Abstract
Purpose
The aim of this study was to identify and characterize immune checkpoint inhibitors (ICIs)-associated pituitary adverse events (AEs).
Methods
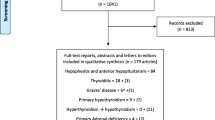
This is a retrospective disproportionality study based on VigiBase, the World Health Organization (WHO) global database of individual case safety reports (ICSRs), with a study period from January 1, 2011 to March 6, 2019. Information component (IC) and reporting odds ratio (ROR) are measures of disproportionate analysis. IC was used to evaluate the association between ICIs and pituitary AEs, while ROR was used to evaluate the differences in reporting of pituitary AEs between different ICI subgroups.
Results
The following ICI-associated pituitary diseases have been increasingly reported: hypophysitis (835 reports; information component 6.74 [95% CI 6.63–6.83]), hypopituitarism (268; 6.12 [95% CI 5.92–6.27]), pituitary enlargement (28; 5.19 [95% CI 4.57–5.63]). The anti-CTLA-4 subgroup had a stronger association with hypophysitis/hypopituitarism than the anti-PD (anti-PD-1 or anti-PD-L1) subgroup (ROR 8.0 [95% CI 6.7–9.6]). Among ICI-associated hypophysitis/hypopituitarism cases, the proportion of male was higher than female (630 [63.9%] vs 356 [36.1%]). Anti-CTLA-4 subgroup and ICI combination (nivolumab plus ipilimumab) subgroup both had a significantly earlier onset time than anti-PD subgroup (67 days [IQR 48–87]; 90 [IQR 34–155]; 140 [IQR 62–218], both p < 0.05). Other endocrinopathies that co-occurred with hypophysitis/hypopituitarism were adrenal insufficiency, thyroid dysfunction, diabetes mellitus and diabetes insipidus. Gastrointestinal disorder was the most common concurrent disease except for endocrinopathies.
Conclusions
ICI-associated pituitary adverse events have significantly increased, and their clinical characteristics should be kept in mind by oncologists and endocrinologists who manage patients treated by immunotherapy.

Similar content being viewed by others
References
Clarke JM, George DJ, Lisi S, Salama AKS (2018) Immune checkpoint blockade: the new frontier in Cancer treatment. Target Oncol 13:1–20. https://doi.org/10.1007/s11523-017-0549-7
Martin-Liberal J, Hierro C, Ochoa de Olza M, Rodon J (2017) Immuno-oncology: the third paradigm in early drug development. Target Oncol 12:125–138. https://doi.org/10.1007/s11523-016-0471-4
Ruggeri RM, Campennì A, Giuffrida G, Trimboli P, Giovanella L, Trimarchi F, Cannavò S (2019) Endocrine and metabolic adverse effects of immune checkpoint inhibitors: an overview (what endocrinologists should know). J Endocrinol Invest 42:745–756. https://doi.org/10.1007/s40618-018-0984-z
Brahmer JR, Lacchetti C, Schneider BJ, Atkins MB, Brassil KJ, Caterino JM, Chau I, Ernstoff MS, Gardner JM, Ginex P et al (2018) Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 36:1714–1768. https://doi.org/10.1200/JCO.2017.77.6385
Byun DJ, Wolchok JD, Rosenberg LM, Girotra M (2017) Cancer immunotherapy: immune checkpoint blockade and associated endocrinopathies. Nat Rev Endocrinol 13:195–207. https://doi.org/10.1038/nrendo.2016.205
Bai X, Chen X, Wu X, Huang Y, Zhuang Y, Lin X (2020) Immune checkpoint inhibitor-associated thyroid dysfunction: a disproportionality analysis using the WHO Adverse Drug Reaction Database, VigiBase. Eur J Endocrinol 182:1–9. https://doi.org/10.1530/EJE-19-0535
Albarel F, Castinetti F, Brue T (2019) MANAGEMENT OF ENDOCRINE DISEASE: Immune check point inhibitors-induced hypophysitis. Eur J Endocrinol 181:R107–R118. https://doi.org/10.1530/EJE-19-0169
Baxi S, Yang A, Gennarelli RL, Khan N, Wang Z, Boyce L, Korenstein D (2018) Immune-related adverse events for anti-PD-1 and anti-PD-L1 drugs: systematic review and meta-analysis. BMJ 360:k793. https://doi.org/10.1136/bmj.k793
Ji HH, Tang XW, Dong Z, Song L, Jia YT (2019) Adverse event profiles of anti-CTLA-4 and anti-PD-1 monoclonal antibodies alone or in combination: analysis of spontaneous reports submitted to FAERS. Clin Drug Investig 39:319–330. https://doi.org/10.1007/s40261-018-0735-0
Zhai Y, Ye X, Hu F, Xu J, Guo X, Zhuang Y, He J (2019) Endocrine toxicity of immune checkpoint inhibitors: a real-world study leveraging US Food and Drug Administration adverse events reporting system. J Immunother Cancer 7:286. https://doi.org/10.1186/s40425-019-0754-2
Raschi E, Mazzarella A, Antonazzo IC, Bendinelli N, Forcesi E, Tuccori M, Moretti U, Poluzzi E, De Ponti F (2019) Toxicities with immune checkpoint inhibitors: emerging priorities from disproportionality analysis of the FDA adverse event reporting system. Target Oncol 14:205–221. https://doi.org/10.1007/s11523-019-00632-w
Lindquist M (2008) VigiBase, the WHO global ICSR database system: basic facts. Drug Inf J 42:409–419. https://doi.org/10.1177/009286150804200501
Bate A, Lindquist M, Edwards IR, Olsson S, Orre R, Lansner A, De Freitas RM (1998) A Bayesian neural network method for adverse drug reaction signal generation. Eur J Clin Pharmacol 54:315–321. https://doi.org/10.1007/s002280050466
Uppsala Monitoring Centre (UMC). Analytical methods developed by the UMC Research team are integrated in VigiLyze. https://www.who-umc.org/vigibase/vigilyze/analytics-in-vigilyze. Accessed 30 Jul 2019
Norén GN, Hopstadius J, Bate A (2013) Shrinkage observed-to-expected ratios for robust and transparent large-scale pattern discovery. Stat Methods Med Res 22:57–69. https://doi.org/10.1177/0962280211403604
OPDIVO® (nivolumab) Prescribing information. Initial US approval: 2014. Revised: 4/2019. https://packageinserts.bms.com/pi/pi_opdivo.pdf. Accessed 17 Jun 2019
KEYTRUDA® (pembrolizumab) Prescribing information. Initial US approval: 2014. Revised: 4/2019. https://www.merck.com/product/usa/pi_circulars/k/keytruda/keytruda_pi.pdf. Accessed 17 Jun 2019
Yervoy® (ipilimumab) Prescribing information. Initial US approval: 2011. Revised: 7/2018. https://packageinserts.bms.com/pi/pi_yervoy.pdf. Accessed 17 Jun 2019
Chang LS, Barroso-Sousa R, Tolaney SM, Hodi FS, Kaiser UB, Min L (2019) Endocrine toxicity of cancer immunotherapy targeting immune checkpoints. Endocr Rev 40:17–65. https://doi.org/10.1210/er.2018-00006
Rastrelli M, Tropea S, Rossi CR, Alaibac M (2014) Melanoma: epidemiology, risk factors, pathogenesis, diagnosis and classification. Vivo 28:1005–1011
Henley SJ, Richards TB, Underwood JM, Eheman CR, Plescia M, McAfee TA (2014) Lung cancer incidence trends among men and women—United States, 2005–2009. MMWR Morb Mortal Wkly Rep 63:1–5
Faje AT, Sullivan R, Lawrence D, Tritos NA, Fadden R, Klibanski A, Nachtigall L (2014) Ipilimumab-induced hypophysitis: a detailed longitudinal analysis in a large cohort of patients with metastatic melanoma. J Clin Endocrinol Metab 99:4078–4085. https://doi.org/10.1210/jc.2014-2306
Min L, Hodi FS, Giobbie-Hurder A, Ott PA, Luke JJ, Donahue H, Davis M, Carroll RS, Kaiser UB (2015) Systemic high-dose corticosteroid treatment does not improve the outcome of ipilimumab-related hypophysitis: a retrospective cohort study. Clin Cancer Res 21:749–755. https://doi.org/10.1158/1078-0432.CCR-14-2353
Caturegli P, Di Dalmazi G, Lombardi M, Grosso F, Larman HB, Larman T, Taverna G, Cosottini M, Lupi I (2016) Hypophysitis secondary to cytotoxic T-lymphocyte-associated protein 4 blockade: insights into pathogenesis from an autopsy series. Am J Pathol 186:3225–3235. https://doi.org/10.1016/j.ajpath.2016.08.020
Scott ES, Long GV, Guminski A, Clifton-Bligh RJ, Menzies AM, Tsang VH (2018) The spectrum, incidence, kinetics and management of endocrinopathies with immune checkpoint inhibitors for metastatic melanoma. Eur J Endocrinol 178:173–180. https://doi.org/10.1530/EJE-17-0810
Mekki A, Dercle L, Lichtenstein P, Marabelle A, Michot JM, Lambotte O, Le Pavec J, De Martin E, Balleyguier C, Champiat S, Ammari S (2018) Detection of immune-related adverse events by medical imaging in patients treated with anti-programmed cell death 1. Eur J Cancer 96:91–104. https://doi.org/10.1016/j.ejca.2018.03.006
Feng Y, Roy A, Masson E, Chen TT, Humphrey R, Weber JS (2013) Exposure-response relationships of the efficacy and safety of ipilimumab in patients with advanced melanoma. Clin Cancer Res 19:3977–3986. https://doi.org/10.1158/1078-0432.CCR-12-3243
Eggermont AM, Chiarion-Sileni V, Grob JJ, Dummer R, Wolchok JD, Schmidt H, Hamid O, Robert C, Ascierto PA, Richards JM et al (2016) Prolonged survival in stage iii melanoma with ipilimumab adjuvant therapy. N Engl J Med 375:1845–1855. https://doi.org/10.1056/NEJMoa1611299
Salem JE, Manouchehri A, Moey M, Lebrun-Vignes B, Bastarache L, Pariente A, Gobert A, Spano JP, Balko JM, Bonaca MP et al (2018) Cardiovascular toxicities associated with immune checkpoint inhibitors: an observational, retrospective, pharmacovigilance study. Lancet Oncol 19:1579–1589. https://doi.org/10.1016/S1470-2045(18)30608-9
Wang DY, Salem JE, Cohen JV, Chandra S, Menzer C, Ye F, Zhao S, Das S, Beckermann KE, Ha L et al (2018) Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and meta-analysis. JAMA Oncol 4:1721–1728. https://doi.org/10.1001/jamaoncol.2018.3923
Iwama S, De Remigis A, Callahan MK, Slovin SF, Wolchok JD, Caturegli P (2014) Pituitary expression of CTLA-4 mediates hypophysitis secondary to administration of CTLA-4 blocking antibody. Sci Transl Med 6:230. https://doi.org/10.1126/scitranslmed.3008002
Barroso-Sousa R, Ott PA, Hodi FS, Kaiser UB, Tolaney SM, Min L (2018) Endocrine dysfunction induced by immune checkpoint inhibitors: practical recommendations for diagnosis and clinical management. Cancer 124:1111–1121. https://doi.org/10.1002/cncr.31200
Lindquist M (2004) Data quality management in pharmacovigilance. Drug Saf 27:857–870. https://doi.org/10.2165/00002018-200427120-00003
Acknowledgements
The supplied data originated from various sources from VigiBase, and the probability that the suspected adverse effect is drug related is not the same in all cases. The information does not represent the opinion of the UMC or the World Health Organization. Camilla Westerberg of the custom search team at the Uppsala Monitoring Centre (Uppsala, Sweden) research department is acknowledged for his help with data extraction.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No competing financial interests exist.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bai, X., Chen, X., Wu, X. et al. Immune checkpoint inhibitor-associated pituitary adverse events: an observational, retrospective, disproportionality study. J Endocrinol Invest 43, 1473–1483 (2020). https://doi.org/10.1007/s40618-020-01226-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01226-4