohort studies, case–control studies, case–crossover studies, cross-sectional studies, and registry-based studies) with pregnant women of any age or from any setting who were prescribed ADHD medications and evaluated any outcome, including both short- and long-term maternal and offspring outcomes. Two independent authors then used the Newcastle–Ottawa Scale to rate the quality of the included studies.
Results
Eight cohort studies that estimated adverse pregnancy-related and offspring outcomes associated with exposure to ADHD medication during pregnancy were included in the qualitative review. The included studies had substantial methodological differences in data sources, type of medications examined, definitions of studied pregnancy-related and offspring outcomes, types of control groups, and confounding adjustment. There was no convincing evidence for teratogenic effects according to the relative risk of pregnancy-related and offspring outcomes, and the observed differences in absolute risks were overall small in magnitude. Adjustment for confounding was inadequate in most studies, and none of the included studies adjusted for ADHD severity in the mothers.
Conclusion
The current evidence does not suggest that the use of ADHD medication during pregnancy results in significant adverse consequences for mother or offspring. However, the data are too limited to make an unequivocal recommendation. Therefore, physicians should consider whether the advantages of using ADHD medication outweigh the potential risks for the developing fetus according to each woman’s specific circumstances. Future research should attempt to triangulate research findings based on a combination of different designs that differ in their underlying strengths and limitations and should investigate specific confounding factors, the potential impact of timing of exposure, and potential long-term outcomes in the offspring.

Similar content being viewed by others
References
Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159–65.
Caye A, et al. Life span studies of ADHD—conceptual challenges and predictors of persistence and outcome. Curr Psychiatry Rep. 2016;18(12):111.
Robison RJ, et al. Gender differences in 2 clinical trials of adults with attention-deficit/hyperactivity disorder: a retrospective data analysis. J Clin Psychiatry. 2008;69(2):213–21.
Quinn PO. Attention-deficit/hyperactivity disorder and its comorbidities in women and girls: an evolving picture. Curr Psychiatry Rep. 2008;10(5):419–23.
Cortese S, et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2018;5(9):727–38.
Cortese S, et al. Practitioner review: current best practice in the management of adverse events during treatment with ADHD medications in children and adolescents. J Child Psychol Psychiatry. 2013;54(3):227–46.
Attention deficit hyperactivity disorder: diagnosis and management. 2018; https://www.nice.org.uk/guidance/ng87. Accessed 1 Oct 2019.
Wolraich ML, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2019;144(4):e20192528. https://doi.org/10.1542/peds.2019-2528.
Faraone SV, et al. Attention-deficit/hyperactivity disorder. Nat Rev Dis Prim. 2015;1(1):15020.
Franke B, et al. Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. Eur Neuropsychopharmacol. 2018;28(10):1059–88.
Instanes JT, et al. Adult ADHD and comorbid somatic disease: a systematic literature review. J Atten Disord. 2018;22(3):203–28.
Chen Q, et al. Common psychiatric and metabolic comorbidity of adult attention-deficit/hyperactivity disorder: a population-based cross-sectional study. PLoS One. 2018;13(9):e0204516.
Adamou M, et al. Occupational issues of adults with ADHD. BMC Psychiatry. 2013;13(1):59.
Du Rietz E, et al. Predictive validity of parent- and self-rated ADHD symptoms in adolescence on adverse socioeconomic and health outcomes. Eur Child Adolesc Psychiatry. 2017;26(7):857–67.
Raman SR, et al. Trends in attention-deficit hyperactivity disorder medication use: a retrospective observational study using population-based databases. Lancet Psychiatry. 2018;5(10):824–35.
McCarthy S, et al. The epidemiology of pharmacologically treated attention deficit hyperactivity disorder (ADHD) in children, adolescents and adults in UK primary care. BMC Pediatr. 2012;12(1):78.
Castle L, et al. Trends in medication treatment for ADHD. J Atten Disord. 2007;10(4):335–42.
Zetterqvist J, et al. Stimulant and non-stimulant attention deficit/hyperactivity disorder drug use: total population study of trends and discontinuation patterns 2006–2009. Acta Psychiatr Scand. 2013;128(1):70–7.
Schulenberg J, et al. Monitoring the future national survey results on drug use, 1975–2018: volume II, college students and adults ages 19–60;2019.
dos Santos JF, et al. Maternal, fetal and neonatal consequences associated with the use of crack cocaine during the gestational period: a systematic review and meta-analysis. Arch Gynecol Obstet. 2018;298(3):487–503.
Frank DA, et al. Growth, development, and behavior in early childhood following prenatal cocaine exposure: a systematic review. JAMA. 2001;285(12):1613–25.
Chavkin W. Cocaine and pregnancy—time to look at the evidence. JAMA. 2001;285(12):1626–8.
Betancourt LM, et al. Adolescents with and without gestational cocaine exposure: longitudinal analysis of inhibitory control, memory and receptive language. Neurotoxicol Teratol. 2011;33(1):36–46.
Messinger DS, et al. The maternal lifestyle study: cognitive, motor, and behavioral outcomes of cocaine-exposed and opiate-exposed infants through three years of age. Pediatrics. 2004;113(6):1677–85.
Hurt H, et al. School performance of children with gestational cocaine exposure. Neurotoxicol Teratol. 2005;27(2):203–11.
Bada HS, et al. Preadolescent behavior problems after prenatal cocaine exposure: relationship between teacher and caretaker ratings (Maternal Lifestyle Study). Neurotoxicol Teratol. 2011;33(1):78–877.
Lester BM, LaGasse LL, Seifer R. Cocaine exposure and children: the meaning of subtle effects. Washington DC: American Association for the Advancement of Science; 1998.
Peters HT, et al. The pharmacokinetic profile of methylphenidate use in pregnancy: a study in mice. Neurotoxicol Teratol. 2016;54:1–4.
McFadyen-Leussis MP, et al. Prenatal exposure to methylphenidate hydrochloride decreases anxiety and increases exploration in mice. Pharmacol Biochem Behav. 2004;77(3):491–500.
Lloyd SA, et al. Prenatal exposure to psychostimulants increases impulsivity, compulsivity, and motivation for rewards in adult mice. Physiol Behav. 2013;119:43–51.
Teo SK, et al. The perinatal and postnatal toxicity of d-methylphenidate and d,l-methylphenidate in rats. Reprod Toxicol. 2002;16(4):353–66.
Teo SK, et al. d-Methylphenidate and d,l-methylphenidate are not developmental toxicants in rats and rabbits. Birth Defects Res B Dev Reprod Toxicol. 2003;68(2):162–71.
Beckman DA, et al. Developmental toxicity assessment of d,l-methylphenidate and d-methylphenidate in rats and rabbits. Birth Defects Res B Dev Reprod Toxicol. 2008;83(5):489–501.
Lepelletier FX, et al. Prenatal exposure to methylphenidate affects the dopamine system and the reactivity to natural reward in adulthood in rats. Int J Neuropsychopharmacol. 2014;18(4):pyu044.
Shah NS, Yates JD. Placental transfer and tissue distribution of dextro-amphetamine in the mouse. Arch Int Pharmacodyn Ther. 1978;233(2):200–8.
Nora JJ, Trasler DG, Fraser FC. Malformations in mice induced by dexamphetamine sulphate. Lancet. 1965;2(7420):1021–2.
Kasirsky G. Teratogenic effects of methamphetamine in mice and rabbits. J Am Osteopath Assoc. 1971;70(10):1119–20.
Yamamoto Y, et al. Effects of amphetamine on rat embryos developing in vitro. Reprod Toxicol. 1998;12(2):133–7.
Sauer JM, Ring BJ, Witcher JW. Clinical pharmacokinetics of atomoxetine. Clin Pharmacokinet. 2005;44(6):571–90.
Eli Lilly, Company. Strattera (atomoxetine) package insert. Indianapolis; 2002.
Jiang H, et al. Maternal and neonatal outcomes after exposure to ADHD medication during pregnancy: a systematic review and meta-analysis. Pharmacoepidemiol Drug Saf. 2019;28(3):288–95.
Von Elm E, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–7.
McAllister-Williams RH, et al. British Association for Psychopharmacology consensus guidance on the use of psychotropic medication preconception, in pregnancy and postpartum 2017. J Psychopharmacol. 2017;31(5):519–52.
Liberati A, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Med. 2009;6(7):e1000100.
Wang Z, et al. Advances in epidemiological methods and utilisation of large databases: a methodological review of observational studies on central nervous system drug use in pregnancy and central nervous system outcomes in children. Drug Saf. 2019;42(4):499–513.
The Ottawa Hospital. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2018. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 21 Aug 2019.
Bro SP, et al. Adverse pregnancy outcomes after exposure to methylphenidate or atomoxetine during pregnancy. Clin Epidemiol. 2015;7:139–47.
Cohen JM, et al. Placental complications associated with psychostimulant use in pregnancy. Obstet Gynecol. 2017;130(6):1192–201.
Diav-Citrin O, et al. Methylphenidate in pregnancy: a multicenter, prospective, comparative, observational study. J Clin Psychiatry. 2016;77(9):1176–81.
Hærvig KB, et al. Use of ADHD medication during pregnancy from 1999 to 2010: a Danish register-based study. Pharmacoepidemiol Drug Saf. 2014;23(5):526–33.
Huybrechts KF, et al. Association between methylphenidate and amphetamine use in pregnancy and risk of congenital malformations: a cohort study from the international pregnancy safety study consortium. JAMA Psychiatry. 2018;75(2):167–75.
Nörby U, Winbladh B, Källén K. Perinatal outcomes after treatment with ADHD medication during pregnancy. Pediatrics. 2017;140(6):e2017747.
Pottegard A, et al. First-trimester exposure to methylphenidate: a population-based cohort study. J Clin Psychiatry. 2014;75(1):e88–e93.
Poulton AS, Armstrong B, Nanan RK. Perinatal outcomes of women diagnosed with attention-deficit/hyperactivity disorder: an Australian Population-Based Cohort Study. CNS Drugs. 2018;32(4):377–86.
Clapp MA, et al. Unexpected term NICU admissions: a marker of obstetrical care quality? Am J Obstet Gynecol. 2019;220(4):395.e1–395.e12.
Al-Wassia H, Saber M. Admission of term infants to the neonatal intensive care unit in a Saudi tertiary teaching hospital: cumulative incidence and risk factors. Ann Saudi Med. 2017;37(6):420–4.
Nigg JT. Attention-deficit/hyperactivity disorder and adverse health outcomes. Clin Psychol Rev. 2013;33(2):215–28.
VanderWeele TJ. Principles of confounder selection. Eur J Epidemiol. 2019;34(3):211–9.
D’onofrio BM, et al. Critical need for family-based, quasi-experimental designs in integrating genetic and social science research. Am J Public Health. 2013;103(S1):S46–S55.
Lahey BB, D’Onofrio BM. All in the family: comparing siblings to test causal hypotheses regarding environmental influences on behavior. Curr Dir Psychol Sci. 2010;19(5):319–23.
Sujan AC, et al. Annual research review: maternal antidepressant use during pregnancy and offspring neurodevelopmental problems—a critical review and recommendations for future research. J Child Psychol Psychiatry. 2019;60(4):356–76.
Sjölander A, et al. Carryover effects in sibling comparison designs. Epidemiology. 2016;27(6):852–8.
Smith GD. Assessing intrauterine influences on offspring health outcomes: can epidemiological studies yield robust findings? Basic Clin Pharmacol Toxicol. 2008;102(2):245–56.
Yoshida K, Solomon DH, Kim SC. Active-comparator design and new-user design in observational studies. Nat Rev Rheumatol. 2015;11(7):437–41.
Lipsitch M, Tchetgen ET, Cohen T. Negative controls: a tool for detecting confounding and bias in observational studies. Epidemiology (Cambridge, Mass). 2010;21(3):383.
Sørensen MJ, et al. Antidepressant exposure in pregnancy and risk of autism spectrum disorders. Clin Epidemiol. 2013;5:449.
Sujan AC, et al. Associations of maternal antidepressant use during the first trimester of pregnancy with preterm birth, small for gestational age, autism spectrum disorder, and attention-deficit/hyperactivity disorder in offspring. JAMA. 2017;317(15):1553–622.
Morales DR, et al. Antidepressant use during pregnancy and risk of autism spectrum disorder and attention deficit hyperactivity disorder: systematic review of observational studies and methodological considerations. BMC Med. 2018;16(1):6.
Lawlor DA, Tilling K, Davey Smith G. Triangulation in aetiological epidemiology. Int J Epidemiol. 2016;45(6):1866–86.
Chang WS, et al. Maternal pregnancy-induced hypertension increases the subsequent risk of transient tachypnea of the newborn: a nationwide population-based cohort study. Taiwan J Obstet Gynecol. 2018;57(4):546–50.
Man KKC, et al. Prenatal antidepressant use and risk of attention-deficit/hyperactivity disorder in offspring: population based cohort study. BMJ. 2017;357:j2350.
Barker DJ. Fetal origins of coronary heart disease. BMJ. 1995;311(6998):171–4.
Thorpe PG, et al. Medications in the first trimester of pregnancy: most common exposures and critical gaps in understanding fetal risk. Pharmacoepidemiol Drug Saf. 2013;22(9):1013–8.
Ross EJ, et al. Developmental consequences of fetal exposure to drugs: what we know and what we still must learn. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2015;40(1):61–87.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Research reported in this publication was supported by the Swedish Research Council (no. 2018-02599 to Larsson and no. 2018-02679 to D’Onofrio), the Swedish Brain Foundation (Viktorin and no. FO2018-0273 to Larsson) and the National Institute on Drug Abuse of the National Institutes of Health under award number R00DA040727 (Quinn) and R01DA048042 (D’Onofrio, Quinn, Oberg). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest
HL has served as a speaker for Evolan Pharma and Shire and has received research grants from Shire, all outside the submitted work. SC has received honoraria and reimbursement of travel and accommodation expenses for lectures from the nonprofit associations Association for Child and Adolescent Central Health, Canadian ADHD Alliance Resource (CADDRA), and BAP and from Healthcare Convention for educational activity on ADHD. BD has received reimbursement of travel and accommodation expenses for CADDRA and Children and Adults with Attention-Deficit/Hyperactivity Disorder. LL, ACS, AB, ZC, PQ, AV, and ASÖ have no conflicts of interest that are directly relevant to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, L., Sujan, A.C., Butwicka, A. et al. Associations of Prescribed ADHD Medication in Pregnancy with Pregnancy-Related and Offspring Outcomes: A Systematic Review. CNS Drugs 34, 731–747 (2020). https://doi.org/10.1007/s40263-020-00728-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-020-00728-2