Abstract
Purpose
The aim was to examine changes in the bone-derived hormone lipocalin 2 (LCN2) levels in patients with active acromegaly and to investigate the potential roles of LCN2 and osteocalcin in glucose metabolism.
Methods
We recruited 50 consecutive acromegalic patients. Of those, 39 patients with complete postoperative follow-up data were included. Thirty sex-, age-, and BMI-matched healthy individuals were recruited as normal controls. The pre- and postoperative serum LCN2 and osteocalcin levels were compared. The homeostasis model assessment insulin resistance (HOMA-IR) index and secretion [β-cell function (HOMA-β)] were calculated.
Results
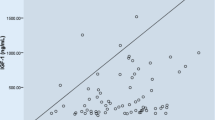
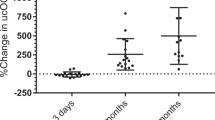
Compared with controls, acromegalic subjects had lower LCN2 levels (34.15 ± 9.95 vs 57.50 ± 29.75 ng/mL, P < 0.01) and higher osteocalcin levels (55.45 ± 34.02 vs 19.46 ± 6.69 ng/mL, P < 0.01). Acromegalic patients also had elevated HOMA-IR levels, and the HOMA-β and the area under the curve for insulin (AUC INS) levels were slightly but nonsignificantly increased. The serum levels of LCN2 significantly increased after surgery (37.03 ± 9.73 vs 45.15 ± 15.33 ng/mL, P < 0.05), and those of osteocalcin significantly decreased [43.51 (26.73–65.66) vs 24.79 (18.39–32.59) ng/mL, P < 0.01]. Total lean mass was the only positive predictor of LCN2, and elevated serum IGF-I was a positive predictor of osteocalcin. Low LCN2 and elevated serum osteocalcin levels were predictors of the AUC INS, and osteocalcin was a positive predictor of HOMA-β.
Conclusion
The bone-derived hormones, osteocalcin and LCN2 changed significantly in active acromegaly, were altered after treatment and served as predictors of β-cell function in acromegaly. This study shows that the bone could be involved in regulating glucose metabolism in acromegaly.

Similar content being viewed by others
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Katznelson L, Laws ER Jr, Melmed S, Molitch ME, Murad MH, Utz A, Wass JA, Endocrine S (2014) Acromegaly: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 99(11):3933–3951. https://doi.org/10.1210/jc.2014-2700
Fieffe S, Morange I, Petrossians P, Chanson P, Rohmer V, Cortet C, Borson-Chazot F, Brue T, Delemer B, French Acromegaly R (2011) Diabetes in acromegaly, prevalence, risk factors, and evolution: data from the French Acromegaly Registry. Eur J Endocrinol 164(6):877–884. https://doi.org/10.1530/EJE-10-1050
Dreval AV, Trigolosova IV, Misnikova IV, Kovalyova YA, Tishenina RS, Barsukov IA, Vinogradova AV, Wolffenbuttel BH (2014) Prevalence of diabetes mellitus in patients with acromegaly. Endocr Connect 3(2):93–98. https://doi.org/10.1530/EC-14-0021
Espinosa-de-los-Monteros AL, Gonzalez B, Vargas G, Sosa E, Mercado M (2011) Clinical and biochemical characteristics of acromegalic patients with different abnormalities in glucose metabolism. Pituitary 14(3):231–235. https://doi.org/10.1007/s11102-010-0284-x
Arosio M, Reimondo G, Malchiodi E, Berchialla P, Borraccino A, De Marinis L, Pivonello R, Grottoli S, Losa M, Cannavo S, Minuto F, Montini M, Bondanelli M, De Menis E, Martini C, Angeletti G, Velardo A, Peri A, Faustini-Fustini M, Tita P, Pigliaru F, Borretta G, Scaroni C, Bazzoni N, Bianchi A, Appetecchia M, Cavagnini F, Lombardi G, Ghigo E, Beck-Peccoz P, Colao A, Terzolo M, Italian Study Group of A (2012) Predictors of morbidity and mortality in acromegaly: an Italian survey. Eur J Endocrinol 167(2):189–198. https://doi.org/10.1530/EJE-12-0084
Frara S, Maffezzoni F, Mazziotti G, Giustina A (2016) Current and emerging aspects of diabetes mellitus in acromegaly. Trends Endocrinol Metab 27(7):470–483. https://doi.org/10.1016/j.tem.2016.04.014
Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, Confavreux C, Dacquin R, Mee PJ, McKee MD, Jung DY, Zhang Z, Kim JK, Mauvais-Jarvis F, Ducy P, Karsenty G (2007) Endocrine regulation of energy metabolism by the skeleton. Cell 130(3):456–469. https://doi.org/10.1016/j.cell.2007.05.047
Mazziotti G, Biagioli E, Maffezzoni F, Spinello M, Serra V, Maroldi R, Floriani I, Giustina A (2015) Bone turnover, bone mineral density, and fracture risk in acromegaly: a meta-analysis. J Clin Endocrinol Metab 100(2):384–394. https://doi.org/10.1210/jc.2014-2937
Constantin T, Tangpricha V, Shah R, Oyesiku NM, Ioachimescu OC, Ritchie J, Ioachimescu AG (2017) Calcium and bone turnover markers in acromegaly: a prospective, controlled study. J Clin Endocrinol Metab 102(7):2416–2424. https://doi.org/10.1210/jc.2016-3693
Karsenty G, Olson EN (2016) Bone and muscle endocrine functions: unexpected paradigms of inter-organ communication. Cell 164(6):1248–1256. https://doi.org/10.1016/j.cell.2016.02.043
Han Y, You X, Xing W, Zhang Z, Zou W (2018) Paracrine and endocrine actions of bone-the functions of secretory proteins from osteoblasts, osteocytes, and osteoclasts. Bone Res 6:16. https://doi.org/10.1038/s41413-018-0019-6
Moschen AR, Adolph TE, Gerner RR, Wieser V, Tilg H (2017) Lipocalin-2: a master mediator of intestinal and metabolic inflammation. Trends Endocrinol Metab 28(5):388–397. https://doi.org/10.1016/j.tem.2017.01.003
Mosialou I, Shikhel S, Liu JM, Maurizi A, Luo N, He Z, Huang Y, Zong H, Friedman RA, Barasch J, Lanzano P, Deng L, Leibel RL, Rubin M, Nickolas T, Chung W, Zeltser LM, Williams KW, Pessin JE, Kousteni S (2017) MC4R-dependent suppression of appetite by bone-derived lipocalin 2. Nature 543(7645):385–390. https://doi.org/10.1038/nature21697
Bi Y, Zeng L, Zhu D, Yan J, Zhang Y, Tong G, Mu P, Shen S, Hu Y, Yu Q, Liang H, Weng J (2012) Association of beta-cell function and insulin sensitivity with fasting and 2-h plasma glucose in a large Chinese population. Diabetes Obes Metab 14(2):174–180. https://doi.org/10.1111/j.1463-1326.2011.01504.x
Yang W, Liu J, Shan Z, Tian H, Zhou Z, Ji Q, Weng J, Jia W, Lu J, Liu J, Xu Y, Yang Z, Chen W (2014) Acarbose compared with metformin as initial therapy in patients with newly diagnosed type 2 diabetes: an open-label, non-inferiority randomised trial. Lancet Diabetes Endocrinol 2(1):46–55. https://doi.org/10.1016/S2213-8587(13)70021-4
Sucunza N, Barahona MJ, Resmini E, Fernandez-Real JM, Ricart W, Farrerons J, Rodriguez Espinosa J, Marin AM, Puig T, Webb SM (2009) A link between bone mineral density and serum adiponectin and visfatin levels in acromegaly. J Clin Endocrinol Metab 94(10):3889–3896. https://doi.org/10.1210/jc.2009-0474
Olarescu NC, Bollerslev J (2016) The impact of adipose tissue on insulin resistance in acromegaly. Trends Endocrinol Metab 27(4):226–237. https://doi.org/10.1016/j.tem.2016.02.005
Kasayama S, Otsuki M, Takagi M, Saito H, Sumitani S, Kouhara H, Koga M, Saitoh Y, Ohnishi T, Arita N (2000) Impaired beta-cell function in the presence of reduced insulin sensitivity determines glucose tolerance status in acromegalic patients. Clin Endocrinol (Oxf) 52(5):549–555
Niculescu D, Purice M, Coculescu M (2013) Insulin-like growth factor-I correlates more closely than growth hormone with insulin resistance and glucose intolerance in patients with acromegaly. Pituitary 16(2):168–174. https://doi.org/10.1007/s11102-012-0396-6
Ueland T, Fougner SL, Godang K, Lekva T, Schurgers LJ, Scholz H, Halvorsen B, Schreiner T, Aukrust P, Bollerslev J (2010) Associations between body composition, circulating interleukin-1 receptor antagonist, osteocalcin, and insulin metabolism in active acromegaly. J Clin Endocrinol Metab 95(1):361–368. https://doi.org/10.1210/jc.2009-0422
Sabek OM, Nishimoto SK, Fraga D, Tejpal N, Ricordi C, Gaber AO (2015) Osteocalcin effect on human beta-cells mass and function. Endocrinology 156(9):3137–3146. https://doi.org/10.1210/EN.2015-1143
Booth SL, Centi A, Smith SR, Gundberg C (2013) The role of osteocalcin in human glucose metabolism: marker or mediator? Nat Rev Endocrinol 9(1):43–55. https://doi.org/10.1038/nrendo.2012.201
De la Chesnaye E, Manuel-Apolinar L, Zarate A, Damasio L, Espino N, Revilla-Monsalve MC, Islas-Andrade S (2015) Lipocalin-2 plasmatic levels are reduced in patients with long-term type 2 diabetes mellitus. Int J Clin Exp Med 8(2):2853–2859
Wu C, Wang Q, Lv C, Qin N, Lei S, Yuan Q, Wang G (2014) The changes of serum sKlotho and NGAL levels and their correlation in type 2 diabetes mellitus patients with different stages of urinary albumin. Diabetes Res Clin Pract 106(2):343–350. https://doi.org/10.1016/j.diabres.2014.08.026
Lou Y, Wu C, Wu M, Xie C, Ren L (2014) The changes of neutrophil gelatinase-associated lipocalin in plasma and its expression in adipose tissue in pregnant women with gestational diabetes. Diabetes Res Clin Pract 104(1):136–142. https://doi.org/10.1016/j.diabres.2014.01.014
Chang SY, Kim DB, Ko SH, Jang HJ, Jo YH, Kim MJ (2016) The level of nitric oxide regulates lipocalin-2 expression under inflammatory condition in RINm5F beta-cells. Biochem Biophys Res Commun 476(1):7–14. https://doi.org/10.1016/j.bbrc.2016.05.110
Rashad NM, El-Shal AS, Etewa RL, Wadea FM (2017) Lipocalin-2 expression and serum levels as early predictors of type 2 diabetes mellitus in obese women. IUBMB Life 69(2):88–97. https://doi.org/10.1002/iub.1594
Bredella MA, Schorr M, Dichtel LE, Gerweck AV, Young BJ, Woodmansee WW, Swearingen B, Miller KK (2017) Body composition and ectopic lipid changes with biochemical control of acromegaly. J Clin Endocrinol Metab 102(11):4218–4225. https://doi.org/10.1210/jc.2017-01210
Funding
This work was supported by the National Natural Science Foundation (Grant Number 81970689), the Natural Science Foundation of Jiangsu Province (Grant Number BK20181116) and the Project of Jiangsu Provincial Medical Youth Talent.
Author information
Authors and Affiliations
Contributions
LP supervised the project and approved the final version of the manuscript to be submitted. ZY, LMS, and CH designed the research; ZKY and FWH performed all patient selection and data collection processes; ZY drafted the initial manuscript; and LP and ZDL critically revised the manuscript. All of the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
All procedures were performed in accordance with the principles of the Declaration of Helsinki and institutional guidelines. The study was approved by the Ethics Review Committee of Nanjing Drum Tower Hospital Affiliated to Nanjing University Medical School.
Research involving human participants and/or animals
This article does not contain any studies with animals performed by any of the authors.
Informed consent
All patients provided written informed consent to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, Y., Liu, M., Chen, H. et al. Associations between circulating bone-derived hormones lipocalin 2, osteocalcin, and glucose metabolism in acromegaly. J Endocrinol Invest 43, 1309–1316 (2020). https://doi.org/10.1007/s40618-020-01221-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01221-9