Abstract
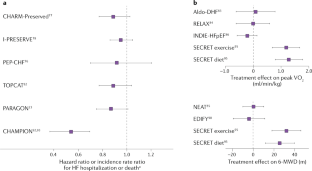
Heart failure with preserved ejection fraction (HFpEF) has grown to become the dominant form of heart failure worldwide, in tandem with ageing of the general population and the increasing prevalences of obesity, diabetes mellitus and hypertension. The clinical syndrome of HFpEF is heterogeneous and must be distinguished from heart failure with reduced ejection fraction as well as other aetiologies that have different treatment strategies. The diagnosis of HFpEF is challenging and ultimately relates to the conceptual definition of heart failure as a clinical syndrome characterized by symptoms that are associated with a reduced capacity of the heart to pump blood adequately at normal filling pressures during diastole. Clinical trials to date have been largely unsuccessful in identifying effective treatments for HFpEF but evidence supports the use of diuretics, mineralocorticoid antagonists and lifestyle interventions. Pathophysiological heterogeneity in the presentation of HFpEF is substantial, and ongoing studies are underway to evaluate the optimal methods to classify patients into phenotypically homogeneous subpopulations to facilitate better individualization of treatment.
Key points
-
Heart failure with preserved ejection fraction (HFpEF) has become the most common form of heart failure, associated with substantial morbidity and mortality.
-
HFpEF is defined haemodynamically as a clinical syndrome associated with a lack of capacity of the heart to pump blood adequately without the requirement for elevated cardiac filling pressures.
-
Typical HFpEF must be distinguished from other causes of the clinical syndrome of heart failure, which are treated differently.
-
Diagnosis is challenging and requires the demonstration of objective evidence of congestion or poor cardiac output using assessment of clinical history, physical examination, natriuretic peptide testing, echocardiography data and invasive exercise testing.
-
To date, most clinical trials on the efficacy of treatments for HFpEF have produced neutral results, but strong evidence supports the use of diuretics, mineralocorticoid receptor antagonists and exercise training as effective therapies.
-
Ongoing studies are evaluating the utility of more rigorous pathophysiological characterization of HFpEF into distinct phenotypes to improve the matching of individualized treatments to patients who are most likely to respond favourably.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Pfeffer, M. A., Shah, A. M. & Borlaug, B. A. Heart failure with preserved ejection fraction in perspective. Circ. Res. 124, 1598–1617 (2019).
Shah, A. M. et al. Heart failure stages among older adults in the community: the Atherosclerosis Risk in Communities Study. Circulation 135, 224–240 (2017).
Dunlay, S. M., Roger, V. L. & Redfield, M. M. Epidemiology of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 14, 591–602 (2017).
Sidney, S. et al. Association between aging of the US population and heart disease mortality from 2011 to 2017. JAMA Cardiol. 4, 1280–1286 (2019).
Flegal, K. M., Kruszon-Moran, D., Carroll, M. D., Fryar, C. D. & Ogden, C. L. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 315, 2284–2291 (2016).
Borlaug, B. A. & Redfield, M. M. Diastolic and systolic heart failure are distinct phenotypes within the heart failure spectrum. Circulation 123, 2006–2013 (2011).
Lupon, J. et al. Heart failure with preserved ejection fraction infrequently evolves toward a reduced phenotype in long-term survivors. Circ. Heart Fail. 12, e005652 (2019).
Pandey, A. et al. Physical activity, fitness, and obesity in heart failure with preserved ejection fraction. JACC Heart Fail. 6, 975–982 (2018).
Borlaug, B. A., Nishimura, R. A., Sorajja, P., Lam, C. S. & Redfield, M. M. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ. Heart Fail. 3, 588–595 (2010).
Obokata, M. et al. Role of diastolic stress testing in the evaluation for heart failure with preserved ejection fraction: a simultaneous invasive-echocardiographic study. Circulation 135, 825–838 (2017).
Reddy, Y. N. V., Carter, R. E., Obokata, M., Redfield, M. M. & Borlaug, B. A. A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation 138, 861–870 (2018).
Pieske, B. et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur. Heart J. 40, 3297–3317 (2019).
Shah, S. J. et al. Phenotype-specific treatment of heart failure with preserved ejection fraction: a multiorgan roadmap. Circulation 134, 73–90 (2016).
Klainer, L. M., Gibson, T. C. & White, K. L. The epidemiology of cardiac failure. J. Chronic Dis. 18, 797–814 (1965).
McKee, P. A., Castelli, W. P., McNamara, P. M. & Kannel, W. B. The natural history of congestive heart failure: the Framingham study. N. Engl. J. Med. 285, 1441–1446 (1971).
Ho, J. E. et al. Differential clinical profiles, exercise responses and outcomes associated with existing HFpEF definitions. Circulation 140, 353–365 (2019).
Abudiab, M. M. et al. Cardiac output response to exercise in relation to metabolic demand in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 15, 776–785 (2013).
Denolin, H., Kuhn, H., Krayenbuehl, H. P., Loogen, F. & Reale, A. The definition of heart failure. Eur. Heart J. 4, 445–448 (1983).
Ponikowski, P. et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 37, 2129–2200 (2016).
Lund, L. H. et al. Heart failure with mid-range ejection fraction in CHARM: characteristics, outcomes and effect of candesartan across the entire ejection fraction spectrum. Eur. J. Heart Fail. 20, 1230–1239 (2018).
Solomon, S. D. et al. Influence of ejection fraction on outcomes and efficacy of spironolactone in patients with heart failure and preserved ejection fraction. Eur. Heart J. 37, 455–462 (2016).
Butler, J., Anker, S. D. & Packer, M. Redefining heart failure with a reduced ejection fraction. JAMA 322, 1761–1762 (2019).
Solomon, S. D. et al. Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N. Engl. J. Med. 381, 1609–1620 (2019).
Yancy, C. W. et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Failure Society of America. Circulation 136, e137–e161 (2017).
Obokata, M. et al. Myocardial injury and cardiac reserve in patients with heart failure and preserved ejection fraction. J. Am. Coll. Cardiol. 72, 29–40 (2018).
Borlaug, B. A. et al. Global cardiovascular reserve dysfunction in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 56, 845–854 (2010).
Borlaug, B. A., Kane, G. C., Melenovsky, V. & Olson, T. P. Abnormal right ventricular-pulmonary artery coupling with exercise in heart failure with preserved ejection fraction. Eur. Heart J. 37, 3293–3302 (2016).
Reddy, Y. N. V. et al. The haemodynamic basis of lung congestion during exercise in heart failure with preserved ejection fraction. Eur Heart J. 40, 3721–3730 (2019).
Obokata, M. et al. Hemodynamics, dyspnea, and pulmonary reserve in heart failure with preserved ejection fraction. Eur. Heart J. 39, 2810–2821 (2018).
Reddy, Y. N. V., Olson, T. P., Obokata, M., Melenovsky, V. & Borlaug, B. A. Hemodynamic correlates and diagnostic role of cardiopulmonary exercise testing in heart failure with preserved ejection fraction. JACC Heart Fail. 6, 665–675 (2018).
Eisman, A. S. et al. Pulmonary capillary wedge pressure patterns during exercise predict exercise capacity and incident heart failure. Circ. Heart Fail. 11, e004750 (2018).
Dorfs, S. et al. Pulmonary capillary wedge pressure during exercise and long-term mortality in patients with suspected heart failure with preserved ejection fraction. Eur. Heart J. 35, 3103–3112 (2014).
Paulus, W. J. & Tschope, C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J. Am. Coll. Cardiol. 62, 263–271 (2013).
Luscher, T. F. Lumpers and splitters: the bumpy road to precision medicine. Eur. Heart J. 40, 3292–3296 (2019).
Hwang, S. J., Melenovsky, V. & Borlaug, B. A. Implications of coronary artery disease in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 63, 2817–2827 (2014).
Eleid, M. F., Nishimura, R. A., Sorajja, P. & Borlaug, B. A. Systemic hypertension in low-gradient severe aortic stenosis with preserved ejection fraction. Circulation 128, 1349–1353 (2013).
Tamargo, M. et al. Functional mitral regurgitation and left atrial myopathy in heart failure with preserved ejection fraction. Eur. J. Heart Fail. https://doi.org/10.1002/ejhf.1699 (2020).
Obokata, M., Reddy, Y. N. V. & Borlaug, B. A. Diastolic dysfunction and heart failure with preserved ejection fraction: understanding mechanisms by using noninvasive methods. JACC Cardiovasc. Imaging 13, 245–257 (2019).
Davie, A. P., Francis, C. M., Caruana, L., Sutherland, G. R. & McMurray, J. J. Assessing diagnosis in heart failure: which features are any use? QJM 90, 335–339 (1997).
Mentz, R. J., Broderick, S., Shaw, L. K., Fiuzat, M. & O’Connor, C. M. Heart failure with preserved ejection fraction: comparison of patients with and without angina pectoris (from the Duke Databank for Cardiovascular Disease). J. Am. Coll. Cardiol. 63, 251–258 (2014).
Shah, S. J. et al. Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur. Heart J. 39, 3439–3450 (2018).
Yang, J. H. et al. Endothelium dependent and independent coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Eur. J. Heart Fail. https://doi.org/10.1002/ejhf.1671 (2020).
Mohammed, S. F. et al. Coronary microvascular rarefaction and myocardial fibrosis in heart failure with preserved ejection fraction. Circulation 131, 550–559 (2015).
Gorter, T. M. et al. Right heart dysfunction and failure in heart failure with preserved ejection fraction: mechanisms and management. Position statement on behalf of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 20, 16–37 (2018).
Reddy, Y. N. V., Obokata, M., Gersh, B. J. & Borlaug, B. A. High prevalence of occult heart failure with preserved ejection fraction among patients with atrial fibrillation and dyspnea. Circulation 137, 534–535 (2018).
Obokata, M., Reddy, Y. N., Pislaru, S. V., Melenovsky, V. & Borlaug, B. A. Evidence supporting the existence of a distinct obese phenotype of heart failure with preserved ejection fraction. Circulation 136, 6–19 (2017).
Drazner, M. H. et al. The relationship of right- and left-sided filling pressures in patients with heart failure and a preserved ejection fraction. Circ. Heart Fail. 3, 202–206 (2010).
From, A. M. et al. Bedside assessment of cardiac hemodynamics: the impact of noninvasive testing and examiner experience. Am. J. Med. 124, 1051–1057 (2011).
Stevenson, L. W. & Perloff, J. K. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA 261, 884–888 (1989).
Lam, C. S. et al. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J. Am. Coll. Cardiol. 53, 1119–1126 (2009).
Iwanaga, Y. et al. B-type natriuretic peptide strongly reflects diastolic wall stress in patients with chronic heart failure: comparison between systolic and diastolic heart failure. J. Am. Coll. Cardiol. 47, 742–748 (2006).
Mueller, C. et al. Heart failure association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eur. J. Heart Fail. 21, 715–731 (2019).
Cleland, J. G., Taylor, J. & Tendera, M. Prognosis in heart failure with a normal ejection fraction. N. Engl. J. Med. 357, 829–830 (2007).
van Veldhuisen, D. J. et al. B-type natriuretic peptide and prognosis in heart failure patients with preserved and reduced ejection fraction. J. Am. Coll. Cardiol. 61, 1498–1506 (2013).
Anjan, V. Y. et al. Prevalence, clinical phenotype, and outcomes associated with normal B-type natriuretic peptide levels in heart failure with preserved ejection fraction. Am. J. Cardiol. 110, 870–876 (2012).
Wang, T. J. et al. Impact of obesity on plasma natriuretic peptide levels. Circulation 109, 594–600 (2004).
Andersen, M. J. & Borlaug, B. A. Invasive hemodynamic characterization of heart failure with preserved ejection fraction. Heart Fail. Clin. 10, 435–444 (2014).
Borlaug, B. A. et al. Diastolic relaxation and compliance reserve during dynamic exercise in heart failure with preserved ejection fraction. Heart 97, 964–969 (2011).
Andersen, M. J., Olson, T. P., Melenovsky, V., Kane, G. C. & Borlaug, B. A. Differential hemodynamic effects of exercise and volume expansion in people with and without heart failure. Circ. Heart Fail. 8, 41–48 (2015).
Maron, B. A., Cockrill, B. A., Waxman, A. B. & Systrom, D. M. The invasive cardiopulmonary exercise test. Circulation 127, 1157–1164 (2013).
Maeder, M. T., Thompson, B. R., Brunner-La Rocca, H. P. & Kaye, D. M. Hemodynamic basis of exercise limitation in patients with heart failure and normal ejection fraction. J. Am. Coll. Cardiol. 56, 855–863 (2010).
Fujimoto, N. et al. Hemodynamic responses to rapid saline loading: the impact of age, sex, and heart failure. Circulation 127, 55–62 (2013).
Guazzi, M. et al. 2016 Focused update: clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation 133, e694–e711 (2016).
Lancellotti, P. et al. The clinical use of stress echocardiography in non-ischaemic heart disease: recommendations from the European association of cardiovascular imaging and the american society of echocardiography. Eur. Heart J. Cardiovasc. Imaging 17, 1191–1229 (2016).
Holland, D. J., Prasad, S. B. & Marwick, T. H. Contribution of exercise echocardiography to the diagnosis of heart failure with preserved ejection fraction (HFpEF). Heart 96, 1024–1028 (2010).
Burgess, M. I., Jenkins, C., Sharman, J. E. & Marwick, T. H. Diastolic stress echocardiography: hemodynamic validation and clinical significance of estimation of ventricular filling pressure with exercise. J. Am. Coll. Cardiol. 47, 1891–1900 (2006).
Talreja, D. R., Nishimura, R. A. & Oh, J. K. Estimation of left ventricular filling pressure with exercise by Doppler echocardiography in patients with normal systolic function: a simultaneous echocardiographic-cardiac catheterization study. J. Am. Soc. Echocardiogr. 20, 477–479 (2007).
Obokata, M. & Borlaug, B. A. The strengths and limitations of E/e’ in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 20, 1312–1314 (2018).
Nauta, J. F. et al. Correlation with invasive left ventricular filling pressures and prognostic relevance of the echocardiographic diastolic parameters used in the 2016 ESC heart failure guidelines and in the 2016 ASE/EACVI recommendations: a systematic review in patients with heart failure with preserved ejection fraction. Eur. J. Heart Fail. 20, 1303–1311 (2018).
Santos, M. et al. E/e’ ratio in patients with unexplained dyspnea: lack of accuracy in estimating left ventricular filling pressure. Circ. Heart Fail. 8, 749–756 (2015).
Sharifov, O. F. & Gupta, H. What is the evidence that the tissue doppler index E/e’ reflects left ventricular filling pressure changes after exercise or pharmacological intervention for evaluating diastolic function? A systematic review. J. Am. Heart Assoc. 6, e004766 (2017).
Paulus, W. J. H2FPEF score. Circulation 138, 871–873 (2018).
Segar, M. W., Patel, K. V., Berry, J. D., Grodin, J. L. & Pandey, A. Generalizability and implications of the H2FPEF score in a cohort of patients with heart failure with preserved ejection fraction. Circulation 139, 1851–1853 (2019).
Myhre, P. L. et al. Application of the H2 FPEF score to a global clinical trial of patients with heart failure with preserved ejection fraction: the TOPCAT trial. Eur. J. Heart Fail. 21, 1288–1291 (2019).
Sepehrvand, N. et al. External validation of the H2F-PEF model in diagnosing patients with heart failure and preserved ejection fraction. Circulation 139, 2377–2379 (2019).
Cleland, J. G. et al. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur. Heart J. 27, 2338–2345 (2006).
Yusuf, S. et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-preserved trial. Lancet 362, 777–781 (2003).
Massie, B. M. et al. Irbesartan in patients with heart failure and preserved ejection fraction. N. Engl. J. Med. 359, 2456–2467 (2008).
Solomon, S. D. et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet 380, 1387–1395 (2012).
Yamamoto, K., Origasa, H. & Hori, M. Effects of carvedilol on heart failure with preserved ejection fraction: the Japanese Diastolic Heart Failure Study (J-DHF). Eur. J. Heart Fail. 15, 110–118 (2013).
Conraads, V. M. et al. Effects of the long-term administration of nebivolol on the clinical symptoms, exercise capacity, and left ventricular function of patients with diastolic dysfunction: results of the ELANDD study. Eur. J. Heart Fail. 14, 219–225 (2012).
Pitt, B. et al. Spironolactone for heart failure with preserved ejection fraction. N. Engl. J. Med. 370, 1383–1392 (2014).
Edelmann, F. et al. Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction: the Aldo-DHF randomized controlled trial. JAMA 309, 781–791 (2013).
Redfield, M. M. et al. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: a randomized clinical trial. JAMA 309, 1268–1277 (2013).
Redfield, M. M. et al. Isosorbide mononitrate in heart failure with preserved ejection fraction. N. Engl. J. Med. 373, 2314–2324 (2015).
Borlaug, B. A. et al. Effect of inorganic nitrite vs placebo on exercise capacity among patients with heart failure with preserved ejection fraction: the INDIE-HFpEF randomized clinical trial. JAMA 320, 1764–1773 (2018).
Pieske, B. et al. Vericiguat in patients with worsening chronic heart failure and preserved ejection fraction: results of the SOluble guanylate Cyclase stimulatoR in heArT failurE patientS with PRESERVED EF (SOCRATES-PRESERVED) study. Eur. Heart J. 38, 1119–1127 (2017).
Filippatos, G. et al. Patient-reported outcomes in the SOluble guanylate Cyclase stimulatoR in heArT failurE patientS with PRESERVED ejection fraction (SOCRATES-PRESERVED) study. Eur. J. Heart Fail. 19, 782–791 (2017).
Ahmed, A. et al. Effects of digoxin on morbidity and mortality in diastolic heart failure: the ancillary digitalis investigation group trial. Circulation 114, 397–403 (2006).
Komajda, M. et al. Effect of ivabradine in patients with heart failure with preserved ejection fraction: the EDIFY randomized placebo-controlled trial. Eur. J. Heart Fail. 19, 1495–1503 (2017).
Shah, S. J. et al. Effect of neladenoson bialanate on exercise capacity among patients with heart failure with preserved ejection fraction: a randomized clinical trial. JAMA 321, 2101–2112 (2019).
Abraham, W. T. et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet 377, 658–666 (2011).
Adamson, P. B. et al. Wireless pulmonary artery pressure monitoring guides management to reduce decompensation in heart failure with preserved ejection fraction. Circ. Heart Fail. 7, 935–944 (2014).
Pandey, A. et al. Exercise training in patients with heart failure and preserved ejection fraction: meta-analysis of randomized control trials. Circ. Heart Fail. 8, 33–40 (2015).
Kitzman, D. W. et al. Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction: a randomized clinical trial. JAMA 315, 36–46 (2016).
Anand, I. S. et al. Interaction between spironolactone and natriuretic peptides in patients with heart failure and preserved ejection fraction: from the TOPCAT trial. JACC Heart Fail. 5, 241–252 (2017).
Pfeffer, M. A. et al. Regional variation in patients and outcomes in the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist (TOPCAT) trial. Circulation 131, 34–42 (2015).
de Denus, S. et al. Spironolactone metabolites in TOPCAT - new insights into regional variation. N. Engl. J. Med. 376, 1690–1692 (2017).
Selvaraj, S. et al. Utility of the cardiovascular physical examination and impact of spironolactone in heart failure with preserved ejection fraction. Circ. Heart Fail. 12, e006125 (2019).
Vaduganathan, M. et al. Prior heart failure hospitalization, clinical outcomes, and response to sacubitril/valsartan compared with valsartan in HFpEF. J. Am. Coll. Cardiol. 75, 245–254 (2020).
Mentz, R. J. et al. Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J. Am. Coll. Cardiol. 64, 2281–2293 (2014).
Schwartzenberg, S. et al. Effects of vasodilation in heart failure with preserved or reduced ejection fraction implications of distinct pathophysiologies on response to therapy. J. Am. Coll. Cardiol. 59, 442–451 (2012).
Tsimploulis, A. et al. Systolic blood pressure and outcomes in patients with heart failure with preserved ejection fraction. JAMA Cardiol. 3, 288–297 (2018).
Alehagen, U., Benson, L., Edner, M., Dahlstrom, U. & Lund, L. H. Association between use of statins and mortality in patients with heart failure and ejection fraction of ≥50. Circ. Heart Fail. 8, 862–870 (2015).
Obokata, M., Reddy, Y. N. V., Melenovsky, V., Pislaru, S. & Borlaug, B. A. Deterioration in right ventricular structure and function over time in patients with heart failure and preserved ejection fraction. Eur. Heart J. 40, 689–697 (2019).
Zakeri, R. et al. Impact of atrial fibrillation on exercise capacity in heart failure with preserved ejection fraction: a RELAX trial ancillary study. Circ. Heart Fail. 7, 123–130 (2014).
Zakeri, R., Chamberlain, A. M., Roger, V. L. & Redfield, M. M. Temporal relationship and prognostic significance of atrial fibrillation in heart failure patients with preserved ejection fraction: a community-based study. Circulation 128, 1085–1093 (2013).
Packer, D. L. et al. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA 321, 1261–1274 (2019).
Packer, M. Effect of catheter ablation on pre-existing abnormalities of left atrial systolic, diastolic, and neurohormonal functions in patients with chronic heart failure and atrial fibrillation. Eur. Heart J. 40, 1873–1879 (2019).
Melenovsky, V. et al. Left atrial remodeling and function in advanced heart failure with preserved or reduced ejection fraction. Circ. Heart Fail. 8, 295–303 (2015).
Freed, B. H. et al. Prognostic utility and clinical significance of cardiac mechanics in heart failure with preserved ejection fraction: importance of left atrial strain. Circ. Cardiovasc. Imaging 9, e003754 (2016).
Reddy, Y. N. V. et al. Left atrial strain and compliance in the diagnostic evaluation of heart failure with preserved ejection fraction. Eur. J. Heart Fail. 21, 891–900 (2019).
Telles, F. et al. Impaired left atrial strain predicts abnormal exercise haemodynamics in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 21, 495–505 (2019).
Kitzman, D. W., Brubaker, P. H., Morgan, T. M., Stewart, K. P. & Little, W. C. Exercise training in older patients with heart failure and preserved ejection fraction: a randomized, controlled, single-blind trial. Circ. Heart Fail. 3, 659–667 (2010).
Edelmann, F. et al. Exercise training improves exercise capacity and diastolic function in patients with heart failure with preserved ejection fraction: results of the Ex-DHF (Exercise training in Diastolic Heart Failure) pilot study. J. Am. Coll. Cardiol. 58, 1780–1791 (2011).
Haykowsky, M. J. et al. Effect of endurance training on the determinants of peak exercise oxygen consumption in elderly patients with stable compensated heart failure and preserved ejection fraction. J. Am. Coll. Cardiol. 60, 120–128 (2012).
Hummel, S. L. et al. Low-sodium DASH diet improves diastolic function and ventricular-arterial coupling in hypertensive heart failure with preserved ejection fraction. Circ. Heart Fail. 6, 1165–1171 (2013).
Reddy, Y. N. V. et al. Characterization of the obese phenotype of heart failure with preserved ejection fraction: a RELAX trial ancillary study. Mayo Clin. Proc. 94, 1199–1209 (2019).
Reddy, Y. N. V. et al. Adverse renal response to decongestion in the obese phenotype of heart failure with preserved ejection fraction. J. Card. Fail. 26, 101–107 (2020).
Miller, W. L. & Borlaug, B. A. Impact of obesity on volume status in patients with ambulatory chronic heart failure. J. Card. Fail. 26, 112–117 (2020).
Reddy, Y. N. V. et al. Quality of life in heart failure with preserved ejection fraction: importance of obesity, functional capacity, and physical inactivity. Eur. J. Heart Fail. https://doi.org/10.1002/ejhf.1788 (2020).
Reddy, Y. N. V. et al. Hemodynamic effects of weight loss in obesity: a systematic review and meta-analysis. JACC Heart Fail. 7, 678–687 (2019).
Zelniker, T. A. et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet 393, 31–39 (2019).
McMurray, J. J. V. et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N. Engl. J. Med. 381, 1995–2008 (2019).
Lam, C. S. P., Chandramouli, C., Ahooja, V. & Verma, S. SGLT-2 inhibitors in heart failure: current management, unmet needs, and therapeutic prospects. J. Am. Heart Assoc. 8, e013389 (2019).
Vaduganathan, M. et al. Sudden death in heart failure with preserved ejection fraction: a competing risks analysis from the TOPCAT trial. JACC Heart Fail. 6, 653–661 (2018).
Borlaug, B. A. et al. Impaired chronotropic and vasodilator reserves limit exercise capacity in patients with heart failure and a preserved ejection fraction. Circulation 114, 2138–2147 (2006).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02145351 (2020).
Hasenfuss, G. et al. A transcatheter intracardiac shunt device for heart failure with preserved ejection fraction (REDUCE LAP-HF): a multicentre, open-label, single-arm, phase 1 trial. Lancet 387, 1298–1304 (2016).
Kaye, D. M. et al. One-year outcomes after transcatheter insertion of an interatrial shunt device for the management of heart failure with preserved ejection fraction. Circ. Heart Fail. 9, e003662 (2016).
Feldman, T. et al. Transcatheter interatrial shunt device for the treatment of heart failure with preserved ejection fraction (REDUCE LAP-HF I [Reduce elevated left atrial pressure in patients with heart failure]): a phase 2, randomized, sham-controlled trial. Circulation 137, 364–375 (2018).
Shah, S. J. et al. One-year safety and clinical outcomes of a transcatheter interatrial shunt device for the treatment of heart failure with preserved ejection fraction in the reduce elevated left atrial pressure in patients with heart failure (REDUCE LAP-HF I) trial: a randomized clinical trial. JAMA Cardiol. 3, 968–977 (2018).
Obokata, M. et al. Effects of interatrial shunt on pulmonary vascular function in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 74, 2539–2550 (2019).
Borlaug, B. A. & Reddy, Y. N. V. The role of the pericardium in heart failure: implications for pathophysiology and treatment. JACC Heart Fail. 7, 574–585 (2019).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03499236 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03088033 (2020).
Borlaug, B. A. et al. Percutaneous pericardial resection: a novel potential treatment for heart failure with preserved ejection fraction. Circ. Heart Fail. 10, e003612 (2017).
Borlaug, B. A. et al. Pericardiotomy enhances left ventricular diastolic reserve with volume loading in humans. Circulation 138, 2295–2297 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03923673 (2020).
Tromp, J. et al. Identifying pathophysiological mechanisms in heart failure with reduced versus preserved ejection fraction. J. Am. Coll. Cardiol. 72, 1081–1090 (2018).
Obokata, M. et al. The neurohormonal basis of pulmonary hypertension in heart failure with preserved ejection fraction. Eur. Heart J. 40, 3707–3717 (2019).
Tromp, J. et al. Novel endotypes in heart failure: effects on guideline-directed medical therapy. Eur. Heart J. 39, 4269–4276 (2018).
Tromp, J. et al. Biomarker profiles in heart failure patients with preserved and reduced ejection fraction. J. Am. Heart Assoc. 6, e003989 (2017).
Sanders-van Wijk, S. et al. Circulating biomarkers of distinct pathophysiological pathways in heart failure with preserved vs. reduced left ventricular ejection fraction. Eur. J. Heart Fail. 17, 1006–1014 (2015).
Tromp, J. et al. Biomarker correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction. Circulation 140, 1359–1361 (2019).
Hoeper, M. M. et al. Pulmonary hypertension in heart failure with preserved ejection fraction: a plea for proper phenotyping and further research. Eur. Heart J. 38, 2869–2873 (2017).
Borlaug, B. A. & Obokata, M. Is it time to recognize a new phenotype? Heart failure with preserved ejection fraction with pulmonary vascular disease. Eur. Heart J. 38, 2874–2878 (2017).
Gorter, T. M., Obokata, M., Reddy, Y. N. V., Melenovsky, V. & Borlaug, B. A. Exercise unmasks distinct pathophysiologic features in heart failure with preserved ejection fraction and pulmonary vascular disease. Eur. Heart J. 39, 2825–2835 (2018).
Borlaug, B. A., Lam, C. S., Roger, V. L., Rodeheffer, R. J. & Redfield, M. M. Contractility and ventricular systolic stiffening in hypertensive heart disease insights into the pathogenesis of heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 54, 410–418 (2009).
Shah, A. M. et al. Prognostic importance of impaired systolic function in heart failure with preserved ejection fraction and the impact of spironolactone. Circulation 132, 402–414 (2015).
Melenovsky, V., Hwang, S. J., Lin, G., Redfield, M. M. & Borlaug, B. A. Right heart dysfunction in heart failure with preserved ejection fraction. Eur. Heart J. 35, 3452–3462 (2014).
Sabbah, M. S. et al. Obese-inflammatory phenotypes in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 73 (Suppl. 1), 661 (2019).
Van Tassell, B. W. et al. IL-1 blockade in patients with heart failure with preserved ejection fraction. Circ. Heart Fail. 11, e005036 (2018).
Houstis, N. E. et al. Exercise intolerance in heart failure with preserved ejection fraction: diagnosing and ranking its causes using personalized O2 pathway analysis. Circulation 137, 148–161 (2018).
Fayyaz, A. U. et al. Global pulmonary vascular remodeling in pulmonary hypertension associated with heart failure and preserved or reduced ejection fraction. Circulation 137, 1796–1810 (2018).
Molina, A. J. et al. Skeletal muscle mitochondrial content, oxidative capacity, and Mfn2 expression are reduced in older patients with heart failure and preserved ejection fraction and are related to exercise intolerance. JACC Heart Fail. 4, 636–645 (2016).
Rommel, K. P. et al. Extracellular volume fraction for characterization of patients with heart failure and preserved ejection fraction. J. Am. Coll. Cardiol. 67, 1815–1825 (2016).
Yap, J. et al. Association of diabetes mellitus on cardiac remodeling, quality of life, and clinical outcomes in heart failure with reduced and preserved ejection fraction. J. Am. Heart Assoc. 8, e013114 (2019).
Shah, S. J. et al. Phenomapping for novel classification of heart failure with preserved ejection fraction. Circulation 131, 269–279 (2015).
Kao, D. P. et al. Characterization of subgroups of heart failure patients with preserved ejection fraction with possible implications for prognosis and treatment response. Eur. J. Heart Fail. 17, 925–935 (2015).
Segar, M. W. et al. Phenomapping of patients with heart failure with preserved ejection fraction using machine learning-based unsupervised cluster analysis. Eur. J. Heart Fail. 22, 148–158 (2020).
Senni, M., Caravita, S. & Paulus, W. J. Do existing definitions identify subgroup phenotypes or reflect the natural history of heart failure with preserved ejection fraction? Circulation 140, 366–369 (2019).
Andersson, C. et al. Risk factor-based subphenotyping of heart failure in the community. PLoS One 14, e0222886 (2019).
Borlaug, B. A., Melenovsky, V. & Koepp, K. E. Inhaled sodium nitrite improves rest and exercise hemodynamics in heart failure with preserved ejection fraction. Circ. Res. 119, 880–886 (2016).
Borlaug, B. A., Koepp, K. E. & Melenovsky, V. Sodium nitrite improves exercise hemodynamics and ventricular performance in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 66, 1672–1682 (2015).
Reddy, Y. N. V. et al. The β-adrenergic agonist albuterol improves pulmonary vascular reserve in heart failure with preserved ejection fraction. Circ. Res. 124, 306–314 (2019).
Maurer, M. S. et al. Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N. Engl. J. Med. 379, 1007–1016 (2018).
Gonzalez-Lopez, E. et al. Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur. Heart J. 36, 2585–2594 (2015).
Mohammed, S. F. et al. Left ventricular amyloid deposition in patients with heart failure and preserved ejection fraction. JACC Heart Fail. 2, 113–122 (2014).
Acknowledgements
The author is supported by grants RO1 HL128526 and UO1 HL125205.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Additional information
Peer review information
Nature Reviews Cardiology thanks A. Desai, M. Metra and W. Paulus for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Borlaug, B.A. Evaluation and management of heart failure with preserved ejection fraction. Nat Rev Cardiol 17, 559–573 (2020). https://doi.org/10.1038/s41569-020-0363-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-020-0363-2
This article is cited by
-
Inhibition of ferroptosis reverses heart failure with preserved ejection fraction in mice
Journal of Translational Medicine (2024)
-
Effect of sacubitril valsartan on heart failure with mid-range or preserved ejection fraction in patients on maintenance hemodialysis: real-world experience in a single-center, prospective study
BMC Cardiovascular Disorders (2024)
-
Targeting HDAC6 to treat heart failure with preserved ejection fraction in mice
Nature Communications (2024)
-
Artificial intelligence-enabled ECG for left ventricular diastolic function and filling pressure
npj Digital Medicine (2024)
-
HFpEF as systemic disease, insight from a diagnostic prediction model reminiscent of systemic inflammation and organ interaction in HFpEF patients
Scientific Reports (2024)



