Abstract
Introduction
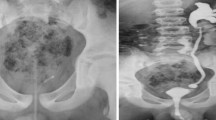
A significant proportion of PUV becomes symptomatic after the perinatal period. Voiding cystourethrography (VCUG) often fails to identify PUVs. This study evaluates the relationship between the radiological appearance of the posterior urethra, potential secondary radiological signs and endoscopically documented PUV in boys with febrile UTIs, VUR, refractory symptoms of bladder overactivity or suggestive sonography findings.
Patients and methods
Data on VCUG findings and endoscopy from 92 boys (mean age 27 months) who underwent endoscopic PUV incision between 2012 and 2017 following a VCUG were reviewed. 24 boys with endoscopically unsuspicious urethras were included as control group (mean age 27.5 months). Statistical analysis was performed using Fisher’s exact test.
Results
In patients with PUV, the urethra was suspicious on a preoperative VCUG in 45.7%, whereas it appeared normal in 54.3%. Abortive forms of PUV were more frequently found in patients with a radiologically unsuspicious urethra (30%vs.16.7%, p = 0.15). Bladder neck hypertrophy on VCUG (16.7%vs.60.9%, OR 7.5, p < 0.001), a trabeculated bladder on VCUG (72%vs.37.5%, OR 4.3, p < 0.001) and a hypertrophied musculus interuretericus (38%vs.4.2%, OR 11.7, p < 0.001) were more common in patients with PUV and urethras appearing normal on VCUG as compared to controls.
Conclusion
Unsuspicious findings of the urethra on VCUG cannot exclude a relevant PUV and implicate a risk of disregarding abortive forms. The presence of secondary radiologic signs of infravesical obstruction on a VCUG despite an unsuspicious posterior urethra in boys with recurrent UTI’s as well as refractory symptoms of bladder overactivity or suggestive signs on sonography must be further clarified endoscopically.




Similar content being viewed by others
References
Schober JM, Dulabon LM, Woodhouse CR (2004) Outcome of valve ablation in late-presenting posterior urethral valves. BJU Int 94:616–619. https://doi.org/10.1111/j.1464-410X.2004.05011.x
Hodges SJ, Patel B, McLorie G, Atala A (2009) Posterior urethral valves. Sci World J 9:1119–1126. https://doi.org/10.1100/tsw.2009.127
Thakkar D, Deshpande AV, Kennedy SE (2014) Epidemiology and demography of recently diagnosed cases of posterior urethral valves. Pediatr Res 76:560–563. https://doi.org/10.1038/pr.2014.134
Agarwal (2001) Urethral valves. BJU Int 84:570–578. https://doi.org/10.1046/j.1464-410x.1999.00307.x
de Jong TPVM, Radmayr C, Dik P et al (2008) Posterior urethral valves: search for a diagnostic reference standard. Urology 72:1022–1025. https://doi.org/10.1016/j.urology.2008.04.037
Stephens FD, Smith ED, Hutson J (2001) Congenital anomalies of the kidney, urinary and genital tracts, 2nd edn. Taylor & Francis, UK, pp 91–117
Young HH, Frontz WA, Baldwin JG (1919) Congenital obstruction of the posterior Urethra1 Read at the meeting of the Association of Genito-Urinary Surgeons at Atlantic City, New Jersey, June 1919. J Urol 3:289–366. https://doi.org/10.1016/S0022-5347(17)74179-1
Nakai H, Hyuga T, Kawai S et al (2017) Aggressive diagnosis and treatment for posterior urethral valve as an etiology for vesicoureteral reflux or urge incontinence in children. Investig Clin Urol 58:S46–S48. https://doi.org/10.4111/icu.2017.58.S1.S46
Nakamura S, Hyuga T, Kawai S et al (2016) The endoscopic morphological features of congenital posterior urethral obstructions in boys with refractory daytime urinary incontinence and nocturnal enuresis. Eur J Pediatr Surg 26:368–375. https://doi.org/10.1055/s-0035-1563401
Pieretti RV (1993) The mild end of the clinical spectrum of posterior urethral valves. J Pediatr Surg 28:701–704. https://doi.org/10.1016/0022-3468(93)90036-k(discussion 704–6)
Bomalaski MD, Anema JG, Coplen DE et al (1999) Delayed presentation of posterior urethral valves: a not so benign condition. J Urol 162:2130–2132. https://doi.org/10.1016/s0022-5347(05)68140-2
de Jong TPVM, Kuijper CF, Chrzan R et al (2013) Efficacy and safety of urethral de-obstruction in boys with overactive bladder complaints. J Pediatr Urol 9:1072–1076. https://doi.org/10.1016/j.jpurol.2013.03.011
Özen MA, Taşdemir M, Gündoğdu G et al (2019) Does voiding cystourethrogram exclude posterior urethral valves in late presenting cases? Eur J Pediatr Surg 29:85–89. https://doi.org/10.1055/s-0038-1672146
Dorschner W, Stolzenburg JU, Dieterich F (1994) A new theory of micturition and urinary continence based on histomorphological studies. 2. The musculus sphincter vesicae: continence or sexual function? Urol Int 52:154–158. https://doi.org/10.1159/000282596
Schwartz GJ, Munoz A, Schneider MF et al (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637. https://doi.org/10.1681/ASN.2008030287
Dewan PA, Zappala SM, Ransley PG, Duffy PG (1992) Endoscopic reappraisal of the morphology of congenital obstruction of the posterior urethra. Br J Urol 70:439–444
Hendren WH (1971) Posterior urethral valves in boys a broad clinical spectrum. J Urol 106:298–307. https://doi.org/10.1016/S0022-5347(17)61278-3
Anema JG, Rozanski TA (1998) Posterior urethral valves presenting as post-ejaculatory dysuria in a 29-year-old physician. J Urol 160:126–127. https://doi.org/10.1016/s0022-5347(01)63056-8
Pulido JE, Furth SL, Zderic SA et al (2014) Renal parenchymal area and risk of ESRD in boys with posterior urethral valves. Clin J Am Soc Nephrol 9:499–505. https://doi.org/10.2215/CJN.08700813
Born M, Spiller L, Bachour H et al (2013) Dose area product of pediatric VCUG with regard to the strongly lowered German diagnostic reference levels. RoFo 185:262–267. https://doi.org/10.1055/s-0032-1325609
Eswara JR, Song JB, Chang AJ et al (2014) Urethrography interpretation skills of urology and radiology residents at tertiary care medical centers. Urology 83:1239–1242. https://doi.org/10.1016/j.urology.2014.02.027
Schaeffer AJ, Sood S, Logvinenko T et al (2014) Variation in the documentation of findings in pediatric voiding cystourethrogram. Pediatr Radiol 44:1548–1556. https://doi.org/10.1007/s00247-014-3028-7
Smeulders N, Makin E, Desai D et al (2011) The predictive value of a repeat micturating cystourethrogram for remnant leaflets after primary endoscopic ablation of posterior urethral valves. J Pediatr Urol 7:203–208. https://doi.org/10.1016/j.jpurol.2010.04.011
Bloom DA, Lebowitz RL, Bauer SB (1997) Correlation of cystographic bladder morphology and neuroanatomy in boys with posterior urethral valves. Pediatr Radiol 27:553–556. https://doi.org/10.1007/s002470050179
Androulakakis PA, Karamanolakis DK, Tsahouridis G et al (2005) Myogenic bladder decompensation in boys with a history of posterior urethral valves is caused by secondary bladder neck obstruction? BJU Int 96:140–143. https://doi.org/10.1111/j.1464-410X.2005.05583.x
Oswald J, Heidegger I, Steiner E et al (2013) Pediatric urology gender-related fetal development of the internal urethral sphincter. Urology 82:1410–1415. https://doi.org/10.1016/j.urology.2013.03.096
Abraham MK, Nasir ARA, Sudarsanan B et al (2009) Role of alpha adrenergic blocker in the management of posterior urethral valves. Pediatr Surg Int 25:1113–1115. https://doi.org/10.1007/s00383-009-2469-9
Kajbafzadeh A-M, Payabvash S, Karimian G (2007) The effects of bladder neck incision on urodynamic abnormalities of children with posterior urethral valves. J Urol 178:2142–2149. https://doi.org/10.1016/j.juro.2007.07.046
Keihani S, Kajbafzadeh A-M, Kameli SM, Abbasioun R (2017) Long-term impacts of concurrent posterior urethral valve ablation and bladder neck incision on urinary continence and ejaculation. Urology 99:278–280. https://doi.org/10.1016/j.urology.2016.09.036
Hennus PML, Hoenjet E, Kieft JH et al (2017) The long-term effect of superficial bladder neck incision on ejaculation and incontinence in boys with primary and secondary bladder neck obstruction. Front Pediatr 5:152. https://doi.org/10.3389/fped.2017.00152
Oswald J, Schwentner C, Lunacek A et al (2006) Reevaluation of the fetal muscle development of the vesical trigone. J Urol 176:1166–1170. https://doi.org/10.1016/j.juro.2006.04.040
Bani Hani O, Prelog K, Smith GHH (2006) A method to assess posterior urethral valve ablation. J Urol 176:303–305. https://doi.org/10.1016/S0022-5347(06)00562-3
Babu R, Hariharasudhan S, Ramesh C (2016) Posterior urethra: anterior urethra ratio in the evaluation of success following PUV ablation. J Pediatr Urol 12:385.e1–385.e5. https://doi.org/10.1016/j.jpurol.2016.04.041
Author information
Authors and Affiliations
Contributions
BH: Protocol development, data collection and management, data analysis, manuscript writing. JT: data collection and analysis, manuscript writing. LL: manuscript editing. TJ: protocol development, manuscript editing. JO: protocol development, manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
The study protocol of this retrospective study is in accordance with the ethical standards of the institutional research committee (Gemeinsame Ethikkommission der Barmherzigen Schwestern + Barmherzige Brüder”, EKS 38/17, approved on 2nd Nov 2017) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Compliant with the journals guidelines and as approved by the institutional ethics committee, there was no need for obtaining informed consent from the included patients/their parents. None of the published endoscopic and radiologic images contain any identifying characteristics.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Haid, B., Thüminger, J., Lusuardi, L. et al. Is there a need for endoscopic evaluation in symptomatic boys with an unsuspicious urethra on VCUG? A consideration of secondary radiologic signs of posterior urethral valves . World J Urol 39, 271–279 (2021). https://doi.org/10.1007/s00345-020-03175-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03175-2