Abstract
Purpose of Review
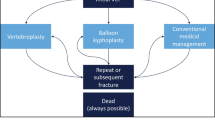
To review the utilization patterns of vertebral augmentation procedures in the US Medicare population from 2004 to 2017 surrounding concurrent developments in the literature and the enactment of the Affordable Care Act (ACA).
Recent Findings
The analysis of vertebroplasty and kyphoplasty utilization patterns was carried out using specialty utilization data from the Centers for Medicare and Medicaid Services Database. Of note, over the period of time between 2009 and 2017, the number of people aged 65 or older showed a 3.2% rate of annual increase, and the number of Medicare beneficiaries increased by 27.6% with a 3.1% rate of annual increase. Concurrently, vertebroplasty utilization decreased 72.8% (annual decline of 15% per 100,000 Medicare beneficiaries), and balloon kyphoplasty utilization decreased 19% (annual decline of 2.6% per 100,000 Medicare beneficiaries). This translates to a 38.3% decrease in vertebroplasty and balloon kyphoplasty utilization (annual decline of 5.9% per 100,000 Medicare beneficiaries) from 2009 to 2017. By contrast, from 2004 to 2009, there was a total 188% increase in vertebroplasty and balloon kyphoplasty utilization (annual increase rate of 23.6% per 100,000 Medicare beneficiaries). The majority of vertebroplasty procedures were done by radiologists, and the majority of kyphoplasties were done by aggregate groups of spine surgeons.
Summary
These results illustrate a significant decline in vertebral augmentation procedures in the fee-for-service Medicare population between 2004 and 2017, with dramatic decreases following the publication of two 2009 trials that failed to demonstrate benefit of vertebroplasty over sham and the enactment of the ACA.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hirsch JA, Chandra RV, Pampati V, Barr JD, Brook AL, Manchikanti L. Analysis of vertebral augmentation practice patterns: a 2016 update. J Neurointer Surg. 2016;8:1299–304.
Clerk-Lamalice O, Beall DP, Ong K, Lorio MP. ISASS policy 2018-vertebral augmentation: coverage indications, limitations, and/or medical necessity. Int J Spine Surg. 2019;13:1–10.
Mattie R, Laimi K, Yu S, Saltychev M. Comparing percutaneous vertebroplasty and conservative therapy for treating osteoporotic compression fractures in the thoracic and lumbar spine: a systematic review and meta-analysis. J Bone Joint Surg Am. 2016;98:1041–51.
Xiao H, Yang J, Feng X, Chen P, Li Y, Huang C, et al. Comparing complications of vertebroplasty and kyphoplasty for treating osteoporotic vertebral compression fractures: a meta-analysis of the randomized and non-randomized controlled studies. Eur J Orthop Surg Traumatol. 2015;25:S77–85.
Zhang H, Xu C, Zhang T, Gao Z, Zhang T. Does percutaneous vertebroplasty or balloon kyphoplasty for osteoporotic vertebral compression fractures increase the incidence of new vertebral fractures? A meta-analysis. Pain Physician. 2017;20:E13–28.
Beall D, Lorio MP, Yun BM, Runa MJ, Ong KL, Warner CB. Review of vertebral augmentation: an updated meta-analysis of the effectiveness. Int J Spine Surg. 2018;12:295–321.
Jensen ME, McGraw JK, Cardella JF, Hirsch JA. Position statement on percutaneous vertebral augmentation: a consensus statement developed by the American Society of Interventional and Therapeutic Neuroradiology, Society of Interventional Radiology, American Association of Neurological Surgeons/Congress of Neurological Surgeons, and American Society of Spine Radiology. J Neurointerv Surg. 2009;1:181–5.
Clark W, Bird P, Gonski P, Diamond TH, Smerdely P, McNeil H, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo controlled trial. Lancet. 2016;388:1408–16.
Hansen EJ, Simony A, Rousing R, Carreon LY, Tropp H, Andersen MO. Double blind placebo-controlled trial of percutaneous vertebroplasty (VOPE). Global Spine J. 2016;6:GO106.
Firanescu CE, de Vries J, Lodder P, Venmans A, Schoemaker MC, Smeets AJ, Donga E, Juttmann JR, Klazen CAH, Elgersma OEH, Jansen FH, Tielbeek AV, Boukrab I, Schonenberg K, van Rooij WJJ, Hirsch JA, Lohle PNM. Vertebroplasty versus sham procedure for painful acute osteoporotic vertebral compression fractures (VERTOS IV): randomised sham controlled clinical trial. BMJ 2018:k1551.
Yang EZ, Xu JG, Huang GZ, Xiao WZ, Liu XK, Zeng BF, et al. Percutaneous vertebroplasty versus conservative treatment in aged patients with acute osteoporotic vertebral compression fractures: a prospective randomized controlled clinical study. Spine (Phila Pa 1976). 2016;41:653–60.
Edidin AA, Ong KL, Lau E, Schmier JK, Kemner JE, Kurtz SM. Cost-effectiveness analysis of treatments for vertebral compression fractures. Appl Health Econ Health Policy. 2012;10:273–84.
Papanastassiou ID, Phillips FM, Van Meirhaeghe J, Berenson JR, Andersson GB, Chung G, et al. Comparing effects of kyphoplasty, vertebroplasty, and nonsurgical management in a systematic review of randomized and non-randomized controlled studies. Eur Spine J. 2012;21:1826–43.
Xiang GH, Tong MJ, Lou C, Zhu SP, Guo WJ, Ke CR. The role of unilateral balloon kyphoplasty for the treatment of patients with OVCFS: a systematic review and meta-analysis. Pain Physician. 2018;21:209–18.
Chen X, Guo W, Li Q, Ou Z, Lao Z, Liu Y, et al. Is unilateral percutaneous kyphoplasty superior to bilateral percutaneous kyphoplasty for osteoporotic vertebral compression fractures? Evidence from a systematic review of discordant meta-analyses. Pain Physician. 2018;21:327–36.
Rosian K, Hawlik K, Piso B. Efficacy assessment of radiofrequency ablation as a palliative pain treatment in patients with painful metastatic spinal lesions: a systematic review. Pain Physician. 2018;21:E467–76.
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557–68.
Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569–79.
Medicare Administrative Contractor Multijurisdictional Contractor Advisory Committee (CAC) meeting re Vertebral Augmentation 2019.
Beall DP, Chambers MR, Thomas S, Amburgy J, Webb JR Jr, Goodman BS, et al. Prospective and multicenter evaluation of outcomes for quality of life and activities of daily living for balloon kyphoplasty in the treatment of vertebral compression fractures: the EVOLVE trial. Neurosurgery. 2019;84:169–78.
National Institute for Health and Care Excellence. Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for treating osteoporotic vertebral compression fractures. April 24, 2013. https://www.nice.org.uk/guidance/ta279
Ong KL, Beall DP, Frohbergh M, Lau E, Hirsch JA. Were VCF patients at higher risk of mortality following the 2009 publication of the vertebroplasty “sham” trials? Osteoporos Int. 2018;29:375–83.
Edidin AA, Ong KL, Lau E, Kurtz SM. Mortality risk for operated and nonoperated vertebral fracture patients in the medicare population. J Bone Miner Res. 2011;26:617–26.
Chen AT, Cohen DB, Skolasky RL. Impact of nonoperative treatment, vertebroplasty, and kyphoplasty on survival and morbidity after vertebral compression fracture in the medicare population. J Bone Joint Surg Am. 2013;95:1729–36.
Lange A, Kasperk C, Alvares L, Sauermann S, Braun S. Survival and cost comparison of kyphoplasty and percutaneous vertebroplasty using German claims data. Spine (Phila Pa 1976). 2014;39:318–26.
Edidin AA, Ong KL, Lau E, Kurtz SM. Morbidity and mortality after vertebral fractures: comparison of vertebral augmentation and nonoperative management in the medicare population. Spine (Phila Pa 1976). 2015;40:1228–41.
Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, et al. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15:38–42.
Lau E, Ong K, Kurtz S, Schmier J, Edidin A. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am. 2008;90:1479–86.
Hirsch JA, Beall DP, Chambers MR, Andreshak TG, Brook AL, Bruel BM, et al. Management of vertebral fragility fractures: a clinical care pathway developed by a multispecialty panel using the RAND/UCLA appropriateness method. Spine J. 2018;18:2152–61.
Marcia S, Muto M, Hirsch JA, Chandra RV, Carter N, Crivelli P, et al. What is the role of vertebral augmentation for osteoporotic fractures? A review of the recent literature. Neuroradiology. 2018;60:777–83.
Chandra RV, Maingard J, Asadi H, Slater LA, Mazwi TL, Marcia S, et al. Vertebroplasty and kyphoplasty for osteoporotic vertebral fractures: what are the latest data? AJNR Am J Neuroradiol. 2018;39:798–806.
Barr JD, Jensen ME, Hirsch JA, JK MG, Barr RM, Brook AL, et al. Society of Interventional Radiology; American Association of Neurological Surgeons; Congress of Neurological Surgeons; American College of Radiology; American Society of Neuroradiology; American Society of Spine Radiology; Canadian Interventional Radiology Association; Society of Neurointerventional Surgery. Position statement on percutaneous vertebral augmentation: A consensus statement developed by the Society of Interventional Radiology (SIR), American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS), American College of Radiology (ACR), American Society of Neuroradiology (ASNR), American Society of Spine Radiology (ASSR), Canadian Interventional Radiology Association (CIRA), and the Society of NeuroInterventional Surgery (SNIS). J Vasc Interv Radiol. 2014;25:171–81.
Buchbinder R, Johnston RV, Rischin KJ, Homik J, Jones CA, Golmohammadi K, et al. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev. 2018 Apr 4;4:CD006349.
Clark W, Bird P, Diamond T, Gonski P, Gebski V. Cochrane vertebroplasty review misrepresented evidence for vertebroplasty with early intervention in severely affected patients. BMJ Evid Based Med 2019.
Manchikanti L, Helm S 2nd, Benyamin RM, Hirsch JA. A critical analysis of Obamacare: affordable care or insurance for many and coverage for few? Pain Physician. 2017;20:111–38.
Bauchner H, Fontanarosa PB. The future of US health care policy. JAMA. 2016;315:1339–40.
Cannon MF. Is Obamacare harming quality? (part 1). Health Affairs Blog 4, 2018. https://www.healthaffairs.org/do/10.1377/hblog20180103.261091/full/. Accessed 3 Feb 2019.
Obama B. United States health care reform: progress to date and next steps. JAMA. 2016;316:525–32.
Manchikanti L, Helm S II, Calodney AK, Hirsch JA. Merit-based incentive payment system: meaningful changes in the final rule brings cautious optimism. Pain Physician. 2017;20:E1–E12.
Manchikanti L, Benyamin RM, Falco FJE, Hirsch JA. Recommendations of the Medicare payment advisory commission (MedPAC) on the health care delivery system: the impact of interventional pain management in 2014 and beyond. Pain Physician. 2013;16:419–40.
Manchikanti L, Pampati V, Benyamin RM, Hirsch JA. Cost calculation methodology exacerbates site-of-service differentials by 10- to 18-fold for soft tissue and joint injections in hospital outpatient departments. IPM Reports. 2017;1:183–9.
Manchikanti L, Soin A, Mann DP, Bakshi S, Pampati V, Hirsch JA. Reversal of growth of utilization of interventional techniques in managing chronic pain in Medicare population post Affordable Care Act. Pain Physician. 2017;20:551–67.
Manchikanti L, Soin A, Mann DP, Bakshi S, Pampati V, Hirsch JA. Utilization patterns of facet joint interventions in managing spinal pain: a retrospective cohort study in the U.S. fee-for-service Medicare population. Curr Pain Headache Rep 2019; in press.
Manchikanti L, Soin A, Mann DP, Bakshi S, Pampati V, Hirsch JA. Comparative analysis of utilization of epidural procedures in managing chronic pain in the Medicare population: pre and post Affordable Care Act. Spine (Phila Pa 1976). 2019;44:220–32.
Manchikanti MV, Manchikanti L, Kaye AD, Pampati V, Hirsch JA. Usage patterns of sacroiliac joint injections - a comparative evaluation of pre and post Affordable Care Act in Medicare population. IPM Reports. 2018;2:157–66.
Manchikanti L, Pampati V, Benyamin RM, Hirsch JA. Declining utilization of percutaneous epidural adhesiolysis in Medicare population: evidence-based or over-regulated? IPM Reports. 2018;2:9–18.
Hartman M, Martin AB, Espinosa N, Catlin A. National health care spending in 2016: spending and enrollment growth slow after initial coverage expansions. Health Aff (Millwood). 2018;37:150–60.
Dieleman JL, Baral R, Birger M, Bui AL, Bulchis A, Chapin A, et al. US spending on personal health care and public health, 1996-2013. JAMA. 2016;316:2627–46.
Manchikanti L, Kaye AM, Knezevic NN, McAnally H, Trescot AM, Blank S, et al. Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2017;20(2S):S3–S92.
• Manchikanti L, Sanapati J, Benyamin RM, Atluri S, Kaye AD, Hirsch JA. Reframing the prevention strategies of the opioid crisis: Focusing on prescription opioids, fentanyl, and heroin epidemic. Pain Physician. 2018;21:309–26. A manuscript of critical importance showing the influence of opioid crisis on national care and interventions in the United States.
Kaye AD, Jones MR, Kaye AM, Ripoll JG, Jones DE, Galan V, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 2. Pain Physician. 2017;20:S111–33.
Chakravarthy K, Manchikanti L, Kaye AD, Christo PJ. Reframing the role of neuromodulation therapy in the chronic pain treatment paradigm. Pain Physician. 2018;21:507–13.
National Institute on Drug Abuse. Overdose Death Rates. September 2017. https://www.drugabuse.gov/relatedtopics/trends-statistics/overdose-death-rates
Centers for Medicare and Medicaid Services. www.cms.hhs.gov/home/medicare.Asp. Accessed 3 Feb 2019.
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18:805–35.
International Scientific Institute. Journal Impact Factor List. http://www.scijournal.org
Beall DP, Tutton SM, Murphy K, Olan W, Warner CB, Test JB. Analysis of reporting bias in vertebral augmentation. Pain Physician. 2017;20:E1081–90.
Hirsch JA, Chandra RV. Resurrection of evidence for vertebroplasty? Lancet. 2016;388:1356–7.
Hulme PA, Krebs J, Ferguson SJ, Berlemann U. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine (Phila Pa 1976). 2006;31:1983–2001.
Anderson PA, Froyshteter AB, Tontz WL Jr. Meta-analysis of vertebral augmentation compared with conservative treatment for osteoporotic spinal fractures. J Bone Miner Res. 2013;28:372–82.
Manchikanti L, Boswell MV, Kaye AD, Helm S II, Hirsch JA. Therapeutic role of placebo: evolution of a new paradigm in understanding research and clinical practice. Pain Physician. 2017;20:363–86.
Chou R, Hashimoto R, Friedly J, Fu R, Dana T, Sullivan S, Bougatsos C, Jarvik J. Pain management injection therapies for low back pain. Technology Assessment Report ESIB0813. (Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. HHSA 290–2012-00014-I.) Rockville, MD: Agency for Healthcare Research and Quality; July 10, 2015. https://www.cms.gov/medicare/coverage/determinationprocess/downloads/id98ta.pdf
Manchikanti L, Knezevic NN, Boswell MV, Kaye AD, Hirsch JA. Epidural injections for lumbar radiculopathy and spinal stenosis: a comparative systematic review and meta-analysis. Pain Physician. 2016;19:E365–410.
Boswell MV, Manchikanti L. Appropriate design and methodologic quality assessment, clinically relevant outcomes are essential to determine the role of epidural corticosteroid injections. Commentary RE: Chou R, Hashimoto R, Friedly J, Fu R, Bougatsos C, Dana T, Sullivan SD, Jarvik J. Epidural corticosteroid injections for radiculopathy and spinal stenosis: A systematic review and meta-analysis. Ann Intern Med 2015; 163:373–381. Evid Based Med 2016; 21:89.
Manchikanti L, Benyamin RM, Falco FJE, Caraway DL, Datta S, Hirsch JA. Guidelines warfare over interventional techniques: is there a lack of discourse or straw man? Pain Physician. 2012;15:E1–E26.
Manchikanti L, Benyamin RM, Falco FJ, Kaye AD, Hirsch JA. Do epidural injections provide short- and long-term relief for lumbar disc herniation? A systematic review. Clin Orthop Relat Res. 2015;473:1940–56.
Lee JH, Kim DH, Kim DH, Shin KH, Park SJ, Lee GJ, et al. Comparison of clinical efficacy of epidural injection with or without steroid in lumbosacral disc herniation: a systematic review and meta-analysis. Pain Physician. 2018;21:449–68.
Lee JH, Shin KH, Park SJ, Lee GJ, Lee CH, Kim DH, et al. Comparison of clinical efficacy between transforaminal and interlaminar epidural injections in lumbosacral disc herniation: a systematic review and meta-analysis. Pain Physician. 2018;21:433–48.
Manchikanti L, Nampiaparampil DE, Manchikanti KN, Falco FJE, Singh V, Benyamin RM, et al. Comparison of the efficacy of saline, local anesthetics, and steroids in epidural and facet joint injections for the management of spinal pain: a systematic review of randomized controlled trials. Surg Neurol Int. 2015;6:S194–235.
Shen J, Xu S, Xu S, Ye S, Hao J. Fusion or not for degenerative lumbar spinal stenosis: a meta-analysis and systematic review. Pain Physician. 2018;21:1–8.
Song D, He A, Xu R, Xiu X, Wei Y. Efficacy of pain relief in different postherpetic neuralgia therapies: a network meta-analysis. Pain Physician. 2018;21:19–32.
Manchikanti L, Soin A, Benyamin RM, Singh V, Falco FJ, Calodney AK, et al. An update of the systematic appraisal of the accuracy and utility of discography in chronic spinal pain. Pain Physician. 2018;21:91–110.
Sanapati J, Manchikanti L, Atluri S, Jordan S, Albers SL, Pappolla MA, et al. Do regenerative medicine therapies provide long-term relief in chronic low back pain: a systematic review and metaanalysis. Pain Physician. 2018;21:515–40.
Fu X, Tang L, Wang C, Li M, Wu H, Li J, et al. A network meta-analysis to compare the efficacy of steroid and antiviral medications for facial paralysis from Bell’s palsy. Pain Physician. 2018;21:559–69.
Hou S, Huh B, Kim HK, Kim KH, Abdi S. Treatment of chemotherapy-induced peripheral neuropathy: systematic review and recommendations. Pain Physician. 2018;21:571–92.
Cho JH, Lee JH, Song KS, Hong JY, Joo YS, Lee DH, et al. Treatment outcomes for patients with failed back surgery. Pain Physician. 2017;20:E29–43.
Salazar AP, Stein C, Marchese RR, Plentz RD, Pagnussat AS. Electric stimulation for pain relief in patients with fibromyalgia: a systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2017;20:15–25.
Gupta A, Huettner DP, Dukewich M. Comparative effectiveness review of cooled versus pulsed radiofrequency ablation for the treatment of knee osteoarthritis: a systematic review. Pain Physician. 2017;20:155–71.
Chaichian S, Kabir A, Mehdizadehkashi A, Rahmani K, Moghimi M, Moazzami B. Comparing the efficacy of surgery and medical therapy for pain management in endometriosis: a systematic review and meta-analysis. Pain Physician. 2017;20:185–95.
Gudala K, Bansal D, Vatte R, Ghai B, Schifano F, Boya C. High prevalence of neuropathic pain component in patients with low back pain: evidence from meta-analysis. Pain Physician. 2017;20:343–52.
Helm S 2nd, Simopoulos TT, Stojanovic MP, Abdi S, El Terany MA. Effectiveness of thermal annular procedures in treating discogenic low back pain. Pain Physician. 2017;20:447–70.
Clark J, Nijs J, Yeowell G, Goodwin PC. What are the predictors of altered central pain modulation in chronic musculoskeletal pain populations? A systematic review. Pain Physician. 2017;20:487–500.
Kaye AD, Jones MR, Kaye AM, Ripoll JG, Galan V, Beakley BD, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 1. Pain Physician. 2017;20:S93–S109.
National Academies of Sciences, Engineering, and Medicine. Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. Washington, DC: The National Academies Press; 2017. Available at: https://doi-org.echo.louisville.edu/10.17226/24781
Letter to Marilyn Tavenner, from President and CEO, America’s Health Insurance Plans from National Association of Attorneys General RE Prescription opioid epidemic. September 18, 2017. https://ag.ny.gov/sites/default/files/final_naag_opioid_letter_to_ahip.pdf
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain: United States, 2016. MMWR Recomm Rep. 2016;65:1–49.
Gottlieb S. FDA takes important step to stem the tide of opioid misuse and abuse. FDA Voice, September 28, 2017. https://blogs.fda.gov/fdavoice/index.php/2017/09/fda-takes-important-steps-to-stem-the-tide-of-opioid-misuse-and-abuse/
Dowell D, Noonan RK, Houry D. Underlying factors in drug overdose deaths. JAMA. 2017;318:2295–6.
Draft Report on Pain Management Best Practices: Updates, Gaps, Inconsistencies, and Recommendations. Docket Number: HHS-OS-2018-0027. https://www.hhs.gov/ash/advisory-committees/pain/reports/2018-12-draft-report-on-updates-gaps-inconsistencies-recommendations/index.html. Accessed 3 Feb 2019.
Manchikanti L, Pampati V, Benyamin RM, Hirsch JA. Cost utility analysis of lumbar interlaminar epidural injections in the treatment of lumbar disc herniation, central spinal stenosis, and axial or discogenic low back pain. Pain Physician. 2017;20:219–28.
Manchikanti L, Pampati V, Kaye AD, Hirsch JA. Therapeutic lumbar facet joint nerve blocks in the treatment of chronic low back pain: cost utility analysis based on a randomized controlled trial. Korean J Pain. 2018;31:27–38.
Manchikanti L, Pampati V, Kaye AD, Hirsch JA. Cost utility analysis of cervical therapeutic medial branch blocks in managing chronic neck pain. Int J Med Sci. 2017;14:1307–16.
Lewis R, Williams N, Matar HE, Din N, Fitzsimmons D, Phillips C, et al. The clinical effectiveness and cost effectiveness of management strategies for sciatica: systematic review and economic model. Health Technol Assess. 2011;15:1–578.
Lewis RA, Williams NH, Sutton AJ, Burton K, Din NU, Matar HE, et al. Comparative clinical effectiveness of management strategies for sciatica: systematic review and network meta-analyses. Spine J. 2015;15:1461–77.
Acknowledgments
The authors wish to thank Bert Fellows, MA, Director Emeritus of Psychological Services, for manuscript review, and Tonie M. Hatton and Diane E. Neihoff, transcriptionists, for their assistance in preparation of this manuscript.
Author information
Authors and Affiliations
Ethics declarations
Conflict of Interest
Laxmaiah Manchikanti has provided limited consulting services to Semnur Pharmaceuticals, Incorporated, which is developing nonparticulate steroids. Jaya Sanapati and Vidyasagar Pampati declare no conflict of interest. Alan Kaye is a Section Editor for Current Headache and Pain Reports. He has not been involved in the editorial handling of this manuscript. Dr. Kaye is also a speaker for Merck. Joshua Hirsch is a consultant for Medtronic and on the DMC for Relievent.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Other Pain
Rights and permissions
About this article
Cite this article
Manchikanti, L., Sanapati, J., Pampati, V. et al. Utilization of Vertebral Augmentation Procedures in the USA: a Comparative Analysis in Medicare Fee-for-Service Population Pre- and Post-2009 Trials. Curr Pain Headache Rep 24, 22 (2020). https://doi.org/10.1007/s11916-020-00850-2
Published:
DOI: https://doi.org/10.1007/s11916-020-00850-2