Abstract
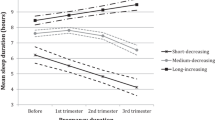
Poor sleep and excessive weight gain of pregnant women are associated with maternal outcomes. However, it’s unknown regarding their effects of each other in pregnant women. This cohort study aimed to identify the trajectories of sleep quality and their associations with excessive gestational weight gain during pregnancy. Data of 403 pregnant women were collected at three visiting points: early pregnancy, between 10 and 17 weeks, mid-pregnancy, between 18 and 21 weeks, and late pregnancy: 28–32 weeks of pregnancy. Sleep quality was examined by the Pittsburgh sleep quality index. A semiparametric mixture model was used to estimate the patterns of sleep quality throughout the pregnancy. Two trajectories were identified as good-to-poor group (76.42%) and constant poor group (23.57%), respectively. It was observed that poor sleep quality was associated with excessive gestational weight gain in both groups. Poor sleep quality during late pregnancy in good-to-poor group predicted excessive gestational weight gain (adjusted Odds Ratio 3.47, 95% CI 1.25, 9.62). In contrast, the relationship was established even at mid-pregnancy in constant poor group (adjusted Odds Ratio 3.12, 95% CI 1.06, 9.19). Results from this study showed that most of pregnant women reported decreased sleep quality, however, a minority reported stable–poor sleep quality throughout pregnancy. Poor sleep quality was associated with excessive gestational weight gain during pregnancy. In comparison, those pregnant women with stable–poor sleep quality had a greater risk to get excessive gestational weight gain.


Similar content being viewed by others
References
Cai S, Tan S, Gluckman PD, Godfrey KM, Saw SM, Teoh OH, et al. Sleep quality and nocturnal sleep duration in pregnancy and risk of gestational diabetes Mellitus. Sleep. 2017;40(2):zsw058. https://doi.org/10.1093/sleep/zsw058.
Wolynczyk-Gmaj D, Rozanska-Waledziak A, Ziemka S, Ufnal M, Brzezicka A, Gmaj B, et al. Insomnia in pregnancy is associated with depressive symptoms and eating at night. J Clin Sleep Med. 2017;13:1171–6.
Signal TL, Gander PH, Sangalli MR, Travier N, Firestone RT, Tuohy JF. Sleep duration and quality in healthy nulliparous and multiparous women across pregnancy and post-partum. Aust N Z J Obstet Gynaecol. 2007;47:16–22.
Hung H-M, Ko S-H, Chen C-H. The association between prenatal sleep quality and obstetric outcome. J Nurs Res. 2014;22:147–54.
Saadati F, Sehhatiei Shafaei F, Mirghafourvand M. Sleep quality and its relationship with quality of life among high-risk pregnant women (gestational diabetes and hypertension). J Matern Fetal Neona. 2018;31:150–7.
Khanolkar AR, Hanley GE, Koupil I, Janssen PA. IOM guidelines for gestational weight gain: how well do they predict outcomes across ethnic groups? Ethnicity Health. 2009;2017:1–16.
McBain RD, Dekker GA, Clifton VL, Mol BW, Grzeskowiak LE. Impact of inter-pregnancy BMI change on perinatal outcomes: a retrospective cohort study. Eur J Obstet Gynecol Reprod Biol. 2016;205:98–104.
Swank ML, Caughey AB, Farinelli CK, Main EK, Melsop KA, Gilbert WM, et al. The impact of change in pregnancy body mass index on the development of gestational hypertensive disorders. J Perinatol. 2014;34:181–5.
Gay CL, Richoux SE, Beebe KR, Lee KA. Sleep disruption and duration in late pregnancy is associated with excess gestational weight gain among overweight and obese women. Birth. 2017;44:173–80.
Facco FL, Kramer J, Ho KH, Zee PC, Grobman WA. Sleep disturbances in pregnancy. Obstet Gynecol. 2010;115:77–83.
Mota J, Vale S. Associations between sleep quality with cardiorespiratory fitness and BMI among adolescent girls. Am J Hum Biol. 2010;22:473–5.
Park SK, Jung JY, Oh C-M, McIntyre RS, Lee J-H. Association between sleep duration, quality and body mass index in the korean population. J Clin Sleep Med. 2018;14:1353–60.
Zhou B. Coorperative meta-analysis group of China obesity task F [Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population]. Zhonghua Liu Xing Bing Xue Za Zhi. 2002;23:5–10.
Wang S-S, Lay S, Yu H-N, Shen S-R, Dietary Guidelines for Chinese Residents. Comments and comparisons. J Zhejiang Univ Sci B. 2016;17:649–56.
Smyth C. The pittsburgh sleep quality index (PSQI). Insight. 2000;25:97–8.
Sut HK, Asci O, Topac N. Sleep quality and health-related quality of life in pregnancy. J Perinat Neonatal Nurs. 2016;34:302–9.
Heo M, Kim N, Faith MS. Statistical power as a function of Cronbach alpha of instrument questionnaire items. BMC Med Res Methodol. 2015;15:86.
Little RJ, Wang Y. Pattern-mixture models for multivariate incomplete data with covariates. Biometrics. 1996;52:98–111.
Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Method Res. 2001;29:374–93.
Rangan A, Zheng M, Olsen NJ, Rohde JF, Heitmann BL. Shorter sleep duration is associated with higher energy intake and an increase in BMI z-score in young children predisposed to overweight. Int J Obes (Lond). 2018;42:59–64.
Little RJA, Rubin DB. Statistical analysis with missing data. Hoboken: Wiley; 2019 (cited).
Tomfohr LM, Buliga E, Letourneau NL, Campbell TS, Giesbrecht GF. Trajectories of sleep quality and associations with mood during the perinatal period. Sleep. 2015;38:1237–45.
Morin CM, Belanger L, LeBlanc M, Ivers H, Savard J, Espie CA, et al. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med. 2009;169:447–53.
Wilkerson AK, Uhde TW. Perinatal sleep problems: causes, complications, and management. Obstet Gynecol Clin North Am. 2018;45:483–94.
Yang Y, Mao J, Ye Z, Zeng X, Zhao H, Liu Y, et al. Determinants of sleep quality among pregnant women in China: a cross-sectional survey. J Matern Fetal Neona. 2018;31:2980–5.
Ribeiro MC, Nakamura MU, Torloni MR, Scanavino MdT, Forte BMB, Mancini PE, et al. [Sleep quality in overweight pregnant women]. Qualidade do sono em gestantes com sobrepeso. Rev Bras Ginecol Obstet. 2015;37:359–65.
Eleuteri S, Norton MC, Livi F, Grano C, Falaschi P, Violani C, et al. Sleep quality as predictor of BMI in non-depressed caregivers of people with dementia. Eat Weight Disord. 2018;23:553–60.
Acknowledgements
The authors acknowledge the study participants for their contributions in making this study possible.
Funding
The study was funded by grants from National Natural Science Foundation of China (81673183, 81874266, 81602860), key project from Shanghai Municipal Science and Technology Commission (18411951600), the Science and Technology Funds from Pudong New Area, Shanghai (PKJ2017-Y01), the Research Funds from Shanghai Jiao Tong University School of Medicine (20170509-1), the Scientific Research Development Funds from Xinhua Hospital, Shanghai Jiao Tong University School of Medicine (HX0251), and the Shanghai Health and Family Planning Committee Research Project (201540165).
Author information
Authors and Affiliations
Contributions
JL: data analysis, manuscript writing. QZ: data collection. ST: manuscript editing. XS: data collection. JH: protocol, manuscript writing, manuscript editing. SL: project development, manuscript writing, manuscript editing.
Corresponding authors
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Ethical approval
The study was approved by the research and ethics committee of Shanghai First Maternity and Infant Hospital, Tongji University School of Medicine (LS1416).
Informed consent
All the participants who signed the written informed consent form were invited to participate in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lyu, J., Zhu, Q., Tong, S. et al. Trajectories of sleep quality and associations with excessive gestational weight gain during pregnancy. Sleep Biol. Rhythms 18, 249–257 (2020). https://doi.org/10.1007/s41105-020-00266-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-020-00266-w