Abstract
Purpose of Review
The purpose of this manuscript is to provide a comprehensive review of postdural puncture headache (PDPH) with a focus on epidemiology, pathophysiology, treatment, and prophylaxis.
Recent Findings
PDPH is an adverse iatrogenic complication of neuraxial anesthesia that occurs following inadvertent puncture of the dura after epidural or spinal anesthesia. The overall incidence of PDPH after neuraxial procedures varies from 6 to 36%. The occurrence of PDPH can lead to increased patient morbidity, delayed discharge, and increased readmission. PDPH is a self-limiting postural headache that most often will resolve within 1 week, without need for treatment. Various prophylactic measures have been studied; however, more studies have been recommended to be undertaken in order to establish a proven benefit.
Summary
For mild PDPH, conservative treatments are currently focused around bed rest, as well as oral caffeine. For moderate-to-severe PDPH, epidural blood patch (EBP) remains the most effective treatment; however, this invasive treatment is not without inherent risks. Further less invasive treatments have been explored such as epidural saline, dextran 40 mg solutions, hydration, caffeine, sphenopalatine ganglion blocks, greater occipital nerve blocks, and surgical closure of the gap; all have shown promise. Further studies are essential to prove efficacy as well as safety over the proven treatment of epidural blood patches. There is still limited evidence in literature about the understanding of PDPH and optimal treatment.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bier A. Experiments on the spinal cord cocainization. Arch Klin Chir Ver Dtsch Z Chir. 1899;51:361–8.
Katz D, Beilin Y. Review of the alternatives to epidural blood patch for treatment of postdural puncture headache in the parturient. Anesth Analg. 2017;124(4):1219–28.
Kwak K-H. Postdural puncture headache. Korean J Anesthesiol. 2017;70(2):136–43.
Kocarev M, Khalid F, Khatoon F, Fernando R. Neuraxial labor analgesia: a focused narrative review of the 2017 literature. Curr Opin Anaesthesiol. 2018;31(3):251–7.
•• Nath S, Koziarz A, Badhiwala JH, Alhazzani W, Jaeschke R, Sharma S, et al. Atraumatic versus conventional lumbar puncture needles: a systematic review and meta-analysis. Lancet. 2018;391(10126):1197–204. This is a great review and meta-analysis discussing lumbar puncture needles.
Van de Velde M, Schepers R, Berends N, Vandermeersch E, De Buck F. Ten years of experience with accidental dural puncture and post-dural puncture headache in a tertiary obstetric anaesthesia department. Int J Obstet Anesth. 2008;17(4):329–35.
• Arevalo-Rodriguez I, Muñoz L, Godoy-Casasbuenas N, Ciapponi A, Arevalo JJ, Boogaard S, et al. Needle gauge and tip designs for preventing post-dural puncture headache (PDPH). Cochrane Database Syst Rev. 2017;4:CD010807. This is a great paper that discusses needle gauge and tip designs to prevent post dural puncture headache.
• Xu H, Liu Y, Song W, Kan S, Liu F, Zhang D, et al. Comparison of cutting and pencil-point spinal needle in spinal anesthesia regarding postdural puncture headache: a meta-analysis. Medicine (Baltimore). 2017;96(14):e6527. This is a great paper that compares pencil-point spinal needle in spinal anesthesia related to postdural puncture headache.
Zorilla-Vaca A, Makkar JK. Effectiveness of lateral decubitus position for preventing post-dural puncture headache: a meta-analysis. Pain Physician. 2017;20(4):E521–9.
Davoudi M, Tarbiat M, Ebadian MR, Hajian P. Effect of position during spinal anesthesia on postdural puncture headache after cesarean section: a prospective, single-blind randomized clinical trial. Anesth Pain Med. 2016;6(4):e35486.
Morewood GH. A rational approach to the cause, prevention and treatment of postdural puncture headache. CMAJ. 1993;149(8):1087–93.
Amorim JA, Gomes De Barros MV, Valença MM. Post-dural (post-lumbar) puncture headache: risk factors and clinical features. Cephalalgia. 2012;32(12):916–23.
• Choi P, Galinski S, Takeuchi L, Lucas S, Tamayo C, Jadad A. PDPH is a common complication of neuraxial blockade in parturients: a meta-analysis of obstetrical studies. Can J Anaesth. 2003;50(5):460–9. This is a great paper that discusses complications of neuraxial blockade.
Wu CL, Rowlingson AJ, Cohen SR, Michaels RK, Courpas GE, Joe EM, et al. Gender and post-dural puncture headache. Anesthesiology. 2006;105(3):613–8.
Haller G, Cornet J, Boldi M-O, Myers C, Savoldelli G, Kern C. Risk factors for post-dural puncture headache following injury of the dural membrane: a root-cause analysis and nested case-control study. Int J Obstet Anesth. 2018;36:17–27.
Faure E, Moreno R, Thisted R. Incidence of postdural puncture headache in morbidly obese parturients. Reg Anesth. 19(5):361–3.
Lee SI, Sandhu S, Djulbegovic B, Mhaskar RS. Impact of spinal needle type on postdural puncture headache among women undergoing cesarean section surgery under spinal anesthesia: a meta-analysis. J Evid Based Med. 2018;11(3):136–44.
Zorrilla-Vaca A, Healy R, Zorrilla-Vaca C. Finer gauge of cutting but not pencil-point needles correlate with lower incidence of post-dural puncture headache: a meta-regression analysis. J Anesth. 2016;30(5):855–63.
Zorrilla-Vaca A, Mathur V, Wu CL, Grant MC, Zorrilla-Vaca A, Mathur V, et al. The impact of spinal needle selection on postdural puncture headache: a meta-analysis and meta regression of randomized studies. Reg Anesth Pain Med. 2018;43(5):502–8.
Angle P, Thompson D, Halpern S, Wilson DB. Second stage pushing correlates with headache after unintentional dural puncture in parturients. Can J Anesth. 1999;46(9):861–6.
Richman JM, Joe EM, Cohen SR, Rowlingson AJ, Michaels RK, Jeffries MA, et al. Bevel direction and postdural puncture headache: a meta-analysis. Neurologist. 2006;12(4):224–8.
• Amrhein TJ, Parivash SN, Gray L, Kranz PG. Incidence of inadvertent dural puncture during CT fluoroscopy-guided interlaminar epidural corticosteroid injections in the cervical spine: an analysis of 974 cases. AJR Am J Roentgenol. 2017;209(3):656–61. This is a good paper that analyzes the incidence of inadvertant dural puncture.
Manchikanti L, Malla Y, Cash KA, Pampati V. Do the gaps in the ligamentum flavum in the cervical spine translate into dural punctures? An analysis of 4,396 fluoroscopic interlaminar epidural injections. Pain Physician. 2015;18(3):259–66.
Park JY, Karm MH, Kim DH, Lee JY, Yun HJ, Suh JH. Optimal angle of contralateral oblique view in cervical interlaminar epidural injection depending on the needle tip position. Pain Physician. 2017;20(1):E169–75.
Lai YC, Chia YY, Lien WH. Reversal of progressive conscious disturbance with epidural blood patch for cerebrospinal fluid leakage at C2 level. Pain Physician. 2017;20(3):E465–8.
Jeon JY, Jeong YM, Lee SW, Kim JH, Choi HY, Ahn Y. The termination level of the dural sac relevant to caudal epidural block in lumbosacral transitional vertebrae: a comparison between sacralization and lumbarization groups. Pain Physician. 2018;21(1):73–82.
•• Abrecht CR, Saba R, Greenberg P, Rathmell JP, Urman RD. A contemporary medicolegal analysis of outpatient interventional pain procedures: 2009-2016. Anesth Analg. 2019. This is a good paper that analyzes outpatient interventional pain procedures.
Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. A prospective evaluation of complications of 10,000 fluoroscopically directed epidural injections. Pain Physician. 2012;15(2):131–40.
Figueiera HD, Guimaraes J, Sousa AL, Regalado AM. Pneumocephalus following unidentified dural puncture: a case report with an unusual neurological presentation. Pain Physician. 2017;20(2):E329–34.
Neuman SA, Eldrige JS, Qu W, Freeman ED, Hoelzer BC. Post dural puncture headache following intrathecal drug delivery system placement. Pain Physician. 2013;16(2):101–7.
Bradbury CL, Singh SI, Badder SR, Wakely LJ, Jones PM. Prevention of post-dural puncture headache in parturients: a systematic review and meta-analysis. Acta Anaesthesiol Scand. 2013;57(4):417–30.
Hustak EC, Engle MP, Viswanathan A, Koyyalagunta D. Lumbar subarachnoid hematoma following an epidural blood patch for meningeal puncture headache related to the implantation of an intrathecal drug delivery system. Pain Physician. 2014;17:E405–11.
Ahmed SV, Jayawarna C, Jude E. Post lumbar puncture headache: diagnosis and management. Postgrad Med J. 2006;82(973):713–6.
Arevalo-Rodriguez I, Ciapponi A, Roqué i Figuls M, Muñoz L, Bonfill CX. Posture and fluids for preventing post-dural puncture headache. Cochrane Database Syst Rev. 2016;3:CD009199.
Basurto Ona X, Osorio D, Bonfill CX. Drug therapy for treating post-dural puncture headache. Cochrane Database Syst Rev. 2015;7:CD007887.
Manchikanti L, Soin A, Mann DP, Bakshi S, Pampati V, Hirsch JA. Reversal of growth of utilization of interventional techniques in managing chronic pain in Medicare population post affordable care act. Pain Physician. 2017;20(6):551–67.
Manchikanti L, Soin A, Mann DP, Bakshi S, Pampati V, Hirsch JA. Utilization patterns of facet joint interventions in managing spinal pain: a retrospective cohort study in the U.S. fee-for-service Medicare population. Curr Pain Headache Rep. 2019;in press.
Manchikanti MV, Manchikanti L, Kaye AD, Pampati V, Hirsch JA. Usage patterns of sacroiliac joint injections-a comparative evaluation of pre and post Affordable Care Act in Medicare population. IPM Rep. 2018;2(5):157–66.
Manchikanti L, Soin A, Mann DP, Bakshi S, Pampati V, Hirsch JA. Comparative analysis of utilization of epidural procedures in managing chronic pain in the Medicare population: pre and post Affordable Care Act. Spine (Phila Pa 1976). 2019;44(3):220–32.
Manchikanti L, Pampati V, Benyamin RM, Hirsch JA. Declining utilization of percutaneous epidural adhesiolysis in Medicare population: evidence-based or over-regulated? IPM Rep. 2018;2(1):9–18.
Lee JH, Kim DH, Kim DH, Shin KH, Park SJ, Lee GJ, et al. Comparison of clinical efficacy of epidural injection with or without steroid in lumbosacral disc herniation: a systematic review and meta-analysis. Pain Physician. 2018;21(5):449–68.
Lee JH, Shin KH, Park SJ, Lee GJ, Lee CH, Kim DH, et al. Comparison of clinical efficacy between transforaminal and interlaminar epidural injections in lumbosacral disc herniation: a systematic review and meta-analysis. Pain Physician. 2018;21(5):433–48.
Nagel SJ, Reddy CG, Frizon LA, Holland MT, Machado AG, Gillies GT, et al. Intrathecal therapeutics: device design, access methods, and complication mitigation. Neuromodulation. 2018;21:625–40.
Manchikanti L, Kaye AM, Knezevic NN, McAnally H, Trescot AM, Blank S, et al. Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2017;20(2S):S3–S92.
Kaye AD, Jones MR, Kaye AM, Ripoll JG, Galan V, Beakley BD, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 1. Pain Physician. 2017;20(2S):S93–S109.
Kaye AD, Jones MR, Kaye AM, Ripoll JG, Jones DE, Galan V, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 2. Pain Physician. 2017;20(2S):S111–33.
Manchikanti L, Sanapati J, Benyamin RM, Atluri S, Kaye AD, Hirsch JA. Reframing the prevention strategies of the opioid crisis: focusing on prescription opioids, fentanyl, and heroin epidemic. Pain Physician. 2018;21(4):309–26.
Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths-United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018;67:1419–27.
Chakravarthy K, Manchikanti L, Kaye AD, Christo PJ. Reframing the role of neuromodulation therapy in the chronic pain treatment paradigm. Pain Physician. 2018;21(6):507–13.
Manchikanti L, Pampati V, Kaye AD, Hirsch JA. Cost utility analysis of cervical therapeutic medial branch blocks in managing chronic neck pain. Int J Med Sci. 2017;14(13):1307–16.
Manchikanti L, Pampati V, Kaye AD, Hirsch JA. Therapeutic lumbar facet joint nerve blocks in the treatment of chronic low back pain: cost utility analysis based on a randomized controlled trial. Korean J Pain. 2018;31(1):27–38.
Manchikanti L, Pampati V, Benyamin RM, Hirsch JA. Cost utility analysis of lumbar interlaminar epidural injections in the treatment of lumbar disc herniation, central spinal stenosis, and axial or discogenic low back pain. Pain Physician. 2017;20(4):219–28.
Beall DP, Tutton SM, Murphy K, Olan W, Warner CB, Test JB. Analysis of reporting bias in vertebral augmentation. Pain Physician. 2017;20(7):E1081–90.
Manchikanti L, Boswell MV, Kaye AD, Helm S II, Hirsch JA. Therapeutic role of placebo: evolution of a new paradigm in understanding research and clinical practice. Pain Physician. 2017;20(5):363–86.
Gupta A, Huettner DP, Dukewich M. Comparative effectiveness review of cooled versus pulsed radiofrequency ablation for the treatment of knee osteoarthritis: a systematic review. Pain Physician. 2017;20(3):155–71.
Manchikanti L, Benyamin RM, Falco FJ, Kaye AD, Hirsch JA. Do epidural injections provide short- and long-term relief for lumbar disc herniation? A systematic review. Clin Orthop Relat Res. 2015;473(6):1940–56.
Guo JR, Jin XJ, Shen HC, Wang H, Zhou X, Liu XQ, et al. A comparison of the efficacy and tolerability of the treatments for sciatica: a network meta-analysis. Ann Pharmacother. 2017;51(12):1041–52.
Rysavy M. Evidence-based medicine: a science of uncertainty and an art of probability. AMA J Ethics. 2013;15(1):4–8.
Manchikanti L, Singh V, Pampati V, Falco FJE, Hirsch JA. Comparison of the efficacy of caudal, interlaminar, and transforaminal epidural injections in managing lumbar disc herniation: is one method superior to the other? Korean J Pain. 2015;28(1):11–21.
Lewis R, Williams N, Matar HE, Din N, Fitzsimmons D, Phillips C, et al. The clinical effectiveness and cost effectiveness of management strategies for sciatica: systematic review and economic model. Health Technol Assess. 2011;15(39):1–578.
Shen J, Xu S, Xu S, Ye S, Hao J. Fusion or not for degenerative lumbar spinal stenosis: a meta-analysis and systematic review. Pain Physician. 2018;21(1):1–8.
Song D, He A, Xu R, Xiu X, Wei Y. Efficacy of pain relief in different postherpetic neuralgia therapies: a network meta-analysis. Pain Physician. 2018;21(1):19–32.
Manchikanti L, Soin A, Benyamin RM, Singh V, Falco FJ, Calodney AK, et al. An update of the systematic appraisal of the accuracy and utility of discography in chronic spinal pain. Pain Physician. 2018;21(2):91–110.
Sanapati J, Manchikanti L, Atluri S, Jordan S, Albers SL, Pappolla MA, et al. Do regenerative medicine therapies provide long-term relief in chronic low back pain: a systematic review and metaanalysis. Pain Physician. 2018;21(6):515–40.
Helm S II, Simopoulos TT, Stojanovic M, Abdi S, El Terany MA. Effectiveness of thermal annular procedures in treating discogenic low back pain. Pain Physician. 2017;20(6):447–70.
Fu X, Tang L, Wang C, Li M, Wu H, Li J, et al. A network meta-analysis to compare the efficacy of steroid and antiviral medications for facial paralysis from Bell’s palsy. Pain Physician. 2018;21(6):559–69.
Cho JH, Lee JH, Song KS, Hong JY, Joo YS, Lee DH, et al. Treatment outcomes for patients with failed back surgery. Pain Physician. 2017;20(1):E29–43.
Chaichian S, Kabir A, Mehdizadehkashi A, Rahmani K, Moghimi M, Moazzami B. Comparing the efficacy of surgery and medical therapy for pain management in endometriosis: a systematic review and meta-analysis. Pain Physician. 2017;20(3):185–95.
Gudala K, Bansal D, Vatte R, Ghai B, Schifano F, Boya C. High prevalence of neuropathic pain component in patients with low back pain: evidence from meta-analysis. Pain Physician. 2017;20(5):343–52.
Dodge HS, Ekhator NN, Jefferson-Wilson L, Fischer M, Jansen I, Horn PS, et al. Cigarette smokers have reduced risk for post-dural puncture headache. Pain Physician. 2013;16(1):E25–30.
Zhang D, Chen L, Chen X, Wang X, Li Y, Ning G, et al. Lower incidence of postdural puncture headache using Whitacre spinal needles after spinal anesthesia: a meta-analysis. Headache. 2016;56(3):501–10.
Lim G, Zorn JM, Dong YJ, DeRenzo JS, Waters JH. Subdural hematoma associated with labor epidural analgesia. Reg Anesth Pain Med. 2016;41(5):628–31.
Darvish B, Dahlgren G, Irestedt L, Magnuson A, Möller C, Gupta A. Auditory function following post-dural puncture headache treated with epidural blood patch. A long-term follow-up. Acta Anaesthesiol Scand. 2015;59(10):1340–54.
Webb C, Weyker P, Zhang L, Stanley S, Coyle T, Tang T, et al. Unintentional dural puncture with a Tuohy needle increases risk of chronic headache. Anesth Analg. 2012;115(1):124–32.
Nishio I, Williams BA, Williams JP. Diplopia: a complication of dural puncture. Anesthesiology. 2004;100(1):158–64.
Mullane D, Tan T. Three cerebral venous sinus thromboses following inadvertent dural puncture: a case series over an eight-year period. Can J Anesth Can. 2014;61(12):1134–5.
Gaiser RR. Postdural puncture headache. Anesthesiol Clin. 2017;35(1):157–67.
Baratloo A, Rouhipour A, Forouzanfar MM, Safari S, Amiri M, Negida A. The role of caffeine in pain management: a brief literature review. Anesthesiol Pain Med. 2016;6(3):e33193.
Feuerstein TJ, Zeides A. Theophylline relieves headache following lumbar puncture. Placebo-controlled, double-blind pilot study. Klin Wochenschr. 1986;64(5):216–8.
Noyan Ashraf MA, Sadeghi A, Azarbakht Z, Salehi S, Hamediseresht E. Evaluation of intravenous hydrocortisone in reducing headache after spinal anesthesia: a double blind controlled clinical study [corrected]. Middle East J Anaesthesiol. 2007;19(2):415–22.
Kroin JS, Nagalla SKS, Buvanendran A, McCarthy RJ, Tuman KJ, Ivankovich AD. The mechanisms of intracranial pressure modulation by epidural blood and other injectates in a postdural puncture rat model. Anesth Analg. 2002;95(2):423–9.
Booth JL, Pan PH, Thomas JA, Harris LC, D’Angelo R. A retrospective review of an epidural blood patch database: the incidence of epidural blood patch associated with obstetric neuraxial anesthetic techniques and the effect of blood volume on efficacy. Int J Obstet Anesth. 2017;29:10–7.
Roy-Gash F, Engrand N, Lecarpentier E, Bonnet MP. Intrathecal hematoma and arachnoiditis mimicking bacterial meningitis after an epidural blood patch. Int J Obstet Anesth. 2017;32:77–81.
Devroe S, Van de Velde M, Demaerel P, Van Calsteren K. Spinal subdural haematoma after an epidural blood patch. Int J Obstet Anesth. 2015;24(3):288–9.
Carlswärd C, Darvish B, Tunelli J, Irestedt L. Chronic adhesive arachnoiditis after repeat epidural blood patch. Int J Obstet Anesth. 2015;24(3):280–3.
Scavone BM, Wong CA, Sullivan JT, Yaghmour E, Sherwani SS, McCarthy RJ. Efficacy of a prophylactic epidural blood patch in preventing post dural puncture headache in parturients after inadvertent dural puncture. Anesthesiology. 2004;101(6):1422–7.
Paech MJ, Doherty DA, Christmas T, Wong CA, Epidural Blood Patch Trial Group. The volume of blood for epidural blood patch in obstetrics. Anesth Analg. 2011;113(1):126–33.
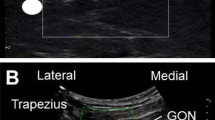
Niraj G, Kelkar A, Girotra V. Greater occipital nerve block for postdural puncture headache (PDPH): a prospective audit of a modified guideline for the management of PDPH and review of the literature. J Clin Anesth. 2014;26(7):539–44.
Cohen S, Levin D, Mellender S, Zhao R, Patel P, Grubb W, et al. Topical sphenopalatine ganglion block compared with epidural blood patch for postdural puncture headache management in postpartum patients: a retrospective review. Reg Anesth Pain Med. 2018;43(8):880–4.
Hakim SM. Cosyntropin for prophylaxis against postdural puncture headache after accidental dural puncture. Anesthesiology. 2010;113(2):413–20.
Fattahi Z, Hadavi SMR, Sahmeddini MA. Effect of ondansetron on post-dural puncture headache (PDPH) in parturients undergoing cesarean section: a double-blind randomized placebo-controlled study. J Anesth. 2015;29(5):702–7.
Pazoki S, Modir H, Kamali A, Zamani A, Shahidani M. Ondansetron 8 mg and 4 mg with normal saline against post-operative headache and nausea/vomiting after spinal anesthesia: a randomized double-blind trial. Med Gas Res. 2018;8(2):48–53.
Masoudifar M, Aghadavoudi O, Adib S. Effect of venous dexamethasone, oral caffeine and acetaminophen on relative frequency and intensity of postdural puncture headache after spinal anesthesia. Adv Biomed Res. 2016;5(1):66.
Agerson AN, Scavone BM. Prophylactic epidural blood patch after unintentional dural puncture for the prevention of postdural puncture headache in parturients. Anesth Analg. 2012;115(1):133–6.
Rana K, Jenkins S, Rana M. Insertion of an intrathecal catheter following a recognised accidental dural puncture reduces the need for an epidural blood patch in parturients: an Australian retrospective study. Int J Obstet Anesth. 2018;36:11–6.
Verstraete S, Walters MA, Devroe S, Roofthooft E, Van de Velde M. Lower incidence of post-dural puncture headache with spinal catheterization after accidental dural puncture in obstetric patients. Acta Anaesthesiol Scand. 2014;58(10):1233–9.
Kaddoum R, Motlani F, Kaddoum RN, Srirajakalidindi A, Gupta D, Soskin V. Accidental dural puncture, postdural puncture headache, intrathecal catheters, and epidural blood patch: revisiting the old nemesis. J Anesth. 2014;28(4):628–30.
Jagannathan DK, Arriaga AF, Elterman KG, Kodali BS, Robinson JN, Tsen LC, et al. Effect of neuraxial technique after inadvertent dural puncture on obstetric outcomes and anesthetic complications. Int J Obstet Anesth. 2016;25:23–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Riki Patel, Ivan Urits, Vwaire Orhurhu, Mariam Salisu Orhurhu, Jacquelin Peck, Emmanuel Ohuabunwa, Andrew Sikorski, Armeen Mehrabani, Laxmaiah Manchikanti, Rachel J. Kaye, John A. Helmstetter, and Omar Viswanath declare no conflict of interest. Alan Kaye is a Section Editor for Current Headache and Pain Reports. He has not been involved in the editorial handling of this manuscript. Dr. Kaye is also a speaker for Merck.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Other Pain
Rights and permissions
About this article
Cite this article
Patel, R., Urits, I., Orhurhu, V. et al. A Comprehensive Update on the Treatment and Management of Postdural Puncture Headache. Curr Pain Headache Rep 24, 24 (2020). https://doi.org/10.1007/s11916-020-00860-0
Published:
DOI: https://doi.org/10.1007/s11916-020-00860-0