Abstract
Purpose
To summarize the scope of nomenclature and measurement methods used to document endplate defects in the health sciences literature.
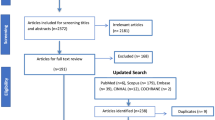
Methods
The scoping review followed the York framework and was reported according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews. The databases of PubMed, Scopus, Embase and CINAHL were searched using key terms. Screening and selection were conducted by two independent reviewers. A standardized, pilot-tested form was used for extracting data, which were analyzed descriptively.
Results
The review included 211 studies, originating from 29 countries, with the USA (18.8%) and China (12.26%) as leading contributors. Thirty-four different terms for structural endplate defects were reported, but were never defined in most studies (65%). Of the 34 different terms used, some appeared to represent the same phenomenon, while the same terms were occasionally defined differently between studies. Schmorl’s nodes were most commonly investigated (n = 99 studies) and defined similarly across studies, with the main difference relating to whether the indentation (node) was required to have a sclerotic margin. There were also similarities in definitions for endplate sclerosis. However, there was great variability in the definitions of other terms, such as lesions, irregularities, abnormalities, erosions and changes.
Conclusion
With the possible exception of Schmorl’s nodes, we lack a common language for effectively communicating structural endplate findings. This review provides a foundation and impetus for standardizing terminology and core measures to improve communication and synthesis of the growing body of endplate research to advance related knowledge.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material (paragraph). Then process the ppt slide as graphical image.


Similar content being viewed by others
References
Brinjikji W, Luetmer PH, Comstock B et al (2015) Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. Am J Neuroradiol 36:811–816. https://doi.org/10.3174/ajnr.A4173
Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian DRJ (1994) Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 331:69–73
Endean A, Palmer KTCD (2011) Potential of magnetic resonance imaging findings to refine case definition for mechanical low back pain in epidemiological studies: a systematic review. Spine (Phila Pa 1976) 36:160–169
DA Moore K (2006) Clinically oriented anatomy, 5th edn. Lippincott Williams & Wilkins, Baltimore
Perry O (1957) Fracture of the vertebral end-plate in the lumbar spine; an experimental biochemical investigation. Acta Orthop Scand Suppl 25:101
Wang Y, Videman T, Battie MC (2013) Morphometrics and lesions of vertebral end plates are associated with lumbar disc degeneration: evidence from cadaveric spines. J Bone Joint Surg Am 95:e26. https://doi.org/10.2106/JBJS.L.00124
Adams M, Dolan P, Luo J et al (2013) Intervertebral disc decompression following endplate damage: implications for disc degeneration depend on spinal level and age. Spine (Phila Pa 1976) 38:1473–1481
Eubanks JD, Lee MJ, Cassinelli EAN (2007) Does lumbar facet arthrosis precede disc degeneration? A postmortem study. Clin Orthop Relat Res 464:184–189
Wang Y, Videman T, Battié MC (2012) ISSLS prize winner: lumbar vertebral endplate lesions: associations with disc degeneration and back pain history. Spine (Phila Pa 1976) 37:1490–1496. https://doi.org/10.1097/BRS.0b013e3182608ac4
Fields AJ, Liebenberg EC, Lotz JC (2014) Innervation of pathologies in the lumbar vertebral end plate and intervertebral disc. Spine J 14:513–521. https://doi.org/10.1016/j.spinee.2013.06.075
Määttä JH, Karppinen JI, Luk KDK et al (2015) Phenotype profiling of Modic changes of the lumbar spine and its association with other MRI phenotypes: a large-scale population-based study. Spine J 15:1933–1942. https://doi.org/10.1016/j.spinee.2015.06.056
Zehra U, Flower L, Robson-Brown K et al (2017) Defects of the vertebral end plate: implications for disc degeneration depend on size. Spine J 17:727–737. https://doi.org/10.1016/j.spinee.2017.01.007
Williams FM, Manek NJSP et al (2007) Schmorl’s nodes: common, highly heritable, and related to lumbar disc disease. Arthritis Rheum 57:855–860
Hamanishi C, Kawabata TYT et al (1994) Schmorl’s nodes on magnetic resonance imaging. Their incidence and clinical relevance. Spine (Phila Pa 1976) 19:450–453
Zehra U, Bow C, Lotz JC et al (2018) Structural vertebral endplate nomenclature and etiology: a study by the ISSLS Spinal Phenotype Focus Group. Eur Spine J 27:2–12. https://doi.org/10.1007/s00586-017-5292-3
Wang Y, Videman T, Battié MC (2012) Lumbar vertebral endplate lesions: prevalence, classification, and association with age. Spine (Phila Pa 1976) 37:1432–1439. https://doi.org/10.1097/BRS.0b013e31824dd20a
Arksey H, O’Malley L (2005) Scoping studies : towards a methodological framework. Int J Soc Res Methodol 8:19–32. https://doi.org/10.1080/1364557032000119616
Dar G, Peleg S, Masharawi Y et al (2009) Demographical aspects of Schmorl nodes. Spine (Phila Pa 1976) 34:E312–E315. https://doi.org/10.1097/brs.0b013e3181995fc5
Hansson T, Roos B (1983) The amount of bone mineral and Schmorl’s nodes in lumbar vertebrae. Spine (Phila Pa 1976) 8:266–271
Lin CY, Chen HY, Ding HJ et al (2012) Evaluation of Schmorl’s nodes using F-18 FDG PET/CT. Clin Radiol 67:e17–e21. https://doi.org/10.1016/j.crad.2012.04.006
Stabler A, Weiss M, Gartner C et al (1997) MR imaging intraosseous (Schmorl’s nodes). Am J Roentgenol 168:933–938
Abbas J, Slon V, Stein D et al (2017) In the quest for degenerative lumbar spinal stenosis etiology: the Schmorl’s nodes model. BMC Musculoskelet Disord 18:1–7. https://doi.org/10.1186/s12891-017-1512-6
Yoo HJ, Hong SH, Kim DH et al (2017) Measurement of fat content in vertebral marrow using a modified dixon sequence to differentiate benign from malignant processes. J Magn Reson Imaging 45:1534–1544. https://doi.org/10.1002/jmri.25496
Grivé E, Rovira A, Capellades J et al (1999) Radiologic findings in two cases of acute Schmorl’s nodes. Am J Neuroradiol 20:1717–1721
Donescu OS, Battie MC, Videman T (2007) The influence of magnetic resonance imaging findings of degenerative disease on dual-energy X-ray absorptiometry measurements in middle-aged men. Acta Radiol 48:193–199. https://doi.org/10.1080/02841850601129015
Al Kaissi A, Klaushofer K, Grill F (2007) Progressive vertebral fusion in a girl with spinal enchondromatosis. Eur J Radiol Extra 63:125–129. https://doi.org/10.1016/j.ejrex.2007.06.004
Lee SW, Mathie AG, Jackson JE, Hughes SP (2001) Investigation of vertebral “end plate sclerosis”. Skeletal Radiol 30:454–459. https://doi.org/10.1007/s0025610300454
Zigler JE, Glenn J, Delamarter RB (2012) Five-year adjacent-level degenerative changes in patients with single-level disease treated using lumbar total disc replacement with ProDisc-L versus circumferential fusion. J Neurosurg Spine 17:504–511. https://doi.org/10.3171/2012.9.SPINE11717
Pfirrman CWA, Resnick D (2001) Schmorl’s nodes of the thoracic and lumbar spine: radiographic-pathologic study of prevalence, characterization, and correlation with degenerative changes of 1650 spinal levels in 100 cadavers. Radiology 219:368–374
Brayda-Bruno M, Albano D, Cannella G et al (2018) Endplate lesions in the lumbar spine: a novel MRI-based classification scheme and epidemiology in low back pain patients. Eur Spine J 27:2854–2861. https://doi.org/10.1007/s00586-018-5787-6
Choi W, Song S, Chae S, Ko S (2017) Comparison of the extent of degeneration among the normal disc, immobilized disc, and immobilized disc with an endplate fracture. CiOS Clin Orthop Surg 9:193–199. https://doi.org/10.4055/cios.2017.9.2.193
Feng Z, Liu Y, Yang G et al (2018) Lumbar vertebral endplate defects on magnetic resonance images. Spine (Phila Pa 1976) 43:919–927. https://doi.org/10.1097/brs.0000000000002450
Berg-Johansen B, Jain D, Liebenberg EC et al (2018) Tidemark avulsions are a predominant form of endplate irregularity. Spine (Phila Pa 1976) 43:1095–1101. https://doi.org/10.1097/BRS.0000000000002545
Østergaard M, Maksymowych WP, Pedersen SJ et al (2009) Structural lesions detected by magnetic resonance imaging in the spine of patients with spondyloarthritis—definitions, assessment system, and reference image set. J Rheumatol 36:18–34. https://doi.org/10.3899/jrheum.090617
Boysen JC, Silverman SL (2012) Chiropractic management of a patient with Scheuermann’s kyphosis. Clin Chiropr 15:5–9. https://doi.org/10.1016/j.clch.2012.01.005
Chen JX, Xu DL, Sheng SR et al (2016) Risk factors of kyphosis recurrence after implant removal in thoracolumbar burst fractures following posterior short-segment fixation. Int Orthop 40:1253–1260. https://doi.org/10.1007/s00264-016-3180-9
Joe E, Lee JW, Park KW et al (2015) Herniation of cartilaginous endplates in the lumbar spine: MRI findings. AJR Am J Roentgenol 204:1075–1081. https://doi.org/10.2214/AJR.14.13319
Armbrecht G, Felsenberg D, Ganswindt M et al (2015) Vertebral Scheuermann’s disease in Europe: prevalence, geographic variation and radiological correlates in men and women aged 50 and over. Osteoporos Int 26:2509–2519. https://doi.org/10.1007/s00198-015-3170-6
Sharma A, Parsons M, Pilgram T (2011) Temporal interactions of degenerative changes in individual components of the lumbar intervertebral discs. Spine (Phila Pa 1976) 36:1794–1800. https://doi.org/10.1097/brs.0b013e31821590ad
Chanchairujira K, Chung CB, Kim JY, Papakonstantinou O, Lee MH, Clopton PRD (2004) Intervertebral disk calcification of the spine in an elderly population: radiographic prevalence, location, and distribution and correlation with spinal degeneration. Radiology 230:499–503
Arana E, Royuela A, Kovacs FM et al (2010) Lumbar spine: agreement in the interpretation of 1.5-T MR images by using the Nordic Modic Consensus Group classification form. Radiology 254:809–817. https://doi.org/10.1148/radiol.09090706/-/DC1
Jensen TS, Sorensen JS, Kjaer P (2007) Intra- and interobserver reproducibility of vertebral endplate signal (modic) changes in the lumbar spine: the nordic modic consensus group classification. Acta Radiol 48:748–754. https://doi.org/10.1080/02841850701422112
Niinimäki J, Korkiakoski A, Parviainen O et al (2009) Association of lumbar artery narrowing, degenerative changes in disc and endplate and apparent diffusion in disc on postcontrast enhancement of lumbar intervertebral disc. Magn Reson Mater Phys Biol Med 22:101–109. https://doi.org/10.1007/s10334-008-0151-1
Toiviainen-Salo S, Markula-Patjas K, Kerttula L et al (2012) The thoracic and lumbar spine in severe juvenile idiopathic arthritis: magnetic resonance imaging analysis in 50 children. J Pediatr 160:140–146. https://doi.org/10.1016/j.jpeds.2011.06.030
Weiner BK, Vilendecic M, Ledic D et al (2015) Endplate changes following discectomy: natural history and associations between imaging and clinical data. Eur Spine J 24:2449–2457. https://doi.org/10.1007/s00586-014-3734-8
Higashino K, Sairyo K, Katoh S et al (2012) Long-term outcomes of lumbar posterior apophyseal. J Bone Joint Surg Am 74:1–7
Uraoka H, Higashino K, Morimoto M et al (2018) Study of lesions of the lumbar endplate based on the stage of maturation of the lumbar vertebral body: the relationship between skeletal maturity and chronological age. Eur J Orthop Surg Traumatol 28:183–187. https://doi.org/10.1007/s00590-017-2032-7
Hilton RC, Ball J, Benn RT (1976) Vertebral end-plate lesions (Schmorl’ s nodes) in the dorsolumbar spine. Ann Rheum Dis 35:127–132
Abu-Ghanem S, Ohana N, Abu-Ghanem Y et al (2013) Acute schmorl node in dorsal spine: an unusual cause of a sudden onset of severe back pain in a young female. Asian Spine J 7:131–135. https://doi.org/10.4184/asj.2013.7.2.131
Li Y, Samartzis D, Campbell DD et al (2016) Two subtypes of intervertebral disc degeneration distinguished by large-scale population-based study. Spine J 16:1079–1089. https://doi.org/10.1016/j.spinee.2016.04.020
Sanginov AJ, Krutko AV, Baykov ES, Lutsik AA (2018) Outcomes of surgical treatment of lumbar disk herniation using an annular closure device. Coluna/Columna 17:188–194. https://doi.org/10.1590/S1808-185120181703193832
Boyle JJW, Singer KP, Milne N (1998) Pattern of intervertebral disc degeneration in the cervicothoracic junctional region. Man Ther 3:72–77. https://doi.org/10.1016/S1356-689X(98)80021-0
Daniels DJ, Luo TD, Puffer R et al (2015) Degenerative changes in adolescent spines: a comparison of motocross racers and age-matched controls. J Neurosurg Pediatr 15:266–271. https://doi.org/10.3171/2014.9.peds14153
Rajab A, Kunze J, Mundlos S (2004) Spondyloepiphyseal dysplasia omani type: a new recessive type of SED with progressive spinal involvement. Am J Med Genet 126A:413–419. https://doi.org/10.1002/ajmg.a.20606
Rose PS, Ahn NU, Levy HP et al (2001) Thoracolumbar spinal abnormalities in Stickler syndrome. Spine (Phila Pa 1976) 26:403–409
Kanna RM, Shetty AP, Rajasekaran S (2014) Patterns of lumbar disc degeneration are different in degenerative disc disease and disc prolapse magnetic resonance imaging analysis of 224 patients. Spine J 14:300–307. https://doi.org/10.1016/j.spinee.2013.10.042
Määttä JH, Rade M, Freidin MB et al (2018) Strong association between vertebral endplate defect and Modic change in the general population. Sci Rep 8:1–8. https://doi.org/10.1038/s41598-018-34933-3
Munir S, Freidin MB, Rade M et al (2018) Endplate defect is heritable, associated with low back pain and triggers intervertebral disc degeneration: a longitudinal study from TwinsUK. Spine (Phila Pa 1976) 43:1496–1501. https://doi.org/10.1097/BRS.0000000000002721
Rajasekaran S, Kanna RM, Senthil N et al (2013) Phenotype variations affect genetic association studies of degenerative disc disease: conclusions of analysis of genetic association of 58 single nucleotide polymorphisms with highly specific phenotypes for disc degeneration in 332 subjects. Spine J 13:1309–1320. https://doi.org/10.1016/j.spinee.2013.05.019
Farshad-Amacker NA, Hughes A, Herzog RJ et al (2017) The intervertebral disc, the endplates and the vertebral bone marrow as a unit in the process of degeneration. Eur Radiol 27:2507–2520. https://doi.org/10.1007/s00330-016-4584-z
Rade M, Määttä JH, Freidin MB et al (2018) Vertebral endplate defect as initiating factor in intervertebral disc degeneration; strong association between endplate defect and disc degeneration in the general population. Spine (Phila Pa 1976) 43:412–419. https://doi.org/10.1097/brs.0000000000002352
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med 22(3):276–282
Zehra U, Cheung JPY, Bow C et al (2019) Multidimensional vertebral endplate defects are associated with disc degeneration, modic changes, facet joint abnormalities, and pain. J Orthop Res 37:1080–1089. https://doi.org/10.1002/jor.24195
Yin R, Lord EL, Cohen JR et al (2015) Distribution of Schmorl nodes in the lumbar spine and their relationship with lumbar disk degeneration and range of motion. Spine (Phila Pa 1976) 40:E49–E53. https://doi.org/10.1097/BRS.0000000000000658
Tomaszewski KA, Adamek D, Konopka T et al (2015) Endplate calcification and cervical intervertebral disc degeneration: the role of endplate marrow contact channel occlusion. Folia Morphol 74:84–92. https://doi.org/10.5603/FM.2015.0014
Boos N, Weissbach S, Rohrbach H et al (2002) Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo award in basic science. (Phila Pa 1976) 27:2631–2644. https://doi.org/10.1097/00007632-200212010-00002
Resnick DNG (1978) Intravertebral disk herniations: cartilaginous (Schmorl’s) nodes. Radiology 126:57–65
Inaoka M, Yamazaki Y, Hosono N et al (2000) Radiographic analysis of lumbar spine for low-back pain in the general population. Arch Orthop Trauma Surg 120:380–385
Acknowledgements
The authors thank Dianne Bryant for her review and critical comments, which improved the manuscript, Zakari Crites Videman for his assistance in the article selection and inclusion process and Meagan Stanley for her assistance towards developing the search strategy.
Funding
No specific funding was received for this project. However, Aliyu Lawan, as a graduate student, receives support from the Faculty of Health Sciences and a Transdisciplinary Training Award from the Bone and Joint Institute at Western University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lawan, A., Leung, A. & Battié, M.C. Vertebral endplate defects: nomenclature, classification and measurement methods: a scoping review. Eur Spine J 29, 1397–1409 (2020). https://doi.org/10.1007/s00586-020-06378-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06378-8