Abstract
Objective
The currently available anti-inflammatory drugs often cause diverse side effects with long-term use. Exploring anti-inflammatory drugs with better efficacy and lower toxicity presents an ongoing challenge. Aloperine is an alkaloid extracted from the leaves and seeds of Sophora alopecuroides L. However, the anti-inflammatory effects of Aloperine have not been fully elucidated. This study aimed to investigate whether Aloperine suppresses lipopolysaccharide (LPS)-induced inflammatory responses in RAW264.7 macrophages.
Methods
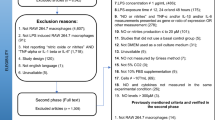
RAW264.7 macrophages were stimulated with LPS (1 μg/mL) in the presence or absence of Aloperine (50 and 100 μM). mRNA expression was measured by real-time PCR, and protein expression was assessed by western blot analysis. The secretion of pro-inflammatory cytokines was measured by ELISA. The levels of nitric oxide (NO) and reactive oxygen species (ROS) were measured by staining. The transcriptional activity of NF-κB was assayed by a luciferase activity assay.
Results
The results proved that Aloperine inhibited the expression of LPS-induced pro-inflammatory cytokines [tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and interleukin-17A (IL-17A)] in macrophages. Treatment with Aloperine inhibited NO production through suppressing inducible nitric oxide synthase (iNOS) expression and the secretion of prostaglandin E2 (PGE2) by inhibiting cyclooxygenase 2 (COX-2) expression. Aloperine prevented LPS-induced oxidative stress by reducing the generation of ROS. Furthermore, aloperine significantly reduced Toll-like receptor 4 (TLR4) and myeloid differentiation factor (Myd-88) levels and prevented the nuclear translocation of nuclear factor-κB (NF-κB) in LPS-treated macrophages.
Conclusion
Taken together, our findings show that Aloperine could suppress LPS-induced macrophage activation by inhibiting the TLR4/Myd-88/NF-κB pathway.









Similar content being viewed by others
References
Gordon S, Taylor P. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005;5:953–64.
Gordon S. Macrophage heterogeneity and tissue lipids. J Clin Invest. 2007;117:89–93.
Sweet MJ, Hume DA. Endotoxin signal transduction in macrophages. J Leukoc Biol. 1996;60:8–26.
Wu C, Zhao W, Zhang X, Chen X. Neocryptotanshinone inhibits lipopolysaccharide-induced inflammation in RAW264.7 macrophages by suppression of NF-κB and iNOS signaling pathways. Acta Pharm Sin B. 2015; 5(4):323–329.
Yang L, Guo H, Li Y, Meng X, Yan L, Zhang D, Wu S, Zhou H, Peng L, Xie Q, et al. Oleoylethanolamide exerts anti-inflammatory effects on LPS-induced THP-1 cells by enhancing PPARα signaling and inhibiting the NF-κB and ERK1/2/AP-1/STAT3 pathways. Sci Rep. 2016;6:34611.
Jeong YH, Oh YC, Cho WK, Yim NH, Ma JY. Anti-inflammatory effect of rhapontici radix ethanol extract via inhibition of NF-κB and MAPK and induction of HO-1 in macrophages. Mediat Inflam. 2016;2016:7216912.
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–10.
Ricciotti E, FitzGerald GA. Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol. 2011;31(5):986–1000.
Shin JS, Hong Y, Lee HH, Ryu B, Cho YW, Kim NJ, Jang DS, Lee KT. Fulgidic Acid isolated from the rhizomes of cyperus rotundus suppresses LPS-Induced iNOS, COX-2, TNF-α, and IL-6 expression by AP-1 inactivation in RAW264.7 macrophages. Biol Pharm Bull. 2015;38(7):1081–1086.
Jiang WY, Jeon BH, Kim YC, Lee SH, Sohn DH, Seo GS. PF2401-SF, standardized fraction of Salvia miltiorrhiza shows anti-inflammatory activity in macrophages and acute arthritis in vivo. Int Immunopharmacol. 2013;16(2):160–164.
Li Fan SY, Zhang SL. Antiviral effect of aloperine. J Zhong Cao Yao. 1998;29:253–4.
Zhou CC, Gao HB, Sun XB, Shi HB, Liu W, Yuan HN, et al. Anti-inflammatory and anti-allergic action of aloperine. Zhongguo Yao Li Xue Bao. 1989;10:360–5.
Ren D, Ma W, Guo B, Wang S. Aloperine attenuates hydrogen peroxide-induced injury via anti-apoptotic activity and suppression of the nuclear factor-κB signaling.
Wu C, Zhao W, Zhang X, Chen X. Neocryptotanshinone inhibits lipopolysaccharide-induced inflammation in RAW264.7 macrophages by suppression of NF-κB and iNOS signaling pathways. Acta Pharm Sin B. 2015; 5(4):323–329.
Dannenberg AJ, Altorki NK, Boyle JO, Dang C, Howe LR, Weksler BB, Subbaramaiah K. Cyclooxygenase 2:a pharmacological target for the prevention for cancer. Lancet Oncol. 2001; 2(9):544.
Watkins DN, Peroni DJ, Lenzo JC, et al. Expression and localization of COX-2 in human airways and cultured airway epithelial cells. Eur Respir J. 1999;13(5):999–1007.
Cao Y, Prescott SM. Many actions of cyclooxyrgenase 2 in cellular dynamics and in cancer. J Cell Physiol. 2002;190(3):279–86.
Totsuka N, Kim YG, Kanemaru K, Niizuma K, Umemoto E, Nagai K, Tahara-Hanaoka S, Nakahasi-Oda C, Honda S, Miyasaka M, et al. Toll-like receptor 4 and MAIR-II/CLM-4/LMIR2 immunoreceptor regulate VLA-4-mediated inflammatory monocyte migration. Nat Commun. 2014;5:4710.
Lucas K, Maes M. Role of the Toll Like receptor (TLR) radical cycle in chronic inflammation: possible treatments targeting the TLR4 pathway. Mol Neurobiol. 2013;48(1):190–204.
Shao J, Li Y, Wang Z, Xiao M, Yin P, Lu Y et al. Novel naphthalimide derivative, exhibited anti-inflammatory effects via targeted- inhibiting TAK1 following down-regulation of ERK1/2- and p38 MAPK-mediated activation of NF-κB in LPS-stimulated RAW264.7 macrophages. Int Immunopharmacol. 2013; 17(2):216–228.
Kumar A, Wu H, Collier-Hyams LS, Hansen JM, Li T, Yamoah K, et al. Commensal bacteria modulate cullin-dependent signaling via generation of reactive oxygen species. EMBO J. 2007;26(21):4457–66.
Lin S, Wu H, Wang C, Xiao Z, Xu F. Regulatory T cells and acute lung injury: cytokines, uncontrolled inflammation, and therapeutic implications. Front Immunol. 2018;9:1545.
Fujiwara Y, Takeya M, Komohara Y. A novel strategy for inducing theantitumor effects of triterpenoid compounds: blocking the protumoralfunctions of tumor-associated macrophages via STAT3 inhibition. Biomed Res Int. 2014;2014:348539.
Lee HT, Kim SK, Kim SH, Kim K, Lim CH, Park J, Roh TY, Kim N, Chai YG. Transcription-related element gene expression pattern differs between microglia and macrophages during inflammation. Inflamm Res. 2014;63(5):389–97.
Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili SA, Mardani F, Seifi B, Mohammadi A, Afshari JT, Sahebkar A. Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol. 2018;233(9):6425–40.
Cen X, Liu S, Cheng K. The role of toll-like receptor in inflammation and tumor immunity. Front Pharmacol. 2018;9:878.
Croce K, Libby P. Intertwining of thrombosis and inflammation in atherosclerosis. Curr Opin Hematol. 2007;14(1):55–61.
Zhang G, Ghosh S. Molecular mechanisms of NF-kappaB activation induced by bacterial lipopolysaccharide through toll-like receptors. J Endotoxin Res. 2000;6(6):453–7.
Zhang J, Wang X, Vikash V, Ye Q, Wu D, Liu Y, Dong W. ROS and ROS-mediated cellular signaling. Oxid Med Cell Longev. 2016;2016:4350965.
Wardyn JD, Ponsford AH, Sanderson CM. Dissecting molecular cross-talk between Nrf2 and NF-κB response pathways. Biochem Soc Trans. 2015;43:621–6.
Wang C, Choi YH, Xian Z, Zheng M, Piao H, Yan G. Aloperine suppresses allergic airway inflammation through NF-κB, MAPK, and Nrf2/HO-1 signaling pathways in mice. Int Immunopharmacol. 2018;65:571–9.
Leon CG, Tory R, Jia J, Sivak O, Wasan KM. Discovery and development of toll-like receptor 4 (TLR4) antagonists: a new paradigm for treating sepsis and other diseases. Pharm Res. 2008;25(8):1751–61.
Acknowledgements
Key research fund of wannan medical college (WK2018ZF05).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None.
Additional information
Responsible Editor: John Di Battista.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ye, Y., Wang, Y., Yang, Y. et al. Aloperine suppresses LPS-induced macrophage activation through inhibiting the TLR4/NF-κB pathway. Inflamm. Res. 69, 375–383 (2020). https://doi.org/10.1007/s00011-019-01313-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-019-01313-0