Abstract
Purpose
To assess outcomes and predictors of early and long-term remission in patients with Cushing’s disease (CD) due to ACTH-secreting adenomas treated via endoscopic endonasal approach (EEA).
Methods
This is a retrospective study. Consecutive patients operated for CD from 1998 to 2017 in an Italian referral Pituitary Center were enrolled. Clinical, radiological, and histological data at enrollment and follow-up were collected.
Results
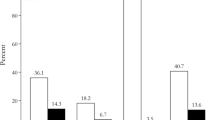
151 patients (107 F) were included; 88.7% were naïve for treatment, 11.3% had been treated surgically and 11.2% medically. At pre-operative magnetic resonance imaging (MRI), 35 had a macroadenoma and 80 a microadenoma, while tumor was undetectable in 36 patients. Mean age at surgery was 41.1 ± 16.6 years. Diagnosis was confirmed histologically in 82.4% of the cases. Patients with disease persistence underwent second surgery and/or medical and/or radiation therapy. Mean follow-up was 92.3 ± 12.0 (range 12–237.4) and median 88.2 months. Remission rate was 88.1% after the first surgery and 90.7% at last follow-up. One patient died of pituitary carcinoma. Post-surgical cortisol drop (p = 0.004), tumor detection at MRI (p = 0.03) and size < 1 cm (p = 0.045) increased the chance of disease remission; cavernous sinus invasion was a negative predictor of outcome (p = 0.002). Twenty-seven patients developed diabetes insipidus and 18 hypopituitarism. Surgery repetition increased the risk of hypopituitarism (p = 0.03), but not of other complications, which included epistaxis (N = 2), cerebrospinal fluid leakage (1), pneumonia (3), myocardial infarction (1), and pulmonary embolisms (2).
Conclusions
Selective adenomectomy via EEA performed by experienced surgeons, supported by a multidisciplinary dedicated team, allows long-term remission in the vast majority of CD patients with low complication rate.

Similar content being viewed by others
References
Guaraldi F, Salvatori R (2012) Cushing syndrome: maybe not so uncommon of an endocrine disease. J Am Board Fam Med 25:199–208
Lonser RR, Nieman L, Oldfield EH (2018) Cushing’s disease: pathobiology, diagnosis, and management. J Neurosurg 126:404–417
Biller BM, Grossman AB, Stewart PM et al (2008) Treatment of adrenocorticotropin-dependent Cushing’s syndrome: a consensus statement. J Clin Endocrinol Metab 93:2454–2462
Wagenmakers MA, Boogaarts HD, Roerink SH et al (2013) Endoscopic transsphenoidal pituitary surgery: a good and safe primary treatment option for Cushing's disease, even in case of macroadenomas or invasive adenomas. Eur J Endocrinol 169:329–337
Smith TR, Holou MM, Huang KT et al (2015) Complications after transsphenoidal surgery for patients with Cushing’s disease and silent corticotroph adenomas. Neurosurg Focus 38:E12
Johnston PC, Kennedy L, Hamrahian AH et al (2017) Surgical outcomes in patients with Cushing's disease: the Cleveland clinic experience. Pituitary 20:430–440
Nieman LK, Biller BM, Findling JW et al (2015) Endocrine society: treatment of Cushing's syndrome: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 100:2807–2831
Nieman LK, Biller BM, Findling JW et al (2008) The diagnosis of Cushing's syndrome: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 93:1526–1540
Wilson CB (1984) A decade of pituitary microsurgery. The Herbert Olivecrona lecture. J Neurosurg 61:814–833
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space. A magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33:610–617
Zoli M, Milanese L, Bonfatti R et al (2016) Cavernous sinus invasion by pituitary adenomas: role of endoscopic endonasal surgery. J Neurosurg Sci 60:485–494
Frank G, Pasquini E, Farneti G et al (2006) The endoscopic versus the traditional approach in pituitary surgery. Neuroendocrinology 83:240–248
Frank G, Pasquini E (2006) Endoscopic endonasal cavernous sinus surgery, with special reference to pituitary adenomas. Front Horm Res 34:64–82
Zoli M, Marucci G, Milanese L et al (2016) Suction filter in endoscopic endonasal surgery: a technical note. World Neurosurg 95:464–468
Barazi SA, Pasquini E, D'Urso PI et al (2013) Extended endoscopic transplanum-transtuberculum approach for pituitary adenomas. Br J Neurosurg 27:374–382
Oldfield EH, Vortmeyer AO (2006) Development of a histological pseudocapsule and its use as a surgical capsule in the excision of pituitary tumors. J Neurosurg 104:7–19
Osamura RY, Grossman A, Korbonits M et al (2017) Pituitary adenoma. In: Lloyd RV, Osamura RY, Kloppel G, Rosai J (eds) World Health Organization classification of tumours of endocrine organs, 4th edn. IARC, Lyon, pp 14–18
Fleseriu M, Hashim IA, Karavitaki N et al (2016) Hormonal replacement in hypopituitarism in adults: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 101:3888–3921
Hameed N, Yedinak CG, Brzana J et al (2013) Remission rate after transsphenoidal surgery in patients with pathologically confirmed Cushing's disease, the role of cortisol, ACTH assessment and immediate reoperation: a large single center experience. Pituitary 16:452–458
Schwartz TH, Morgenstern PF, Anand VK (2019) Lessons learned in the evolution of endoscopic skull base surgery. J Neurosurg 130:337–346
Broersen LHA, Biermasz NR, van Furth WR et al (2018) Endoscopic vs. microscopic transsphenoidal surgery for Cushing's disease: a systematic review and meta-analysis. Pituitary 21:524–534
Qiao N (2018) Outcome of endoscopic vs microsurgical transsphenoidal resection for Cushing’s disease. Endocr Connect 7:R26–R37
Berker M, Isikay I, Berker D, Bayraktar M, Gurlek A (2014) Early promising results for the endoscopic surgical treatment of Cushing’s disease. Neurosurg Rev 37:105–114
Atkinson AB, Kennedy A, Wiggam MI, McCance DR, Sheridan B (2005) Long-term remission rates after pituitary surgery for Cushing’s disease: the need for long-term surveillance. Clin Endocrinol 63:549–559
Alahmadi H, Cusimano MD, Woo K et al (2013) Impact of technique on Cushing disease outcome using strict remission criteria. Can J Neurol Sci 40:334–341
Cebula H, Baussart B, Villa C et al (2017) Efficacy of endoscopic endonasal transsphenoidal surgery for Cushing's disease in 230 patients with positive and negative MRI. Acta Neurochir (Wien) 159:1227–1236
Dehdashti AR, Gentili F (2007) Current state of the art in the diagnosis and surgical treatment of Cushing disease: early experience with a purely endoscopic endonasal technique. Neurosurg Focus 23:E9
Kuo CH, Yen YS, Wu JC, Chen YC, Huang WC, Cheng H (2015) Primary endoscopic transnasal transsphenoidal surgery for magnetic resonance image-positive cushing disease: outcomes of a series over 14 years. World Neurosurg 84:772–779
Netea-Maier RT, van Lindert EJ, den Heijer M et al (2006) Transsphenoidal pituitary surgery via the endoscopic technique: results in 35 consecutive patients with Cushing's disease. Eur J Endocrinol 154:675–684
Sarkar S, Rajaratnam S, Chacko G, Mani S, Hesargatta AS, Chacko AG (2016) Pure endoscopic transsphenoidal surgery for functional pituitary adenomas: outcomes with Cushing's disease. Acta Neurochir (Wien) 158:77–86
Shin SS, Gardner PA, Ng J et al (2017) Endoscopic endonasal approach for adrenocorticotropic hormone-secreting pituitary adenomas: outcomes and analysis of remission rates and tumor biochemical activity with respect to tumor invasiveness. World Neurosurg 102:651–658
Starke RM, Reames DL, Chen CJ, Laws ER, Jane JAJR (2013) Endoscopic transsphenoidal surgery for Cushing disease: techniques, outcomes, and predictors of remission. Neurosurgery 72:240–247
Casanueva FF, Barkan AL, Buchfelder M et al (2017) Pituitary society, expert group on pituitary tumors. Criteria for the definition of pituitary tumor centers of excellence (PTCOE): a pituitary society statement. Pituitary 20:489–498
Dickerman RD, Oldfield EH (2002) Basis of persistent and re- current Cushing disease: an analysis of findings at repeated pituitary surgery. J Neurosurg 97:1343–1349
Lobatto DJ, de Vries F, Zamanipoor Najafabadi AH et al (2018) Preoperative risk factors for postoperative complications in endoscopic pituitary surgery: a systematic review. Pituitary 21:84–97
Acknowledgements
We thank Dr. Giorgio Frank for his fundamental clinical and scientific support over the past 20 years. The study received no financial support.
Funding
The authors declare that the study has received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the inter-hospital Ethical Committee of Bologna City (Protocol No. CE17143, February 2018) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All patients gave written informed consent after detailed explanation of the study purpose and procedures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Guaraldi, F., Zoli, M., Asioli, S. et al. Results and predictors of outcome of endoscopic endonasal surgery in Cushing’s disease: 20-year experience of an Italian referral Pituitary Center. J Endocrinol Invest 43, 1463–1471 (2020). https://doi.org/10.1007/s40618-020-01225-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01225-5