Abstract
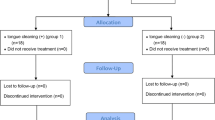
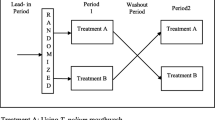
This study was to evaluate the effect of Streptococcus salivarius K12 on tongue coating–associated halitosis. Twenty-eight subjects having tongue coating–associated halitosis were randomly divided into either a test or control group. For each of the 30 days, the test subjects sucked S. salivarius K12 tablet while the control subjects sucked placebo tablets. All the subjects did not take physical (tongue scraping) and chemical (antiseptic mouth-rinse) oral cavity pretreatment prior to use of the tablets. At baseline, and on the 1st, 7th, and 14th day after completing the course of tablets, the subjects were assessed for their organoleptic test (OLT) scores, volatile sulfur compound (VSC) levels, and tongue coating scores (TCS). During the course, all subjects kept their routine oral care habits without scraping their tongue coating. Plaque index, probing depth, and bleeding index were recorded at baseline and at the completion of the trial. On the 1st day following the end of tablet use, the OLT scores and VSC levels had significantly decreased in the test group when compared with the baseline values (P = 0.001 and P = 0.012). The TCS in the test group were also significantly decreased (P = 0.05). At days 7 and 14, the OLT scores in the test group were still significantly lower than the baseline levels (P = 0.006 and P = 0.039 respectively). However, there were no statistical differences with OLT, VSC, and TCS between the test group and the placebo group by analysis of multi-level regression model. The use of S. salivarius K12 did not have significant effect on halitosis with tongue coating cause when the tongue coating was not physically or chemically pre-treated, which implies removing tongue coating is required before Streptococcus salivarius K12 use.

Similar content being viewed by others
References
Yaegaki K, Coil JM (2000) Examination, classification, and treatment of halitosis; clinical perspectives. J Can Dent Assoc 66(5):257–261
Calil CM, Marcondes FK (2006) Influence of anxiety on the production of oral volatile sulfur compounds. Life Sci 79(7):660–664. https://doi.org/10.1016/j.lfs.2006.02.010
Madhushankari GS, Yamunadevi A, Selvamani M, Mohan Kumar KP, Basandi PS (2015) Halitosis - an overview: part-I - classification, etiology, and pathophysiology of halitosis. J Pharm Bioallied Sci 7(Suppl 2):S339–S343. https://doi.org/10.4103/0975-7406.163441
Rosing CK, Loesche W (2011) Halitosis: an overview of epidemiology, etiology and clinical management. Braz Oral Res 25(5):466–471. https://doi.org/10.1590/S1806-83242011000500015
Quirynen M, Dadamio J, Van den Velde S, De Smit M, Dekeyser C, Van Tornout M, Vandekerckhove B (2009) Characteristics of 2000 patients who visited a halitosis clinic. J Clin Periodontol 36(11):970–975. https://doi.org/10.1111/j.1600-051x.2009.01478.x
Yaegaki K, Sanada K (1992) Biochemical and clinical factors influencing oral malodor in periodontal patients. J Periodontol 63(9):783–789. https://doi.org/10.1902/jop.1992.63.9.783
Kazor CE, Mitchell PM, Lee AM, Stokes LN, Loesche WJ, Dewhirst FE, Paster BJ (2003) Diversity of bacterial populations on the tongue dorsa of patients with halitosis and healthy patients. J Clin Microbiol 41(2):558–563. https://doi.org/10.1128/jcm.41.2.558-563.2003
Riggio MP, Lennon A, Rolph HJ, Hodge PJ, Donaldson A, Maxwell AJ, Bagg J (2008) Molecular identification of bacteria on the tongue dorsum of subjects with and without halitosis. Oral Dis 14(3):251–258. https://doi.org/10.1111/j.1601-0825.2007.01371.x
Wang J, Wang M-r, Wang Z-l (2010) Diversity of bacterial population on the tongue dorsa of halitosis patients. Beijing J Stomatol 18(1):25–29
Tonzetich J (1997) Production and origin of oral malodor: a review of mechanisms and methods of analysis. J Periodontol 48(1):13–20. https://doi.org/10.1902/jop.1977.48.1.13
Loesche WJ, Kazor C (2002) Microbiology and treatment of halitosis. Periodontol 2000 28(1):256–279. https://doi.org/10.1034/j.1600-0757.2002.280111.x
Van der Sleen MI, Slot DE, Van Trijffel E, Winkel EG, Van der Weijden GA (2010) Effectiveness of mechanical tongue cleaning on breath odour and tongue coating: a systematic review. Int J Dent Hyg 8(4):258–268. https://doi.org/10.1111/j.1601-5037.2010.00479.x
Wang J, He L (2017) Effect of mechanical self-cleaning of tongue coating on malodor in halitosis patients originating from tongue coating. J Peking Univ (health sciences) 49(2):344–347
Henker J, Schuster F, Nissler K (2001) Successful treatment of gut-caused halitosis with a suspension of living non-pathogenic Escherichia coli bacteria--a case report. Eur J Pediatr 160(10):592–594. https://doi.org/10.1007/s004310100831
Burton JP, Chilcott CN, Moore CJ, Speiser G, Tagg JR (2006) A preliminary study of the effect of probiotic Streptococcus salivarius K12 on oral malodour parameters. J Appl Microbiol 100(4):754–764. https://doi.org/10.1111/j.1365-2672.2006.02837.x
Burton JP, Chilcott CN, Tagg JR (2005) The rationale and potential for the reduction of oral malodour using Streptococcus salivarius probiotics. Oral Dis 11(Suppl 1):29–31. https://doi.org/10.1111/j.1601-0825.2005.01084.x
Masdea L, Kulik EM, Hauser-Gerspach I, Ramseier AM, Filippi A, Waltimo T (2012) Antimicrobial activity of Streptococcus salivarius K12 on bacteria involved in oral malodour. Arch Oral Biol 57(8):1041–1047. https://doi.org/10.1016/j.archoralbio.2012.02.011
Cosseau C, Devine DA, Dullaghan E, Gardy JL, Chikatamarla A, Gellatly S, Yu LL, Pistolic J, Falsafi R, Tagg J, Hancock RE (2008) The commensal Streptococcus salivarius K12 downregulates the innate immune responses of human epithelial cells and promotes host-microbe homeostasis. Infect Immun 76(9):4163–4175. https://doi.org/10.1128/iai.00188-08
Kang MS, Kim BG, Chung J, Lee HC, Oh JS (2006) Inhibitory effect of Weissella cibaria isolates on the production of volatile sulphur compounds. J Clin Periodontol 33(3):226–232. https://doi.org/10.1111/j.1600-051x.2006.00893.x
Suzuki N, Yoneda M, Tanabe K, Fujimoto A, Iha K, Seno K, Yamada K, Iwamoto T, Masuo Y, Hirofuji T (2014) Lactobacillus salivarius WB21-containing tablets for the treatment of oral malodor: a double-blind, randomized, placebo-controlled crossover trial--reply to letter. Oral Surg Oral Med Oral Pathol Oral Radiol 118(4):506. https://doi.org/10.1016/j.oooo.2014.06.014
Shimauchi H, Mayanagi G, Nakaya S, Minamibuchi M, Ito Y, Yamaki K, Hirata H (2008) Improvement of periodontal condition by probiotics with Lactobacillus salivarius WB21: a randomized, double-blind, placebo-controlled study. J Clin Periodontol 35(10):897–905. https://doi.org/10.1111/j.1600-051x.2008.01306.x
Suzuki N, Tanabe K, Takeshita T, Yoneda M, Iwamoto T, Oshiro S, Yamashita Y, Hirofuji T (2012) Effects of oil drops containing Lactobacillus salivarius WB21 on periodontal health and oral microbiota producing volatile sulfur compounds. J Breath Res 6(1):017106. https://doi.org/10.1088/1752-7155/6/1/017106
Kamra S, Pai KM (2014) Lactobacillus salivarius WB21 tablets for the treatment of oral malodor: a commentary. Oral Surg Oral Med Oral Pathol Oral Radiol 118(4):505. https://doi.org/10.1016/j.oooo.2014.06.013
Burton JP, Cowley S, Simon RR, McKinney J, Wescombe PA, Tagg JR (2011) Evaluation of safety and human tolerance of the oral probiotic Streptococcus salivarius K12: a randomized, placebo-controlled, double-blind study. Food Chem Toxicol 49(9):2356–2364. https://doi.org/10.1016/j.fct.2011.06.038
Jamali Z, Aminabadi NA, Samiei M, Sighari Deljavan A, Shokravi M, Shirazi S (2016) Impact of Chlorhexidine pretreatment followed by probiotic Streptococcus salivarius strain K12 on halitosis in children: a randomised controlled clinical trial. Oral Health Prev Dent 14(4):305–313
Rosenberg M, McCulloch CA (1992) Measurement of oral malodor: current methods and future prospects. J Periodontol 63(9):776–782. https://doi.org/10.1902/jop.1992.63.9.776
Oho T, Yoshida Y, Shimazaki Y, Yamashita Y, Koga T (2001) Characteristics of patients complaining of halitosis and the usefulness of gas chromatography for diagnosing halitosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 91(5):531–534. https://doi.org/10.1067/moe.2001.112543
Iwamoto T, Suzuki N, Tanabe K, Takeshita T, Hirofuji T (2010) Effects of probiotic Lactobacillus salivarius WB21 on halitosis and oral health: an open-label pilot trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110(2):201–208. https://doi.org/10.1016/j.tripleo.2010.03.032
Horz HP, Meinelt A, Houben B, Conrads G (2007) Distribution and persistence of probiotic Streptococcus salivarius K12 in the human oral cavity as determined by real-time quantitative polymerase chain reaction. Oral Microbiol Immunol 22(2):126–130. https://doi.org/10.1111/j.1399-302x.2007.00334.x
Miyazaki H, Sakao S, Katoh Y, Takehara T (1995) Correlation between volatile sulphur compounds and certain oral health measurements in the general population. J Periodontol 66(8):679–684. https://doi.org/10.1902/jop.1995.66.8.679
ADA Council on Scientific Affairs (2003) Oral malodor. J Am Dent Assoc 134(2):209–214. https://doi.org/10.14219/jada.archive.2003.0135
Erovic Ademovski S, Lingstrom P, Winkel E, Tangerman A, Persson GR, Renvert S (2012) Comparison of different treatment modalities for oral halitosis. Acta Odontol Scand 70(3):224–233. https://doi.org/10.3109/00016357.2011.635601
Bollen CM, Beikler T (2012) Halitosis: the multidisciplinary approach. Int J Oral Sci 4(2):55–63. https://doi.org/10.1038/ijos.2012.39
Mizuta K, Abiko C, Murata T, Itagaki T, Katsushima N, Akiba T, Sakamoto M, Ootani K, Murayama S (2003) Re-emergence of echovirus type 13 infections in 2002 in Yamagata, Japan. J Inf Secur 47(3):243–247. https://doi.org/10.1016/s0163-4453(03)00081-1
Beecher HK (1955) The powerful placebo. J Am Med Assoc 159(17):1602–1606. https://doi.org/10.1001/jama.1955.02960340022006
Queiroz CS, Hayacibara MF, Tabchoury CP, Marcondes FK, Cury JA (2002) Relationship between stressful situations, salivary flow rate and oral volatile sulfur-containing compounds. Eur J Oral Sci 110(5):337–340. https://doi.org/10.1034/j.1600-0722.2002.21320.x
Wang J, He L, Liu T-t (2012) Study on self-reported halitosis and the associated factors in patients in a periodontal clinic. J Peking Univ (health sciences) 44(2):295–298
Acknowledgments
We thank William McQiu and Prof John Tagg for the correction of grammar and sentence of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lu He and Hongjiang Yang are the co-first authors.
Rights and permissions
About this article
Cite this article
He, L., Yang, H., Chen, Z. et al. The Effect of Streptococcus salivarius K12 on Halitosis: a Double-Blind, Randomized, Placebo-Controlled Trial. Probiotics & Antimicro. Prot. 12, 1321–1329 (2020). https://doi.org/10.1007/s12602-020-09646-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-020-09646-7