Abstract
Background
Autism spectrum disorder (ASD) is a neurodevelopmental disorder, and many individuals with ASD have gastrointestinal (GI) comorbidities. Vitamin A (VA) is an essential micronutrient that plays an important role in brain development and GI function.
Methods
A total of 323 children with ASD and 180 control children were enrolled in this study. Symptoms of ASD were assessed with the Child Autism Rating Scale (CARS), the Social Responsiveness Scale (SRS), and the Autism Behavior Checklist (ABC). Caregivers of the children completed questionnaires about GI symptoms. Serum retinol levels were detected with high-performance liquid chromatography (HPLC).
Results
Children with ASD and with GI comorbidity and constipation had considerably lower serum VA levels than autistic children without these symptoms. VA level was associated with CARS, SRS, and ABC scores, whereas GI symptoms were associated some SRS and ABC scores. The interaction of VAD and GI symptoms appeared to aggravate some of the core symptoms of children with ASD.
Conclusions
VAD exacerbates core symptoms in children with ASD, and ASD children with GI comorbidities also have more serious core symptoms than ASD children without GI comorbidities. VAD comorbid with GI symptoms aggravates autistic children’s core symptoms.
Impact
-
VAD exacerbates core symptoms in children with ASD.
-
ASD children with GI comorbidities have more serious core symptoms than ASD children without GI comorbidities.
-
VAD comorbid with GI symptoms aggravates autistic children’s core symptoms.
-
We speculate that VAD might be related to a subtype of ASD that involves GI comorbidities.
-
We believe that our findings will be of fundamental importance to the scientific community.
Similar content being viewed by others
Introduction
Autism spectrum disorder (ASD) is a highly heterogeneous neurodevelopment disorder that is characterized by alterations in social interactions and communication, and restricted and repetitive behavior.1 The prevalence of ASD has been rising in recent years, with an estimated 1 in 59 American children affected by it.2 ASD is one of the most serious problems affecting children’s health worldwide, and it has brought an enormous burden on families and the society.3
The exact etiology or etiologies of ASD are not known. It is generally accepted that genetic and environmental factors contribute to the risk of ASD,3 and the environmental factors appear to include nutrition.4 Several studies have found the nutrition levels of children with ASD differ from those of controls.5,6 Vitamin A deficiency (VAD) is one of the three major micronutrient deficiency diseases in the world, especially in developing countries, and children and pregnant women are at high risk of VAD.7 VA and its active metabolite retinoic acid (RA) play critical roles in the nervous system, including early development of the brain, neuronal proliferation and differentiation, neurite outgrowth, and synaptogenesis.8 The correlation between VA-related substances and ASD has been a topic of interest in recent years. Foreign studies have found that children with ASD have lower retinal dehydrogenase 1 (RALDH1) levels than typically developing (TD) children. RALDH1 catalyzes the oxidation of retinal to RA.9 Research in China also shows that children with ASD have lower VA levels than control children, and VAD is quite common among children with ASD.6
ASD is often displayed with comorbidities, including attention deficit hyperactivity disorder (ADHD), sleep abnormalities, and gastrointestinal (GI) symptoms,10,11,12 and GI comorbidities are common in children with ASD. The incidence of GI comorbidities in children with ASD is much higher than that in TD children,12 and some scholars have suggested that ASD with GI comorbidities may be a subtype of ASD.13
Studies have shown that VA is associated with neurological diseases14,15 and intestinal flora and GI diseases.16,17 A nutritional survey we conducted of children with ASD indicated these children with ASD had higher rates of VAD and constipation than the control group, and the level of VA was negatively correlated with scores on the Child Autism Rating Scale (CARS).6 However, few studies have examined the relationship among VA nutrition levels, GI comorbidities, and the core symptoms of children with ASD. Therefore, the purpose of the current study was to explore the relationship between VA and GI comorbidities and to evaluate whether the coexistence of VAD and GI comorbidities exacerbate the core symptoms of children with ASD, based on our previous research.6 We were particularly interested in determining whether VAD is related to a subtype of ASD that has GI comorbidities.
Methods
Participants
A total of 323 children with ASD, age 2−7 years (274 boys and 49 girls) were recruited for the study, between July 2018 and June 2019, from six training institutions in Chongqing, China. The diagnoses were made after a series of structured interviews conducted by a psychologist and two developmental pediatricians at the Children’s Hospital of Chongqing Medical University, based on the criteria for Autism Spectrum Disorder defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).1 The exclusion criteria were as follows: a history of other developmental disorders or neurological and psychiatric diseases, such as Rett syndrome, cerebral palsy, chronic seizures; other congenital diseases; a history of infections in the past 3 months; a history of using a vitamin A supplement in the previous 3 months; or being unwilling to participate.
The control group included 180 TD children (142 boys and 38 girls). They were recruited randomly from two common kindergartens and one primary school in the same area as the training institutions, between July 2018 and June 2019. The age and gender of this group were similar to those in the ASD group. None of the children in the control group had any signs of neuropathology or any acute or chronic affective diseases in the past 3 months, and none of these children received a vitamin A supplement during the previous 3 months.
Informed consent was obtained from the parents of all the children. The study’s protocol was approved by the Institutional Ethics Committee of the Children’s Hospital of Chongqing Medical University, and this clinical trial was registered in the Chinese Clinical Trial Registry (ChiCTR) (registration number: ChiCTR-ROC-14005442).
Anthropometric measures
Anthropometric examinations were performed by three anthropometrists from the Department of Child Health Care of Children’s Hospital. Body mass index (BMI) was calculated from height and weight measurements (kg/m2).
Questionnaires
The caregivers of the children with ASD and the TD children completed the questionnaires following the instructions of trained investigators. The questionnaires included general demographic information, medical history, and GI symptoms. The GI-symptom questions about constipation, diarrhea, abdominal pain, flatulence, and nausea and vomiting were based on the Questionnaire on Pediatric Gastrointestinal Symptoms-Rome IV (QPGSRIV).18 As it contains no clear definition of the smell of stool, this study defined it as an abnormal odor, such as the smell of rotten eggs.
Symptoms of ASD were assessed with CARS, Social Responsiveness Scale (SRS), and the Autism Behavior Checklist (ABC). The CARS consists of 15 items that are rated on a 4-point scale. Scores of 30−36 indicate mild-moderate autism, while scores greater than 36 indicate severe autism.19 The SRS scale is a 65-item questionnaire that includes five subscales: social awareness, social cognition, social communication, social motivation, and autistic mannerisms. Each item is scored on a Likert scale ranging from 1 to 4.20 The ABC scale contains 57 items (scored 1−4) related to five areas, including sensory stimuli, sensorial relating, body and object use, language, and social self-help.21 The SRS and ABC scales were completed by the caregivers of ASD children following the instructions of trained investigators. The total scores of the scales and the score of each subscale were calculated.
Laboratory measures
The morning fasting venous blood of all the participants was obtained (2 ml) and immediately (within 2 h) transported to the Children’s Hospital. Blood samples were centrifuged at room temperature for 10 min at 3000 rpm and serum was separated. The serum retinol concentration was estimated via high-performance liquid chromatography (HPLC) based on previously described methods.22 Briefly, 200 μl of serum was deproteinized with an equal volume of dehydrated alcohol. The retinol was extracted from the serum by 1000 μl of hexane. Then, 500 μl of supernatant was extracted and the hexane in it was evaporated with nitrogen gas. The residue was dissolved in a 100 μl mobile phase and injected into a column installed in the HPLC apparatus (DGU-20As, Shimadzu Corporation, Kyoto, Japan). The mobile phase was a methanol−water mixture (97:3). The concentration of retinol was determined by spectrophotometry at 315 nm. All the procedures were performed by the same operator in a dark room without light. Serum retinol concentrations of <0.7 , 0.7–1.05, and >1.05 μmol/l were defined, respectively, as VA deficiency (VAD), marginal VA deficiency (MVAD), and VA normal (VAN).
Statistical analyses
The sample size was calculated based on previous studies related to VA in Chinese children.6,23 The standard deviation of VA concentration we used was 0.23 µmol/l and the allowable error was 0.07 µmol/l. With the statistical power set at 0.8, and a type I error rate of 0.05 for a two-sided test, a minimum of 170 participants for each group would be required. We recruited >170 participants for each group in our study.
The Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) version 17 was used for data analysis. The Kolmogorov−Smirnov goodness-of-fit test was used to test the distribution of each dataset for normality before analysis. Continuous variables are described as the mean ± SD, and categorical variables were described as frequencies and percentages. Differences between groups were assessed using a two-tailed Student’s t test, the chi-square test, or Fisher’s exact test. ANCOVA was used to analyze the interaction between VA level and GI symptoms on SRS, ABC and CARS scores, adjusting for gender and age. A Bonferroni post-hoc analysis was conducted to adjust for multiple comparisons.
Results
Socio-demographic characteristics
This study enrolled 323 children with ASD (274 boys and 49 girls) and 180 TD children (142 boys and 38 girls) as the control group. The children with ASD were 4.72 ± 1.33 years old, and the TD children were 4.74 ± 0.93 years old. There was no difference in the age distribution or the gender ratio between the two groups. As shown in Table 1, the weight and height of the children with ASD were significantly lower than those of the control group, while BMI was similar in the two groups. These results indicate that the physical status of the ASD children was lower than that of the control group.
Serum concentrations of retinol
The retinol concentration in the serum of the children with ASD was significantly lower than that of children in the control group (P < 0.01) (Fig. 1a). The males and females in the ASD group had similar serum retinol levels (Fig. 1b), indicating that gender did not affect the serum retinol of children with ASD. The children in the ASD group were classified as mild-moderate ASD (30–36) and severe ASD (37–60), based on the CARS score.19 Patients with severe ASD had lower serum retinol levels than those with mild-moderate ASD (P < 0.01) (Fig. 1c), indicating that children with severe ASD had a more serious VA deficiency.
GI symptoms of the ASD and control groups
As shown in Table 2, 156 (48.3%) of the children in the ASD group reported at least one type of GI symptom, whereas 36 (20.0%) children in the control group reported a GI symptom. The analysis showed that the rate of GI symptoms in the ASD group was significantly greater than that in the control group (P < 0.01). The children in the ASD group had significantly higher rates of constipation, diarrhea, abdominal pain, nausea/vomiting, and stool odor, compared to the children in the control group (all Ps < 0.05). The most common GI symptoms in the ASD group were constipation (n = 105, 32.5%) and stool odor (n = 49, 15.2%). Moreover, 62 (19.2%) of the children with ASD had at least two GI symptoms. The most frequent combination of symptoms in the ASD group was constipation and stool odor (n = 29, 9.0%).
Serum VA levels of the autistic children with and without different GI symptoms
We compared VA levels of the autistic children with and without different GI symptoms. As shown in Table 3, autistic children with GI symptoms had significantly lower serum VA levels than autistic children without GI symptoms (P < 0.01). The VA level in autistic children with constipation was also considerably lower than it was in the autistic children without constipation (P < 0.01). There were no significant differences in VA levels between autistic children with and without other GI symptoms. This suggests that VA level is closely associated with GI symptoms in autistic children, especially those with constipation.
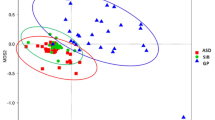
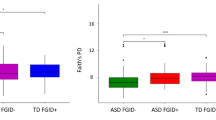
Association of VA level and GI comorbidities on SRS, ABC and CARS scores in children with ASD
The children with ASD were divided into a VA normal without GI symptoms group (VAN + non-GI), a VA deficiency without GI symptoms group (VAD + non-GI), a VA normal with GI symptoms group (VAN + GI), and a VA deficiency with GI symptoms group (VAD + GI) based on serum VA levels and GI symptoms. As shown in Table 4, the ANCOVA found no interaction effect between VA level and GI comorbidity on social awareness, social cognition, social communication, or social motivation, but VA level was significantly associated with social awareness, social cognition, and social communication (all Ps < 0.05). The scores on social awareness, social cognition, and social communication in the VAD + GI group were significantly higher compared with those in the VAN + non-GI group (P < 0.008). The analysis found no interaction effect of VA levels and GI symptoms on total SRS score. However, both VA level (P < 0.001) and GI comorbidity (P = 0.029) had a significant association with the total SRS score; both the VAD + GI group and VAD + non-GI group had significantly higher total SRS scores than the VAN + non-GI group (P < 0.008). Our analysis found that there was a significant interaction effect of VA level and GI symptoms on autistic mannerisms (P = 0.011), as well as a main effect of VA level (P < 0.001). The scores for autistic mannerisms in the VAD + GI group were significantly higher than those in the VAD + non-GI, VAN + GI, and VAN + non-GI groups (P < 0.008). These results suggest that VA level has an effect on the total SRS score and all the SRS subscales, except social motivation. GI comorbidity was associated with autistic mannerisms and the total SRS score. Moreover, the comorbidity of VA deficiency and GI symptoms appears to aggravate autistic mannerisms in children with ASD.
We also analyzed the association of VA level and GI comorbidity with ABC scores. As shown in Table 4, the analysis found no interaction effect between VA level and GI comorbidity on sensory stimuli, sensorial relating, or language in children with ASD, but VA level was associated with sensory stimuli and sensorial relating. There were significant interaction effects of VA level and GI comorbidity on body and object use, social self-help, and total ABC score (all Ps < 0.05), and a main effect of VA level on body and object use, social self-help, and the total ABC score (all Ps < 0.001). The scores for body and object use, social self-help, and the total ABC score of the VAD + GI group were all higher than those scores of the VAD + non-GI, VAN + GI, and VAN + non-GI groups (all Ps < 0.008). These results suggest that VA level affects the total score and all the subscales scores of the ABC, except language, while GI comorbidity has an effect on body and object use and the total ABC score. In addition, the comorbidity of VAD and GI symptoms appears to aggravate body and object use, social self-help, and the total ABC score.
Furthermore, the ANCOVA found no interaction effect between VA level and GI symptoms, but VA level was associated with CARS scores (P < 0.001). The CARS score of the VAD + GI group was significantly higher than that of the VAN + non-GI group (P < 0.008).
Discussion
The incidence of ASD has been increasing in recent years. The clinical manifestations of ASD vary greatly and ASD cannot currently be explained by a single etiology. Thus, ASD should be studied through subtypes with similar clinical features. As many children with ASD have GI comorbidities12 and VA plays an important role in brain development and GI function,8,17 this study focused on the associations among VA level, GI symptoms, and the core symptoms of children with ASD.
The anthropometric index is a key indicator of a child’s nutritional status. Our study showed that the weight and height of children with ASD were significantly lower than those of the children in the control group. This result indicates that the children with ASD may have malnutrition. The results are similar to those of some previous studies. For example, a study by Mari-Bauset et al.24 found that the height of children with ASD was lower than that of controls, and that more children with ASD were under-weight.
VA is an essential micronutrient that plays an important role in the development and function of the brain.14,15 Our analysis of the VA levels of children with ASD showed that autistic children had significantly lower serum VA levels than TD children had. Although males and females of children with ASD showed similar serum retinol levels, patients with severe ASD had lower serum retinol levels than those with mild-moderate ASD, suggesting that VA level is associated with the severity of ASD. The association of VA or its derivatives and ASD has recently received attention from other research teams, and their results have also demonstrated that VA was related to ASD and the severity of ASD.23,25 A study by Xu et al.26 in 2017 demonstrated that reduced RA signaling is an underlying mechanism in the ASD phenotypes linked to ubiquitin protein ligase E3A (UBE3A) hyperactivity. Megson27 thinks that autism may be linked to a disruption of the G-alpha protein, which affects retinoid receptors in the brain. However, some studies have yielded different results. Hyman’s28 study in America found that only children with ASD who were 4−8 years of age had a lower VA intake, whereas specific age groups had an excessive VA intake. This might be related to the dietary habits of different regions and the high food selectivity of some ASD children.
The present study also showed that the incidence of GI symptoms in children with ASD was significantly higher than that of TD children, consistent with findings reported in other studies.12,29 Various studies have found that the GI symptoms that are mainly comorbid in children with ASD are diarrhea, constipation, abdominal pain, nausea or vomiting, and flatulence. Our survey not only included these symptoms, but also investigated the incidence of stool odor, as some parents of autistic children have reported their child’s stool has an abnormal odor. Our results showed that children in the ASD group had higher rates of constipation, diarrhea, abdominal pain, nausea/vomiting, and stool odor than the rates of children in the control group. The most common GI symptom in the ASD group was constipation, followed by stool odor. Some studies also indicate that constipation is the most common GI symptom in children with ASD.12,29 However, there is no consensus on the mechanism of GI symptoms in children with ASD.
A series of studies have demonstrated that VA is associated with GI function. VA can control lymphoid tissues within the small intestines,30 VAD impairs physical barrier functions,31 VA supplementation helps relieve diarrhea and improves intestinal damage.32 However, to the best of our knowledge, there are few studies of the relationship between VA and GI symptoms in children with ASD.
The current study found that autistic children with total GI symptoms had significantly lower serum VA levels than autistic children without GI symptoms, and the VA levels of children with ASD who had constipation were considerably lower than those of children without constipation. The results demonstrated that VA level is closely associated with the incidence of GI symptoms in autistic children, particularly constipation. However, the specific mechanism has not yet been studied. Some studies have shown that VA and its derivatives can affect the development of the enteric nervous system (ENS);33,34 thus, we speculate that VAD may be related to autistic children’s GI comorbidities by affecting their ENS. Moreover, this survey and our previous research6 have shown that VA is associated with the symptoms of ASD and intestinal flora in children with ASD,16 which may be potential causes of the relationship between VA and the GI comorbidity of autistic children.
We further analyzed the association of VA level and GI symptoms on CARS, SRS, and ABC scores in children with ASD. The data showed that VAD was associated with higher scores on the CARS, SRS, and ABC. The results suggest that VAD exacerbates the core symptoms in children with ASD. These results may be related to oxytocin, and CD38 mediates oxytocin release in the brain.35 In addition, all-trans RA is a potent inducer of CD38 expression.36 Our previous study illustrated that gestational VAD might be a risk factor for autistic-like behaviors by suppressing CD38 expression in the hypothalamus of offspring through the Retinoic Acid Receptor Beta (RARβ) signal pathway.37 Nevertheless, GI comorbidity increased autistic mannerisms and the total SRS score, as well as body and object use and the total ABC score. This indicates that children with ASD who have GI comorbidities also have more serious core symptoms. Chaidez et al.’s38 study demonstrated that children with ASD who have frequent GI symptoms scored worse on irritability, social withdrawal, stereotypy, and hyperactivity compared to children with ASD who did not have frequent GI symptoms. Marler et al.39 found in 2017 that functional constipation was associated with parent ratings on the repetitive behavior scales—the revised compulsive, ritualistic, and sameness subscales. It may be that children with ASD have difficulty expressing discomfort or pain due to their communication disorders, so they show increased repetitive stereotypes. Buie et al. surmised in 2010 that a GI symptom is a factor that increases this behavior. Sudden and unexplained behavioral change can be the hallmark of underlying pain or discomfort.40 Moreover, our study also suggests that VAD with comorbid GI symptoms can aggravate autistic children’s core symptoms. This is a new discovery, but its underlying mechanism needs to be studied further. We speculate that VAD might be related to a subtype of ASD that has GI comorbidities.
Of course, the present study has some limitations. First, there is no standardized and valid approach to assessing GI symptoms in ASD. Our questionnaire for GI symptoms was based on the Questionnaire on Pediatric GI Symptoms-Rome IV, and the severity of GI symptoms was not scored, so a correlation analysis between VA and GI symptoms was not performed. Second, ASD children generally have communication problems, and the clinical features of their GI symptoms may differ from those of TD children. Behaviors, such as self-injury, aggression, putting pressure on the abdomen, and other unusual behaviors may be an indication of GI distress. Hence, GI symptoms are difficult to assess accurately by questionnaires and the GI symptoms of autistic children might be underestimated. Finally, this is a cross-sectional study, so it cannot determine which is the cause and which is the result of the associations among ASD, GI symptoms, and VAD.
Conclusion
The serum VA level of children with ASD is lower than that of TD children. The VA level of children with severe autism is lower compared to that of children with mild-moderate autism. The rate of GI symptoms in children with ASD is much higher than that in TD children. The VA level of autistic children with total GI symptoms or constipation is lower than that of the autistic children without these symptoms. The VA nutritional level of autistic children is independently associated with CARS, SRS, and ABC scores. GI symptoms are associated with autistic mannerisms and the total score of the SRS, and body and object use and the total score of the ABC. Moreover, coexistence of VAD and GI symptoms apparently aggravates autistic mannerisms on the SRS, and body and object use, social self-help, and total score of the ABC of children with ASD. VAD exacerbates core symptoms in children with ASD, and ASD children with comorbid GI symptoms also have more serious core symptoms than ASD children without GI comorbidity. In addition, VAD coexist with GI comorbidity apparently aggravates the core symptoms of children with autism. VAD might be related to a subtype of ASD with GI comorbidities. Future animal experiments and prospective clinical studies should be conducted to investigate the mechanism of VA regulating GI symptoms and core symptoms in ASD.
References
Association AP. Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (American Psychiatric Pub, 2013).
Center for Disease Control and Prevention. Data and statistics. http://www.cdc.gov/ncbddd/autism/data.html (2018).
Lord, C., Elsabbagh, M., Baird, G. & Veenstra-Vanderweele, J. Autism spectrum disorder. Lancet 392, 508–520 (2018).
Fujiwara, Takeo, Morisaki, Naho, Honda, Yukiko, Sampei, Makiko & Tani, Yukako Chemicals, nutrition, and autism spectrum disorder: a mini-review. Front. Neurosci. 10, 174 (2016).
Sharp William, G. et al. Dietary intake, nutrient status, and growth parameters in children with autism spectrum disorder and severe food selectivity: an electronic medical record review. J. Acad. Nutr. Diet. 118, 1943–1950 (2018).
Liu, X. et al. Correlation between nutrition and symptoms: nutritional survey of children with autism spectrum disorder in Chongqing, China. Nutrients 8, 294 (2016).
WHO. in WHO Global Database on Vitamin A Deficiency (World Health Organization, 2009).
Maden, M. Retinoic acid in the development, regeneration and maintenance of the nervous system. Nat. Rev. Neurosci. 8, 755–765 (2007).
Pavăl, D. et al. Low retinal dehydrogenase 1 (RALDH1) level in prepubertal boys with autism spectrum disorder: a possible link to dopamine dysfunction. Clin. Psychopharmacol. Neurosci. 15, 229–236 (2017).
Gargaro, B. A. et al. Attentional mechanisms in autism, ADHD, and autism-ADHD using a local-global paradigm. J. Atten. Disord. 22, 1320–1332 (2018).
Cohen, S., Conduit, R., Lockley, S. W., Rajaratnam, S. M. & Cornish, K. M. The relationship between sleep and behavior in autism spectrum disorder (ASD): a review. J. Neurodev. Disord. 6, 44 (2014).
McElhanon, B. O., McCracken, C., Karpen, S. & Sharp, W. G. Gastrointestinal symptoms in autism spectrum disorder: a meta-analysis. Pediatrics 133, 872–883 (2014).
Brown, A. et al. Possible gastrointestinal symptoms in a subset of children with autism. Expert Rev. Gastroenterol. Hepatol. 4, 125–127 (2010).
Zeng, J. et al. Marginal vitamin A deficiency facilitates Alzheimer’s pathogenesis. Acta Neuropathol. 133, 967–982 (2017).
Takeda, A. et al. Vitamin A and carotenoids and the risk of Parkinson’s disease: a systematic review and meta-analysis. Neuroepidemiology 42, 25–38 (2014).
Liu, J. et al. Effect of vitamin A supplementation on gut microbiota in children with autism spectrum disorders—a pilot study. BMC Microbiol. 17, 204 (2017).
Thornton, K. A., Mora-Plazas, M., Marín, C. & Villamor, E. Vitamin A deficiency is associated with gastrointestinal and respiratory morbidity in school-age children. J. Nutr. 144, 496–503 (2014).
Rasquin, A. et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology 130, 1527–1537 (2006).
Zhang, Q. B., Jiang, L. F., Kong, L. Y. & Lu, Y. J. Serum brain-derived neurotrophic factor levels in Chinese children with autism spectrum disorders: a pilot study. Int. J. Dev. Neurosci. 37, 65–68 (2014).
Cen, C. Q. et al. Investigating the validation of the Chinese Mandarin version of the social responsiveness scale in a mainland China child population. BMC Psychiatry 17, 51 (2017).
Santos, T. H. et al. Comparing the use of the Childhood Autism Rating Scale and the Autism Behavior Checklist protocols to identify and characterize autistic individuals. J. Soc. Bras. Fonoaudiol. 24, 104–106 (2012).
Liu, X. et al. Vitamin A supplementation in early life enhances the intestinal immune response of rats with gestational vitamin A deficiency by increasing the number of immune cells. PLoS ONE 9, e114934 (2014).
Sun, C. et al. Nutritional status survey of children with autism and typically developing children aged 4-6 years in Heilongjiang Province, China. J. Nutr. Sci. 2, e16 (2013).
Marí-Bauset, S., Llopis-González, A., Zazpe-García, I., Marí-Sanchis, A. & Morales-Suárez-Varela, M. Nutritional status of children with autism spectrum disorders (ASDs): a case-control study. J. Autism Dev. Disord. 45, 203–212 (2015).
Zhou, W. & Li, S. Decreased levels of serum retinoic acid in chinese children with autism spectrum disorder. Psychiatry Res. 269, 469–473 (2018).
Xu, X. et al. Excessive UBE3A dosage impairs retinoic acid signaling and synaptic plasticity in autism spectrum disorders. Cell Res. 28, 48–68 (2018).
Megson, M. N. Is autism a G-alpha protein defect reversible with natural vitamin A? Med. Hypotheses 54, 979–83.53 (2000).
Hyman, S. L. et al. Nutrient intake from food in children with autism. Pediatrics 130, S145−S153 (2012).
Fulceri, F. et al. Gastrointestinal symptoms and behavioral problems in preschoolers with Autism Spectrum Disorder. Dig. Liver Dis. 48, 248–254 (2016).
Goverse, G. et al. Vitamin A controls the presence of RORγ+ innate lymphoid cells and lymphoid tissue in the small intestine. J. Immunol. 196, 5148–5155 (2016).
Jiang, W. D. et al. Vitamin A deficiency impairs intestinal physical barrier function of fish. Fish. Shellfish Immunol. 87, 546–558 (2019).
Xiao, L. et al. Vitamin A supplementation improves the intestinal mucosal barrier and facilitates the expression of tight junction proteins in rats with diarrhea. Nutrition 57, 97–108 (2019).
Uribe Rosa, A., Hong, S. S. & Bronner, M. E. Retinoic acid temporally orchestrates colonization of the gut by vagal neural crest cells. Dev. Biol. 433, 17–32 (2018).
Nandor, Nagy & Goldstein Allan, M. Enteric nervous system development: a crest cell’s journey from neural tube to colon. Semin. Cell Dev. Biol. 66, 94–106 (2017).
Higashida Haruhiro et al. Cyclic ADP-ribose as a universal calcium signal molecule in the nervous system. Neurochem. Int. 51, 192–199 (2007).
Kishimoto, H. et al. Molecular mechanism of human CD38 gene expression by retinoic acid. Identification of retinoic acid response element in the first intron. J. Biol. Chem. 273, 15429–15434 (1998).
Lai, X. et al. Vitamin A deficiency induces autistic-like behaviors in rats by regulating the RARβ-CD38-oxytocin axis in the hypothalamus. Mol. Nutr. Food Res. 62, 1700754 (2018).
Chaidez, V., Hansen, R. L. & Hertzpicciotto, I. Gastrointestinal problems in children with autism, developmental delays or typical development. J. Autism Developmental Disord. 44, 1117 (2014).
Marler, S. et al. Association of rigid-compulsive behavior with functional constipation in autism spectrum disorder. J. Autism Dev. Disord. 47, 1673–1681 (2017).
Buie, T. et al. Evaluation, diagnosis, and treatment of gastrointestinal disorders in individuals with ASDs: a consensus report. Pediatrics 125, S1−S18 (2010).
Acknowledgements
This study was supported by a grant from the National Natural Science Foundation of China (Nos. 81771223, 81770526), Guangdong Key Project (2018B030335001), and the People’s Livelihood projects in Chongqing Science and Technology Commission (cstc2018jscx-msybX0106).
Author information
Authors and Affiliations
Contributions
T.L. conceived and designed the study. B.C. performed the data acquisition, interpretation, and drafted and revised the manuscript. J.Z., T.Y., M.G., X.L., Q.L. and J.C. assisted with the data acquisition and analyses. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Informed consent was obtained from the parents of all the children.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheng, B., Zhu, J., Yang, T. et al. Vitamin A deficiency increases the risk of gastrointestinal comorbidity and exacerbates core symptoms in children with autism spectrum disorder. Pediatr Res 89, 211–216 (2021). https://doi.org/10.1038/s41390-020-0865-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0865-y
This article is cited by
-
The association of vitamin A, zinc and copper levels with clinical symptoms in children with autism spectrum disorders in Jilin Province, China
BMC Pediatrics (2023)
-
Autism Spectrum Disorder: Signaling Pathways and Prospective Therapeutic Targets
Cellular and Molecular Neurobiology (2021)