Abstract
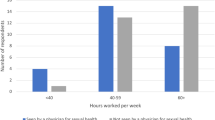
Men’s Health is a urological subspecialty that is at the forefront of innovation, but little data exist evaluating the attitudes that andrologists have toward the current treatment modalities available for managing Men’s Health conditions. A survey of 37 questions asking what providers would choose as treatment for common conditions was distributed online via Survey Monkey to members of the Sexual Medicine Society of North America and European Society for Sexual Medicine. A total of 115 respondents completed the survey after an initial screening question. For erectile dysfunction (ED), 40%, 38%, and 33% of providers indicated that they would use tadalafil daily, tadalafil on demand, or sildenafil on demand, respectively, as first-line phosphodiesterase 5 inhibitor therapy. Furthermore, a total of 74% would elect to undergo low-intensity shockwave therapy [67%], platelet rich plasma injections [15%], and stem cell injections [15%]. Sex/behavioral therapy was preferred for both premature (36%) and delayed (52%) ejaculation. Approximately 44% of respondents indicated that they would undergo Collagenase Clostridium Histolyticum injections for Peyronie’s Disease in the acute phase. In the setting of hypogonadal symptoms with borderline low total testosterone levels (300–400 ng/dL), 69% of respondents would pursue testosterone therapy. The prostatic lift procedure was the preferred procedure for men seeking symptom resolution with preservation of ejaculatory function. Many Men’s Health specialists would pursue the least invasive options before considering procedural intervention for any given condition. Providers may shift their treatment preferences toward newer treatment modalities as longer term data become available.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Change history
09 April 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41443-020-0266-0
References
Smith JA, Robertson S. Men’s health promotion: a new frontier in Australia and the UK? Health Promot Int. 2008;23:283–9.
Bhasin S. A perspective on the evolving landscape in male reproductive medicine. J Clin Endocrinol Metab. 2016;101:827–36.
Robertson S. Understanding men and health: masculinities, identity and well-being. UK: McGraw-Hill Education; 2007.
Sotomayor M. The burden of premature ejaculation: the patient’s perspective. J Sex Med. 2005;2:110–4.
Rosen R, Catania J, Lue T, Althof S, Henne J, Hellstrom W, et al. Impact of Peyronie’s disease on sexual and psychosocial functioning: qualitative findings in patients and controls. J Sex Med. 2008;5:1977–84.
Schnetzler G, Banks I, Kirby M, Zou KH, Symonds T. Characteristics, behaviors, and attitudes of men bypassing the healthcare system when obtaining phosphodiesterase type 5 inhibitors. J Sex Med. 2010;7:1237–46.
Chiang J, Yafi FA, Dorsey PJ Jr, Hellstrom WJ. The dangers of sexual enhancement supplements and counterfeit drugs to “treat” erectile dysfunction. Transl Androl Urol. 2017;6:12.
Serefoglu EC, Hellstrom WJ. Treatment of Peyronie’s disease: 2012 update. Curr Urol Rep. 2011;12:444–52.
Anaissie J, Yafi FA. A review of surgical strategies for penile prosthesis implantation in patients with Peyronie’s disease. Transl Androl Urol. 2016;5:342.
Goldstein I, Lue TF, Padma-Nathan H, Rosen RC, Steers WD, Wicker PA. Oral sildenafil in the treatment of erectile dysfunction. N. Engl J Med. 1998;338:1397–404.
Porst H, Rosen R, Padma-Nathan H, Goldstein I, Giuliano F, Ulbrich E. The efficacy and tolerability of vardenafil, a new, oral, selective phosphodiesterase type 5 inhibitor, in patients with erectile dysfunction: the first at-home clinical trial. Int J Impot Res. 2001;13:192.
Brock GB, McMahon CG, Chen KK, Costigan T, Shen W, Watkins V, et al. Efficacy and safety of tadalafil for the treatment of erectile dysfunction: results of integrated analyses. J Urol. 2002;168:1332–6.
Berkseth KE, Thirumalai A, Amory JK. Pharmacologic therapy in men’s health: hypogonadism, erectile dysfunction, and benign prostatic hyperplasia. Med Clin. 2016;100:791–805.
Francis SH, Corbin JD. Molecular mechanisms and pharmacokinetics of phosphodiesterase-5 antagonists. Curr Urol Rep. 2003;4:457–65.
Kitrey ND, Gruenwald I, Appel B, Shechter A, Massarwa O, Vardi Y. Penile low intensity shock wave treatment is able to shift PDE5i nonresponders to responders: a double-blind, Sham Controlled Study. J Urol. 2016;195:1550–5.
Sokolakis I, Hatzichristodoulou G. Clinical studies on low intensity extracorporeal shockwave therapy for erectile dysfunction: a systematic review and meta-analysis of randomised controlled trials. Int J Impot Res. 2019;31:177–94.
Campbell JD, Trock BJ, Oppenheim AR, Anusionwu I, Gor RA, Burnett AL. Meta-analysis of randomized controlled trials that assess the efficacy of low-intensity shockwave therapy for the treatment of erectile dysfunction. Therapeutic Adv Urol. 2019;11:1756287219838364.
Capogrosso P, Frey A, Jensen CF, Rastrelli G, Russo GI, Torremade J, et al. Low-intensity shock wave therapy in sexual medicine—clinical recommendations from the European Society of Sexual Medicine (ESSM). J Sex Med. 2019;16:1490–505.
Peak TC, Anaissie J, Hellstrom WJ. Current perspectives on stem cell therapy for erectile dysfunction. Sex Med Rev. 2016;4:247–56.
Scott S, Roberts M, Chung E. Platelet-rich plasma and treatment of erectile dysfunction: Critical review of literature and global trends in platelet-rich plasma clinics. Sex Med Rev. 2019;7:306–12.
Sexual Medicine Society of North America. Position statement: ED restorative (regenerative) therapies; 2019. http://www.smsna.org/V1/news/433-smsna-position-statement-on-restorative-therapies-for-ed.
Shindel A, Nelson C, Brandes S. Urologist practice patterns in the management of premature ejaculation: a nationwide survey. J Sex Med. 2008;5:199–205.
Nguyen HM, Anaissie J, DeLay KJ, Yafi FA, Sikka SC, Hellstrom WJ. Safety and efficacy of collagenase Clostridium histolyticum in the treatment of acute-phase Peyronie’s disease. J Sex Med. 2017;14:1220–5.
Yang KK, Bennett N. Peyronie’s disease and injectable collagenase clostridium histolyticum: safety, efficacy, and improvements in subjective symptoms. Urology. 2016;94:143–7.
Anaissie J, Yafi FA, DeLay KJ, Traore EJ, Sikka SC, Hellstrom WJ. Impact of number of cycles of collagenase Clostridium histolyticum on outcomes in patients with Peyronie’s disease. Urology. 2017;100:125–30.
Shindel AW, Bullock TL, Brandes S. Urologist practice patterns in the management of Peyronie’s disease: a nationwide survey. J Sex Med. 2008;5:954–64.
Nehra A, Alterowitz R, Culkin DJ, Faraday MM, Hakim LS, Heidelbaugh JJ, et al. Peyronie’s disease: AUA guideline. J Urol. 2015;194:745–53.
Corona G, Maseroli E, Rastrelli G, Isidori AM, Sforza A, Mannucci E, et al. Cardiovascular risk associated with testosterone-boosting medications: a systematic review and meta-analysis. Expert Opin Drug Saf. 2014;13:1327–51.
Pastuszak AW, Rodriguez KM, Nguyen TM, Khera M. Testosterone therapy and prostate cancer. Transl Androl Urol. 2016;5:909.
Mulhall JP, Trost LW, Brannigan RE, Kurtz EG, Redmon JB, Chiles KA, et al. Evaluation and management of testosterone deficiency: AUA guideline. J Urol. 2018;200:423–32.
Bautista OM, Kusek JW, Nyberg LM Jr, McConnell JD, Bain RP, Miller G, et al. Study design of the Medical Therapy of Prostatic Symptoms (MTOPS) trial. Control Clin Trials. 2003;24:224–43.
Siami P, Roehrborn CG, Barkin J, Damiao R, Wyczolkowski M, Duggan A, et al. Combination therapy with dutasteride and tamsulosin in men with moderate-to-severe benign prostatic hyperplasia and prostate enlargement: the CombAT (Combination of Avodart® and Tamsulosin) trial rationale and study design. Contemp Clin Trials. 2007;28:770–9.
McVary KT, Gange SN, Shore ND, Bolton DM, Cowan BE, Brown BT, et al. Treatment of LUTS secondary to BPH while preserving sexual function: randomized controlled study of prostatic urethral lift. J Sex Med. 2014;11:279–87.
Roehrborn CG, Gange SN, Shore ND, Giddens JL, Bolton DM, Cowan BE, et al. The prostatic urethral lift for the treatment of lower urinary tract symptoms associated with prostate enlargement due to benign prostatic hyperplasia: the LIFT Study. J Urol. 2013;190:2161–7.
Gratzke C, Barber N, Speakman MJ, Berges R, Wetterauer U, Greene D, et al. Prostatic urethral lift vs transurethral resection of the prostate: 2‐year results of the BPH 6 prospective, multicentre, randomized study. BJU Int. 2017;119:767–75.
Green Z, Westwood J, Somani BK. What’s new in Rezum: a transurethral water vapour therapy for BPH. Curr Urol Rep. 2019;20:39.
McVary KT, Rogers T, Roehrborn CG. Rezūm water vapor thermal therapy for lower urinary tract symptoms associated with benign prostatic hyperplasia: 4-year results from randomized controlled study. Urology. 2019;126:171–9.
Gilling PJ, Barber N, Bidair M, Anderson P, Sutton M, Aho T, et al. Randomized controlled trial of aquablation versus transurethral resection of the prostate in benign prostatic hyperplasia: one-year outcomes. Urology. 2019;125:169–73.
Yafi FA, Tallman CT, Seard ML, Jordan ML. Aquablation outcomes for the US cohort of men with LUTS due to BPH in large prostates (80–150 cc). Int J Impot Res. 2018;30:209.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FAY is a consultant for Coloplast. AP is an advisor and speaker for Endo Pharmaceuticals, and received research and fellowship support from this entity. He is also an advisor for Boston Scientific and an advisor for Antares Pharmaceuticals. He is a speaker for Bayer AG. He is the founder of and maintains a leadership role in Woven Health. RC is a consultant for Coloplast, a consultant for Boston Scientific, and a consultant for Endo Pharmaceuticals. All other authors have no conflicts of interest to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Towe, M., El-Khatib, F., Osman, M. et al. “Doc, if it were you, what would you do?”: a survey of Men’s Health specialists’ personal preferences regarding treatment modalities. Int J Impot Res 33, 303–310 (2021). https://doi.org/10.1038/s41443-020-0263-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-0263-3
This article is cited by
-
Current and emerging treatment options for premature ejaculation
Nature Reviews Urology (2022)
-
Low-intensity extracorporeal shockwave therapy among urologist practitioners: how the opinion of urologists changed between 2016 and 2019
International Journal of Impotence Research (2021)