Abstract
Objective
Assess impact of parental involvement in care provision for term substance exposed newborns (SENs).
Study design
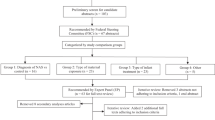
Prospective observational cohort study included mothers with opioid use disorder and their SENs over 4 year study period. Maternal–Infant dyads enrolled in EMPOWER and rooming-in (RI) programs were included and received care 24/7 in a private room until newborn’s discharge. Outcomes were compared for dyads participating in EMPOWER/RI with historical controls.
Results
Ninety of 156 historical SENs were RI eligible, while 49 of 108 SENs born during RI period had mothers enrolled in EMPOWER. EMPOWER/RI SENs had lower rates for and duration of pharmacotherapy, shorter neonatal intensive care unit (NICU) and hospital lengths of stay. EMPOWER/RI increased initiation and continuation of breastfeeding at discharge.
Conclusions
Parental participation was associated with a decrease in initiation and duration of pharmacotherapy, NICU admission, length of stay and hospital charges while increasing breastfeeding initiation and continuation at discharge.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder doumented at delivery hospitalization – United States, 1999–2014. MMWR Morb Mortal Wkly Rep. 2018;67:845–9.
Patrick SW, Shumacher RE, Benneyworth BD, Kranz EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000–9. JAMA. 2012;307:1934–40.
Kocherlakota P. Neonatal abstinence syndrome. Am Acad Pediatrics. 2014;134:e547–e561.
Wachman EM, Warden AH, Thomas Z, Thomas-Lewis JA, Shrestha H, Nikita FN, et al. Impact of psychiatric medication co-exposure on Neonatal Abstinence Syndrome severity. Drug Alcohol Depend. 2018;192:45–50.
Oei JL, Melhuish E, Uebel H, Azzam N, Breen C, Burns L, et al. Neonatal abstinence syndrome and high school performance. Pediatrics. 2017;139:e20162651.
Fill MMA, Miller AM, Wilkinson RH, Warren M, Dunn J, Schaffner W, et al. Educational disabilities among children born with neonatal abstinence syndrome. Pediatrics. 2018;142:e20180562.
Vela RM. The effect of severe stress on early brain development, attachment, and emotions: a psychoanatomical formulation. Psychiatr Clin North Am. 2014;37:519–34.
Abrahams RR, Kelly SA, Payne S, Thiessen PN, Mackintosh J, Janssen PA. Rooming-in compared with standard care for newborns of mothers using methadone or heroin. Can Fam Phys. 2007;53:1722–30.
McCarthy JJ, Leamon MH, Finnegan LP, Fassbender C. Opioid dependence and pregnancy: minimizing stress on the fetal brain. Am J Obstet Gynecol. 2017;216:226–31.
Krans EE, Patrick SW. Opioid use disorder in pregnancy: health policy and practice in the midst of an epidemic. Obstet Gynecol. 2016;128:4–10.
Stone R. Pregnant women and substance use: fear, stigma, and barriers to care. Health Justice. 2015;3:2.12.
Lopian KM, Chebolu E, Kulak JA, Kahn LS, Blondell RD. A retrospective analysis of treatment and retention outcomes of pregnant and/or parenting women with opioid use disorder. J Subst Abus Treat. 2019;97:1–6.
Watson C, Mallory A, Crossland A. The spiritual and ethical implications of medication-assisted recovery in pregnancy: preserving the dignity and worth of mother and baby. Soc Work Christianity. 2019;46:66–86.
Krans EE, Bobby S, England M, Gedekoh RH, Chang JC, Maguire B, et al. The pregnancy recovery center: a women-centered treatment program for pregnant and postpartum women with opioid use disorder. Addict Behav 2018;86:124–9.
https://www.cdc.gov/healthliteracy/learn/index.html. Accessed 23 Nov 2019.
Heijmans M, Waverijn G, Rademakers J, van der Vaart R, Rijken M. Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management. Patient Educ Couns. 2015;98:41–8.
Harrington KF, Zhang B, Magruder T, Bailey WC, Gerald LB. The impact of parent’s health literacy on pediatric asthma outcomes. Pediatr Allergy Immunol Pulmonol. 2015;28:20–6.
Kale MS, Federman AD, Krauskopf K, Wolf M, O’Conor R, Martynenko M, et al. The association of health literacy with illness and medication beliefs among patients with chronic obstructive pulmonary disease. PloS ONE. 2015;10:e0123937.
Devraj R, Borrego M, Vilay AM, Gordon EJ, Pailden J, Horowitz B. Relationship between health literacy and kidney function. Nephrology. 2015;20:360–7.
Holmes AV, Atwood EC, Whalen B, Beliveau J, Jarvis JD, Matulis JC, et al. Rooming-in to treat neonatal abstinence syndrome: improved family-centered care at lower cost. Pediatrics. 2016;137:e20152929.
McQueen KA. ‘Rooming-in’ could be an effective non-pharmacological treatment for infants with neonatal abstinence syndrome. Evid Based Nurs. 2018;21110.
Grossman MR, Berkwitt AK, Osborn RR, Xu Y, Esserman DA, Shapiro ED, et al. An initiative to improve the quality of care of infants with neonatal abstinence syndrome. Pediatrics. 2017;139:e20163360.
Holmes AV. Rooming-in reduces costs of neonatal abstinence syndrome. Pharmacoecon Outcomes N. 2016;755:34–18.
Blount T, Painter A, Freeman E, Grossman M, Sutton AG. Reduction in length of stay and morphine use for NAS with the “eat, sleep, console” method. Hosp Pediatr. 2019;9:615–23.
Grisham LM, Stephen MM, Coykendall MR, Kane MF, Maurer JA, Bader MY. Eat, sleep, console approach: a family-centered model for the treatment of neonatal abstinence syndrome. Adv Neonatal Care. 2019;19:138–44.
Tilberg AD. Implementing the eat, sleep, console approach for NAS management: review of literature. Doctor of nursing practice (DNP) practice innovation projects. 125. 2019. https://openprairie.sdstate.edu/con_dnp/125.
Minear S, Wachman EM. Management of newborns with prenatal opioid exposure: one institution’s journey. Clin Ther 2019;41:1663–8.
Jansson LM, Velez ML. Optimal care for NAS: are we moving in the wrong direction? Hosp Pediatr. 2019;9:655–8.
Acknowledgements
The authors gratefully acknowledge the contributions of their subjects, and their subjects’ families, as well as those of their colleagues. In addition, we would like to acknowledge Dr Daniel Grow, Ms Annery Brown, Ms Linda Jablonski, Ms Nancy Rines, Ms Michelle Nicoli, Ms Sheila Foss, Ms Emily Lajeunesse, Ms Katiria Moran, Ms Sarah Crawford, Ms Donna Stafilarakis and entire OB nursing staff. Without their support the program could not have achieved the success it did.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, R., Rothstein, R., Ricci, K. et al. Partnering with parents to improve outcomes for substance exposed newborns—a pilot program. J Perinatol 40, 1041–1049 (2020). https://doi.org/10.1038/s41372-020-0662-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0662-9
This article is cited by
-
Short term outcomes of neonatal opioid withdrawal syndrome: a comparison of two approaches
Journal of Perinatology (2024)
-
The impact of antenatal cannabis use on the neonate: Time for open engagement?
Pediatric Research (2021)
-
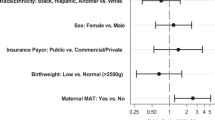
Predictors of pharmacologic therapy for neonatal opioid withdrawal syndrome: a retrospective analysis of a statewide database
Journal of Perinatology (2021)